INTRODUCTION
The occurrence of overweight/obesity in people with epilepsy is higher when compared to the general population (1-3) and is associated with clinical variables of epilepsy, neuroendocrine factors, and less regular physical activity (4,5). However, other studies describe different results (4).
Overweight/obesity is a chronic inflammatory state of multifactorial etiology and affects multiple systems and organs, being a risk factor for cognitive impairment. Population studies describe a higher risk of cognitive decline and the development of dementia in elderly people with central obesity and worse performance on tests of memory and executive function in obese adults (6-8).
In epilepsy, the impact of obesity on cognitive function has been poorly described. Baxendale et al. described a small but significant variation in intellectual function and memory in 81 obese individuals with epilepsy (9). In a previous study in which 30 elderly people with recent-onset epilepsy were assessed, it was observed that the worst cognitive performance was associated with the presence of central obesity and the best performance in memory was related to lower adiposity (10).
Epilepsy is a disorder of neural networks that can affect cognition, and cognitive impairments may be present at the beginning of the disease or appear in the course of chronic epilepsy (11,12). However, there are still gaps in the knowledge of the possible relationships between the impairment of cognitive functions and the occurrence of obesity in epilepsy. Thus, the study hypothesis is that overweight/obesity in chronic epilepsy is associated with clinical and cognitive variables.
The aim of this study was to assess the occurrence of overweight/obesity in adults with epilepsy and to relate it to cognitive aspects and clinical variables.
METHODOLOGY
This cross-sectional study involved adults diagnosed with epilepsy treated at the clinical neurology outpatient clinic of University Hospital of the Pontifical Catholic University of Campinas, in the city of Campinas, Brazil. Data were collected between December 2019 and December 2021. Epilepsy was diagnosed according to the International Classification of Epilepsies and Epileptic Syndromes (ILAE) (13) criteria. The sample consisted of individuals of both genders, aged over 18 years, and having received treatment with antiseizure medications (ASMs) for at least two years.
Cases with severe cardiovascular and psychiatric disorders, those with progressive neurological diseases and malignant neoplasms, patients who had previously undergone bariatric surgery, and women who were pregnant or lactating at the time of the study were excluded.
A control group was composed of individuals of the same age group and without neurological or psychiatric diseases, preferably among people accompanying patients at the hospital's outpatient clinics.
The Human research ethics committee of the PUC-Campinas approved the research (CAAE: 22510773249517300005481; nº 300005481; 31/08/2017). The individuals were informed of the research protocol and those who agreed to participate signed the free and informed consent form. All assessments were performed individually in a room at the neurological clinic of a hospital.
The participants underwent the following neuropsychological tests:
− Questionnaire with demographic data (age, educational level, and gender) and clinical variables (age at the first seizure, type and frequency of seizures, and antiseizure medications (ASMs) in use). Imaging and EEG data were obtained from hospital charts. Uncontrolled seizures in the last year and the use of an appropriate therapeutic regimen in the last two years were used as criteria for drug-resistant epilepsy.
− Assessment of anthropometric indicators: measurements of waist circumference, right calf circumference, and right arm circumference using a 2-meter tape measure (Sanny Medical SN-4011). Body mass index (BMI) was assessed by dividing weight (in kilograms) by height (in square meters). Overweight was defined as a BMI > 25 to 29.9 kg/m2 and obesity as a BMI ≥ 30 kg/m2 (14).
− Mini-Mental State Examination (MMSE) (15,16); Brief Cognitive Battery-Edu (BCB-Edu): battery consisting of 10 pictures that assesses identification, naming, incidental, immediate, delay recall and recognition. The BCB-Edu also includes the semantic (animal pictures) verbal fluency test (SVF) and the clock drawing test (17).
DATA ANALYSIS
Anthropometric measurements were related to clinical variables and cognitive assessment data (MMSE and BCB-Edu) of adults with epilepsy. Cognitive and anthropometric data from these adults with epilepsy were compared with those obtained from individuals in the control group.
With the data from the cognitive assessment, two groups were formed: a group of adults with epilepsy without or minimally compromised cognitive impairment and another group composed of adults with epilepsy who presented impairment in multiple domains (memory, language, and attention).
Categorical variables were presented as frequencies and percentages, while continuous variables were expressed as means and standard deviations. The chi-square test was used to assess associations between categorical variables, while Student's t-test was used to compare group means. As the cognitive assessment variables did not show a normal distribution, they were transformed into ranks for the nonparametric assessment in the linear regression model.
To assess factors related to cognitive aspects, linear logistic regression and multiple logistic models were used, with stepwise variable selection criteria according to the Akaike Information Criterion (AIC). In linear regression, cognitive aspects were transformed into ranks.
