My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Anales de Psicología
On-line version ISSN 1695-2294Print version ISSN 0212-9728
Anal. Psicol. vol.30 n.2 Murcia May. 2014
https://dx.doi.org/10.6018/analesps.30.2.161421
Predictors of distress in hospital physicians: protective and vulnerability factors
Predictores de distrés en médicos hospitalarios: factores protectores y de vulnerabilidad
Fermín Martínez-Zaragoza1, Gemma Benavides-Gil1, Manuel Ato-García2, Ángel Solanes-Puchol1, Beatriz Martín-del-Río1, Jordi Fernández-Castro3 y Yolanda Pastor-Ruiz4
1 Universidad Miguel Hernández
2 Universidad de Murcia
3 Universidad Autónoma de Barcelona
4 Universidad Rey Juan Carlos
This study was carried out with the help of the Valenciana School of Health Studies (EVES). Project Reference PI092.
ABSTRACT
This study investigates the relationship between protective and vulnerability factors affecting health (distréss) in medical staff. Participants were 127 doctors from four public hospitals, who were administered the Occupational Stress in Health Professionals Inventory, the Ways of Coping Questionnaire, the Maslach Burnout Inventory, the Symptom Check-list-90 Revised Questionnaire, and the Flow Trait Scale-2. Following the methodology of Partial Least Squares modeling (PLS), an explanation is given for distréss in hospital physicians, where the avoidance coping strategy produces distréss directly (β = .296) and indirectly (β = .139) th rough its influence on the increase of burnout (β = .314), which in turn is increased by occupational stress (β = .209). Professional flow, measured by professional efficacy and flow, acts as a good protector against distréss (β = -.133), partly compensating the effects of the variables which have an increasing impact on an individual's distréss (GoF = .983). To sum up, when trying to predict a physician's distréss, four key elements should be considered: avoidance coping and its indirect effect through burnout on distréss; the burnout construct itself and professional flow.
Key words: Hospital physicians; burnout; flow; distréss; partial least squares modeling.
RESUMEN
Este estudio investiga la relación entre factores protectores y de vulnerabilidad que afectan la salud (distrés) del personal médico. Los participantes fueron 127 médicos de cuatro hospitales públicos, a quienes se les administró el Cuestionario de Estrés Ocupacional, el Cuestionario de Estilos de Afrontamiento, el Inventario de Burnout de Maslach, el Cuestionario de 90 Síntomas-Revisado y la Escala de Experiencia Óptima-2. Siguiendo la metodología de Mínimos Cuadrados Parciales (PLS) se propone una explicación del estrés en médicos hospitalarios, según la cual la estrategia de afrontamiento de evitación produce directamente distrés (β = .314), que a su vez se ve incrementado por el estrés ocupacional (β = .209). La experiencia optima profesional, medida mediante la eficacia profesional y el estado de flow, actuaria como un buen protector contra el distrés (β = -.133), compensando en parte los efectos de las variables que incrementan el distrés (ajuste global, GoF = .983). En resumen, cuatro serían los elementos a considerar al intentar predecir el distrés médico: afrontamiento evitativo y su efecto indirecto a través del burnout en el distrés, el constructo de burnout en sí mismo y la experiencia óptima profesional.
Palabras clave: médicos hospitalarios; burnout, flow; distrés; modelado de mínimos cuadrados parciales.
Introduction
Much has been written about the welfare and quality of life of patients in recent years, however, little attention has been paid to the welfare of doctors and how it affects patients (Shanafelt, Sloan & Habermann, 2003). Since the key elements to the smooth running of health systems are the health professionals, their care is crucial to understanding the health of the health system and of the patients, as recently stated by the President of the World Medical Association, Dr. Dana Hanson (2009), while addressing The Global Forum of Health Leaders conference in Taipei about attention to stress and burnout in doctors.
As indicated by Wallace, Lemaire and Ghali (2009), physicians have an important role in health systems and medical evidence indicates that many of them have health problems. A health system weakened by the fact that its most important components are not in good health leads to a series of direct consequences. If a doctor has poor health, the following outcomes in the health system appear: low productivity and efficiency by medical personnel, suboptimal quality of patient care (Revicki, May & Whitley, 1991), lower patient satisfaction and lower adherence to treatment and increased risk of medical errors, which are seen as a consequence of the health system. At the same time, a greater perception of stress, burnout, depression, substance abuse, suicide risk and problems in personal relationships are also observed among medical staff (Wallace et al., 2009). The "patient" doctor is also subjected to a series of physical problems, caused by a growing work demand and unhealthy lifestyles. Reig and Caruana (1990a) found that smoking behavior in these professionals is associated with different aspects of stress such as conflicts with patients and conflicts with the organization.
Data from the European Agency for Safety and Health at Work (EUOSHA, 2009) reported high levels of stress in the health worker sector. Prevalence of stress in health professionals for Latin-American countries was 36.30% in the study by Grau et al. (2008), 87.40% of which were doctors. In Spain, the Sixth National Survey on Working Conditions (Ministerio de Trabajo e Inmigracion, 2007) informed that stress is the most commonly reported illness among health workers (41%); even more so than, for example, headaches, depression and insomnia.
This clearly illustrates, therefore, that physicians suffer stress (Anderson, Cooper & Willmott, 1996; Bernaldo-Quiros & Labrador, 2008; Bethelmy-Rincon & Guarino, 2008; Knesebeck, Kelin, Grosse-Frie, Blum & Siegrist, 2010; McManus, Winder & Gordon, 1999, 2002; Schaufeli, Bakker, van der Heijden & Prins, 2009; Wallace et al., 2009). For McCue (1982) the sources of stress in medical practice could be the following: intense emotional work, contact with anxious people, discomfort and sometimes inability to express gratitude and affection, painful treatments, prohibition of pleasant habits, problematic patients, important clinical decisions and dealing with sensitive issues like sexuality or fear of death. Recently, concern and fear in relation to committing or being accused of malpractice is one of the more specific stressors among medical staff (Moreno-Jimenez & Penacoba, 1999).
In addition, many physicians suffer burnout (Blust, 2009; Goehring, Gallacchi, Kiinzi & Bovier, 2005; Keeton, Fenner, Johnson & Hayward, 2007; Moreno, Seminotti, Garrosa, Rodriguez & Morante, 2005). Maslach and Jackson (1982) suggested burnout as being a syndrome of chronic stress common among service professions where severe and prolonged attention is given to people who are in a situation of need or dependence. In their study, the two occupations most affected by the syndrome are education and health care. Although the factors that contribute to burnout in doctors are not entirely clear, there is evidence that among those that play an important role are: overload, choice of specialty, practice type, patient characteristics, lack of sleep, personality type, coping with death and suffering, medical errors, medical malpractice lawsuits, lack of control over the work environment and difficulties in reconciling work-family life (Shanafelt et al., 2003; Spickard, Gabbe & Christensen, 2002). Some studies try to explain the mechanisms that lead to burnout by looking at interpersonal and intrapersonal mechanisms (Martinez-Iñigo, Totterdell, Alcover & Holman, 2007). The impact that this has on the patient can be enormous; seriously deteriorating the doctor-patient relationship, dehumanizing treatment and doctors not devoting the necessary time and attention to each patient. A decrease in performance and work commitment, a reduction in career satisfaction and poorer quality care of patients has also been described (Goldberg et al., 1996; Lemkau, Rafferty & Gordon, 1994).
Several studies have linked stress and burnout in medical professionals (Segura-Bernal et al., 2006), finding reciprocal causal relationships between stress and emotional exhaustion (McManus et al., 2002). Cherniss (1980) developed a two-stage evolutionary model presenting burnout as the result of chronic exposure to stress. Also, if emotional exhaustion is compared among nurses and doctors, it is the latter who record the highest values (Maslach & Jackson, 1982). As discussed by Moreno-Jimenez et al. (2005), burnout among physicians is not terribly different from that of other professions, but their reactions are unique to some extent and have worrying consequences for patients.
When examining the coping strategies used by doctors to cope with the demands or stressors that lead to stress and burnout, mental disconnect and seeking social support appear to be the most used (Bethelmy-Rincon & Guarino, 2008; Escriba-Agiiir & Bernabe-Muñoz, 2002). Several studies (Etzion & Pynes, 1986; Thornton, 1992) have also indicated that avoidance coping, as defined in the model by Lazarus and Folkman (1984) is associated with the global presence of burnout. Traditional studies on the wellness of health professionals emphasize the negative impact on health from this type of coping such as, depression, burnout, substance abuse and divorce (Shanafelt et al., 2003). Bowman and Allen (1985), however, propose a model that separates positive and negative coping and McCue (1986) also made a division between positive and negative coping strategies. So, negative coping, can adversely affect doctors' health, while positive coping can be protective. Some doctors are unhappy in their work, which can manifest itself as stress or burnout (McManus et al., 2002). So stress, burnout and negative coping have a negative effect on doctors' health.