The Statistical Packages for Social Sciences, version 22 was used for statistical analysis. Statistical significance was set to a p-value lower than 0.05.
RESULTS
In this study, 164 adults with epilepsy and 71 subjects were included for the composition of the control group. There was no significant difference in age, educational level, occupation, and gender between the groups.
Adults with epilepsy performed worse in several cognitive areas when compared to control-group subjects. Compromise in multiple cognitive domains was observed only in adults with epilepsy (n = 42; 25.6 %).
Overweight/obesity was observed in 106 (64.6 %) adults with epilepsy and in 42 (59.1 %) control-group subjects. Demographic and clinical data are shown in table I.
Table I. Clinical and cognitive data, and anthropometric measurements of adults with epilepsy and control group subjects.
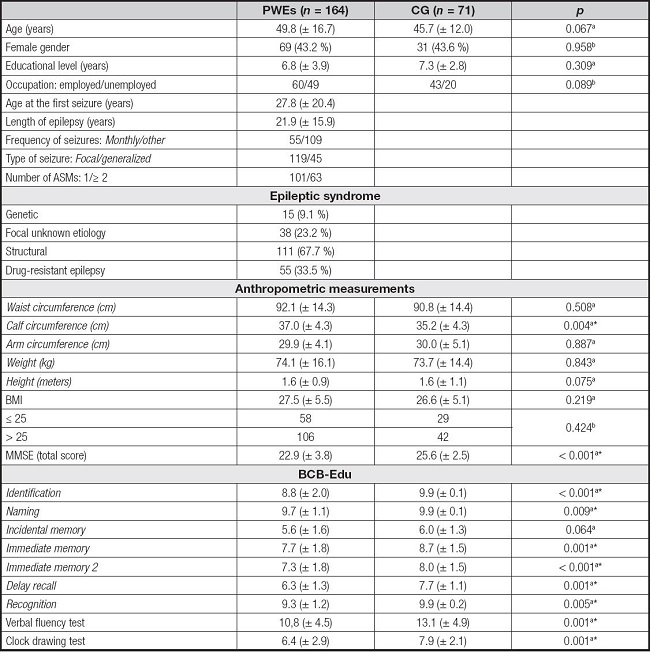
PWEs: people with epilepsy; CG: control group; ASMs: antiseizure medications; BMI: body mass index; MMSE: Mini-Mental State Examination; BCB-Edu: Brief Cognitive Battery-Edu;
at-test;
bchi-square test;
*p < 0.05.
CONTROL GROUP: ANTHROPOMETRIC INDICATORS AND CLINICAL VARIABLES
There was a significant correlation between weight and age (Pearson's correlation, -0.288; p = 0.015). There was no correlation between weight and educational level.
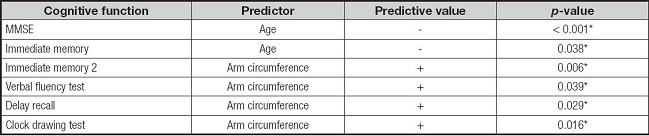
In the multiple linear regression to assess the factors associated with cognition outcomes in individuals in the control group, it was observed that younger age was related to better performance in the MMSE and in immediate memory. Greater arm circumference measurements were associated with better performance in immediate and delayed memories, and in the verbal fluency test and clock drawing test (Table II).
ADULTS WITH EPILEPSY: CLINICAL AND COGNITIVE DATA AND ANTHROPOMETRIC INDICATORS
Younger patients had lower body weight (Pearson's correlation; -0.259; p = 0.001), were taller (-0.486; p < 0.001), had greater calf circumference measurements (-0.159; p = 0.041), and lower waist circumference measurements (0.157; p = 0.044).
Overweight/obesity was associated with lower educational level, older age, and worse performance in some cognitive functions (Table III). There was no significant difference in overweight/obesity rates according to the type and length of epilepsy and the type and frequency of seizure.
Table III. Demographic, clinical, and cognitive aspects according to the BMI classification of adults with epilepsy.