Different specific theoretical models have attempted to explain the relationship between stress, coping, burnout, and distréss. A general health model reference is the one by Wallace et al. (2009), where burnout, depression and stress are physician outcomes from workplace stressors, contextual factors and physician characteristics (indifference to personal wellness, avoidance). Physician selfcare and prevention is directed towards physician characteristics, and physician treatment and recovery is directed towards physician outcomes. Previous models (e.g., Belfer, 1989; Bowman & Allen, 1985) did not show the contextual factors. In Firth-Cozens' (1998) model, perceived stressors (overload, relationships, mistakes, violence... ) cause self-criticism, which causes stress and depression, which also increases perceived stressors in a cycle. Sleep loss correlates with perceived stressors.
McManus et al. (2002) proposed a model where emotional exhaustion is increased by stress and professional efficacy, which in turn increases stress again; cynicism decreases stress. However, with entirely different results, Graham, Potts and Ramirez (2002) found that job stress is associated with emotional exhaustion and psychiatric morbidity. Also, perceived stress results in poor mental health and personal accomplishment reduces the psychiatric morbidity.
There is, therefore, plenty of information regarding negative factors leading to distréss. The flow theory, however, may offer a new perspective by considering protective factors in response to stress. This concept was developed by Csikszentmihalyi (1990), and is defined as a state in which a person is completely absorbed in an activity that they enjoy, during which subjective time passes by faster and actions, thoughts and movements occur one after the other without a break. Their whole being is involved in this activity and a person uses their skills and abilities to their full potential. The concept of time disappears and a greater sense of satisfaction is experienced. The construct can be considered as the optimal psychological state for carrying out an activity (García, Jimenez, Santos-Rosa, Queen & Cervello, 2008), and is closely related to motivation and personal enjoyment (Csikszentmihaly, 1997). In its relation with distréss, it is the ability to transform an adversity into a challenge that can provide enjoyment; if a person can find flow in their job, this is a good way to improve the quality of life in general (Csikszentmihalyi, 1990).
Do doctors work in this way? We think to some extent they participate in this process, which is the opposite of distréss and burnout. However, there are no studies examining the relationship between flow and distréss in physicians. If we take the idea that professional efficacy acts opposite to emotional exhaustion and cynicism, we can expect flow and professional efficacy to form part of this same construct. Furthermore, it is possible, to consider professional efficacy as a protective factor. Greenglass, Burke and Moore (2003) propose a model in nurses where professional efficacy is decreased by distréss, and distréss increases depression.
Given the contradictory results found in literature and focusing on the possible protective factors of distréss, the purpose of this paper is to study the direct and indirect effects from coping strategies, burnout, and occupational stress on physicians' distréss, and the role that flow and professional efficacy have in this distréss. We are also interested in the direction and relative importance of these relationships.
Our research questions are: (i) what factors lead to burnout in doctors? (ii) what is the role of flow and professional efficacy in a physician's distréss?, and, (iii) what are the vulnerability and protective factors of distréss in hospital doctors?
In this sense, we propose a model to investigate the relationship between protective and vulnerability factors which affect distréss in medical staff.
Our hypotheses are: (a) negative coping styles (avoidance and distancing) are associated to distréss, (b) burnout produces distréss, (c) occupational stress increases burnout, (d) professional efficacy and flow decrease distréss, (e) cynicism and emotional exhaustion reflect burnout, (f) flow and professional efficacy reflect what we have called professional flow, (g) anxiety, depression, somatization, and hostility reflect distréss.
Method
Participants
127 physicians from the four largest national health hospitals in the Alicante province participated in this study. Physicians from the Emergency Unit were not considered for participating in the study due to the different type of tasks developed by them.
Materials
Occupational Stress in Health Professionals Inventory (Caruana, 1989; Reig & Caruana, 1990b).- Consists of 122 items related to stressful events which are characteristic of work carried out in hospitals. Health professionals have to indicate the level of stress, tension and irritability generated by each of the situations on a scale 0 (none) to 4 (very much), The test consists of seven factors relating to: contact with pain and death, conflicts with patients and their families, conflicts with superiors, emergency situations and severe deficiency issues, emotional stress and overwork. Internal consistency of all sizes ranges from .81 to .91, and test-retest reliability is .78. The inventory can also obtain an overall index of occupational stress in a hospital setting, which is used in this study.