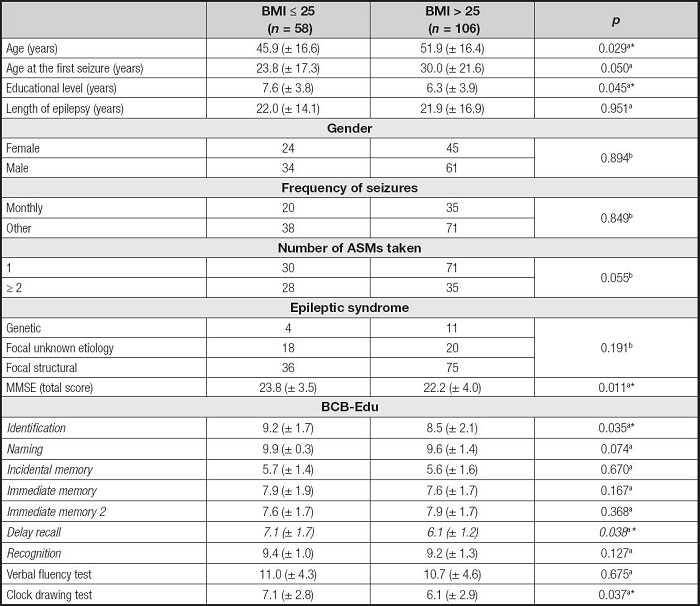
BMI: body mass index; MMSE: Mini-mental state examination; BCB-Edu: Brief Cognitive Battery-Edu; ASMs: antiseizure medications;
at-test;
bchi-square test;
*p < 0.05.
At the time of the assessment, the ASMs used in monotherapy or in association were: levetiracetam or lamotrigine in 12 cases each, carbamazepine in 95 cases, phenytoin in 15 cases, valproic acid in 49 cases, phenobarbital in 29 cases, topiramate in 5 cases, and clobazam in 48 cases. There was a higher occurrence of overweight in patients using valproic acid (monotherapy or polytherapy) when compared to those using other ASMs (chi-square; 26 (53 %) vs 31 (26.9 %); p = 0.013).
In the multiple linear regression model with stepwise variable selection with the AIC for each cognition parameter, it was observed that age, age at the first seizure, and the number of ASMs are predictors for the performance of memory, verbal fluency, and aspects of executive and visuospatial function (Table IV).
Table IV. Multiple linear regression to assess factors associated with cognition outcomes in adults with epilepsy.
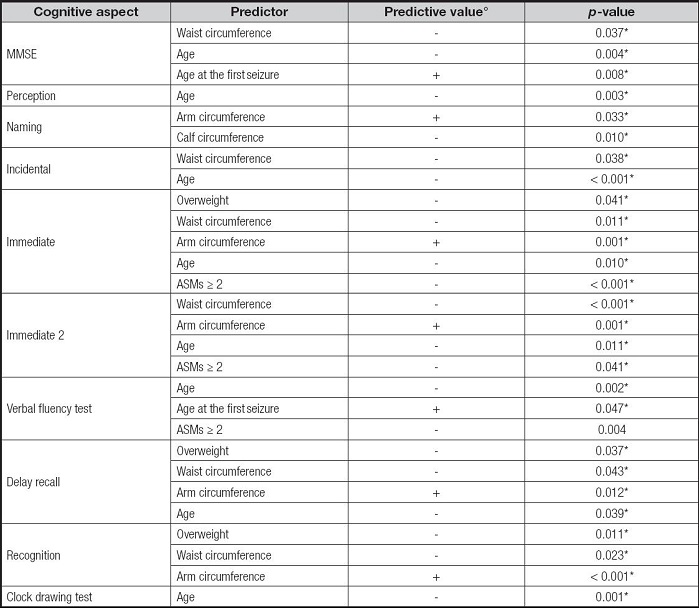
MMSE: Mini-mental state examination; ASMs: antiseizure medications;
°the regression coefficient was not included because it has no interpretation other than its direction, since the outcomes were transformed into ranks.
Greater waist circumference measurements were predictive of worse cognitive performance in the multiple linear regression analysis. Greater arm and calf circumference measurements were associated with better performance in several areas of cognitive functions. The presence of overweight was a predictor of worse performance in the tests of immediate, delayed, and recognition memories (Table IV).
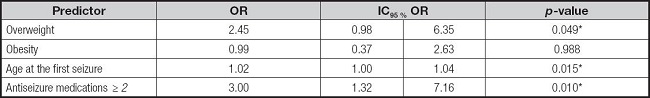
A multiple logistic regression with stepwise selection of variables was performed using the AIC to assess the predictive factors between clinical and anthropometric data. The model selected overweight, older age at the first seizure, and the use of polytherapy with ASMs as the variables with the greatest chance of impaired cognition (Table V).
DISCUSSION
This study showed a high occurrence of overweight/obesity in adults with epilepsy and in CG subjects, similar in terms of age, gender, and socioeconomic status. Obesity is a problem with serious repercussions on the health of the individual, being considered a worldwide epidemic and with an increase in prevalence in recent decades in developed and developing countries. Studies have described the occurrence of overweight/obesity and metabolic syndrome in adults with epilepsy using ASMs in 66.7 % of cases and in one third of all patients under 50 years old (18,19).