Maslach Burnout Inventory (MBI-GS) (Schaufeli, Leiter, Maslach & Jackson, 1996).- Measures the frequency and intensity of burnout. Spanish translation and adaptation by Salanova, Schaufeli, Llorens, Peiro and Grau (2000). It consists of 22 items on a Likert response scale ranging from 0 (never) to ó (daily). It has three subscales: (a) emotional exhaustion, which refers to the feeling of being emotionally exhausted by work and less able to give to others; (b) depersonalization, also called cynicism, a response involving an impersonal, indifferent and cold attitude towards patients; (c) and staff performance, also known as professional efficacy, expressing feelings of competence and professional success, which contrasts with the previous two scales that are indicative of burnout. This inventory has shown high levels of reliability (from .73 to .85) for the assessment of the construct (Salanova et al., 2000).
Ways of Coping Questionnaire (Folkman & Lazarus, 1988).-Spanish translation and adaptation by Sanchez-Canovas (1991). This is perhaps the best known test for measuring coping strategies in Psychology. It consists of 66 items, with a response scale of four points (0 to 3), which evaluates eight ways for coping with stressful situations. For this study, the following are used: (a) distancing, or efforts to separate themselves from the situation, efforts to control or regulate one's own feelings and actions; and (b) avoidance or escape from the stressful situation.
The Symptom Checklist-90 Revised Questionnaire (SCL-90-R) (Derogatis, 1983).- Spanish translation and adaptation by Gonzalez-Rivera et al. (1989). This questionnaire was developed to assess current levels of psychological distréss that a person experiences and is one of the most frequently used tests to detect psychopathological or psychological symptoms. It consists of 90 items on a five-point scale (0 to 4), grouped into nine domains. In this study we focused on four: anxiety, depression, somatization and hostility. The reliability of the nine dimensions reaches values close to or above .70 in most studies of test-retest reliability and around .80 in the analysis of internal consistency (Derogatis, 1994; Derogatis & Savitz, 2000).
Flow Trait Scale-2 (Jackson & Marsh, 1996).- This test evaluates the flow trait based on the theory by Csikszent-mihalyi (1990) about optimal experience. Although this questionnaire was developed to measure optimal experience in sports and physical activity settings, these scales can be fruitfully applied in other areas such as education or work, in order to measure the optimal psychological state (Jackson, Martin & Eklund, 2008; Martin & Jackson, 2008). It consists of the following scales: (a) challenge-skill balance, based on the perception of challenge in relation to the ability that we have; (b) the merging of action and awareness, which involves being automatically absorbed in the task being performed without the intrusion of other thoughts; (c) clear goals, or knowledge of objectives and preparation and performance planning; (d) unambiguous feedback on the process and how performance is progressing in relation to goals; (e) total concentration, deep concentration, without any kind of distractibility; (f) sense of control over the task being carried out; (g) loss of self-consciousness or inhibition, which means transcending concerns about their own abilities; (h) time transformation, or alteration of real time perception; and (i) autotelic experience or quality of the experience as rewarding in itself. The scale allows for a total score of flow used in the study. With the Spanish adaptation of the test, Cronbach's alpha values of over .70, and scales much higher than .80 are obtained (García et al., 2008).
Procedure
A cover letter along with the project to be carried out was sent to the head of the hospitals and their ethics committees, who approved the study. Later, an interview was arranged with the hospital directors. Participants were volunteers and were informed in writing of the content of the study, duration, participation, the pros and cons of participating, and the possibility of receiving a personalized report of their results at the end of the study. It was clearly defined that the study was designed to investigate health in health professionals. No mention was made about distréss or health problems; so the investigation theme was blind to participants. An informed consent was signed by each participant. A personal letter was also sent to department heads to inform them about the study. Personal reports were confidential and only general results were presented to the hospital direction. Tests were completed during shifts in spare time.
Data analysis
Method justification. Partial Least Squares and Structural Equation Modeling
When trying to cope with models in Psychology we almost always think of Structural Equation Modeling (SEM) as the ideal way to analyze data. But SEM has some limitations which can make this task very difficult or impossible.
It is frequent to find low sample sizes when a researcher works with special samples where it is difficult to recruit participants. You can also find multicollinearity between variables, which causes serious problems for the analysis. Moreover, when coping with too many parameters, SEM has substantial problems in relation to parameter estimation and sample size, leading to non-identified models. Assumption of univariate and multivariate normality is another important theme. Maximum likelihood is the most extended estimation method, but data has to be distributed normally. Finally, management of missing data is another problem in this methodology.
What can be done in these cases? An interesting alternative statistical procedure, Partial Least Squares (PLS), could be a potential solution to these issues. It is not sensitive to low sample size, does not require normality in the distribution of data, can work with missing data, multicollinearity is not a problem and it can cope with more complex models. This procedure was developed by Wold (Wold, Ruhe, Wold & Dunn, 1984), and although it is not widely used in Psychology, it has been very successful in Chemistry and Marketing research (see Esposito-Vinzi, Chin, Henseler & Wang, 2010).