Epilepsy variables such as syndrome type, length of epilepsy, and seizure refractoriness do not seem to affect obesity, like the findings of Fernandes et al. and Ladino et al. (5,18). Differently, other studies describe an association between drug-resistant epilepsy and overweight/obesity (4,20,21). Regarding the pharmacological treatment of epilepsy, there are studies showing some effects of the treatment of neurological patients that can cause changes in the metabolic and nutritional status, including some micronutrient deficiencies such as zinc, folic acid, and vitamins C, D, E, B6, and B12, in addition to reducing energy consumption and changes in energy expenditure (22). There are also reports of weight gain caused by pharmacological treatment with some antiepileptic drugs in individuals with epilepsy (23). The use of valproic acid in monotherapy or polytherapy was associated with higher rates of obesity than those observed with the use of other ASMs, which corroborates the finding that significant weight gain is one of the most frequent problems experienced by individuals who use valproic acid and some modern ASMs (19,24).
COGNITION AND ANTHROPOMETRIC INDICATORS
There was a high occurrence of cognitive impairment in cases with different types of epilepsy with a mean length of 22 ± 15.9 years. Impairment in multiple cognitive domains was observed in a quarter of the cases. Cognitive deficits, particularly memory impairment, are described in several epilepsies and are associated with clinical features, epileptiform discharges, biological factors inherent to epilepsy or a combination of these factors (11,12,25). However, the findings on the relationship between cognition and anthropometric indicators are still conflicting and inflammatory and metabolic markers may be involved (26). Other studies suggest a possible common genetic pathway in the association between obesity, epilepsy, and a family history of epilepsy (5).
Overweight/obesity and greater waist circumference were associated with worse cognitive performance, including executive function and memory. Similarly, other studies describe that multiple metabolic, inflammatory, and vascular abnormalities are associated with poor cognitive performance in elderly people with chronic epilepsy (27). The relationship between obesity and adiposity with worse cognitive prognosis and dementia is biologically plausible. However, the pathophysiological evidence is still inconsistent, and the causes remain unclear.
In the regression test, the abdominal obesity was the stronger factor associated of cognitive impairment than whole-body adiposity. In obese individuals, executive dysfunction is possibly mediated by a low concentration of brain-derived neurotrophic factor, which is one of the factors responsible for neurogenesis, neuronal regeneration, and synaptic and axonal remodeling (28). In obese individuals, chronic neuroinflammation is related to an increase in inflammatory markers such as interleukin-6, tumor necrosis factor-α, and Toll-like receptors, which can promote changes in structures in cortical brain regions, in areas of the hippocampus, cerebellum and amygdala. In individuals with BMI > 30, cranial resonance studies describe exacerbated microglial activation and disruption of the blood-brain barrier, which may suggest that multiple neuroendocrine and immunometabolic aspects and alterations in brain structure and function are directly involved in the relationship between cognition and overweight/obesity (29-31).
In patients with impairment in multiple cognitive domains, the associated clinical variables were overweight, older age at the first seizure, and the use of more than one ASM (polytherapy), which suggests that several clinical factors of epilepsy, ASMs, and overweight play a role in the function cognitive in epilepsy.
Arm and calf circumference, which are measures of lean mass, were significantly associated with better performance in assessments of memories, aspects of executive function such as verbal fluency and the clock drawing test in adults with epilepsy and control group subjects. These data confirm the study of the American Health and Nutrition Examination Database in which the researchers observed that participants without lean mass depletion had better cognitive performance on the Digit Symbol Substitution Test (32). It is known that there is an association between the presence of lean mass preservation and less central fat, with the prevention of cognitive impairment in several samples.
Other investigations in patients with epilepsy with multidisciplinary approaches, from the nutritional point of view, have been conducted in different studies, relating anthropometric profile and food consumption (18), clinical and cognitive aspects with anthropometry (33), advances and perspectives of the ketogenic diet in refractory epilepsy (10), and food and its effects on neurological diseases (34).
This study has its limitations. An important one was the inclusion of a small sample from a single regional epilepsy treatment facility, which may overestimate the frequency of more severe cases and of difficult-to-control epilepsy in comparison with population samples. However, the data are robust on the occurrence of obesity/overweight and cognitive impairment in different types of epilepsy.
Thus, it is concluded that the occurrence of overweight/obesity and cognitive impairment was high in the adults with epilepsy. Impairment in several cognitive functions was associated with overweight, the use of polytherapy with ASMs, and greater waist circumference measurements. Greater arm and calf circumference were related to better cognitive performance.












 Curriculum ScienTI
Curriculum ScienTI