So, as a whole, the PLS method demands significantly fewer requirements compared to that of covariance structure analysis, but nevertheless delivers consistent estimation results.
Some Monte Carlo studies (Chin & Newsted, 1999) have shown that PLS performs well with much smaller (around 100 cases) samples sizes than the SEM requires (minimum 150-200 cases) to reach the same level of power, particularly with strong effect sizes. There are some examples with 85 and 200 cases in Campbell and Ntobedzi (2007) and Karim and Weisz (2010), respectively.
Results
Preliminary analysis
The mean age of the sample was 42.41 years (SD = 9.41), 57.20% were women. Mean years in the health profession was 18.27 (SD = 10.50), from those who had started in the medical world in the last year to some who had been in the profession for 40 years. Mean years in current job was 10.14 (SD = 8.02), some had been working in their current job for up to 32 years. Mean hours spent at work was 24.70 (SD = 10.10), although some professionals were committed to up to 78 hours per week, including hours spent at private clinics. The mean number of patients in daily professional care was 11.22 (SD = 9.63), although some doctors attended up to 40 patients a day. Night shifts per month were a mean of 3.60 (SD = 4.24). Work schedules were: 53.30% worked a morning shift, 0.80% an afternoon shift, 5.70% a split shift -39.30% mornings and evenings, and 0.80% at another time. Moreover, 28.30% of evaluated physicians also have work outside the hospital. Finally, 54.30% of them had a permanent contract. Only ó medical doctors (4.70%) were resident physicians. The rest were permanent staff.
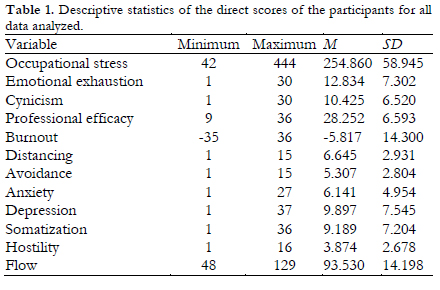
First of all, a descriptive statistics table of the direct scores of the participants for all data analyzed is shown (Table 1).
The analysis began with a complete model (Figure 1) containing all paths in the matrix between all variables of interest (emotional exhaustion, cynicism, occupational stress, anxiety, depression, hostility, somatization, avoidance and distancing coping styles scales, professional efficacy and flow), then the least significant variables were dropped sequentially until all remaining paths were significant. Scales from questionnaires were considered in order to define our models more precisely. The first steps were directed towards a model of vulnerability to anxiety and depression illnesses with burnout components.
Partial Least Squares (PLS) modeling
To test the models, the PLSPM package of free R software is used (Sanchez & Trinchera, 2010). Data were scaled in a standardized format and the weighting scheme was centroid. Bootstrapping methodology was used in order to estimate standard errors and evaluate statistical significance of loadings, path coefficients and r-squared values. One case with missing data was replaced by the mean. Results follow the recommendations by Chin (2010).
The final model is reflective, with five latent variables.
Outer model
Latent variable negative coping has one indicator: avoidance. Latent variable burnout has two indicators: cynicism and emotional exhaustion. Latent variable stress has one indicator: occupational stress. Latent variable professional flow has two indicators: flow and professional efficacy. Latent variable distréss has four indicators: somatization, hostility, anxiety and depression.
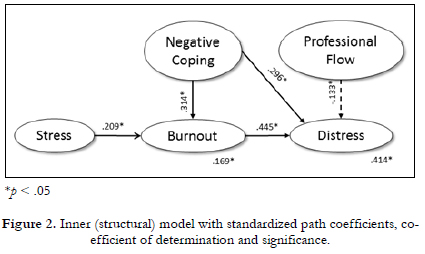
Inner model
Negative coping produces an indirect effect (through burnout) and a direct effect on distréss. Stress influences distréss through burnout. Professional flow has a direct and negative effect on distréss.
Evaluation of the reflective measurement (outer model). Model fit and fit criteria model
Fit criteria assessment was made according to the criteria proposed by Chin (1998) and Gotz, Liehr-Gobbers and Krafft (2010).
Content validity
All the constructs show unidimensionality. The first eigen-values were higher than 1 and the second eigen-values were lower than 1 (see Table 2).
Indicator reliability
All the loadings of the latent constructs on their indicator variables are higher than the other loadings on these indicators (see Table 3). Loadings are above or near .700. The constructs are well explained by their indicators.
Construct reliability
Dillon, Goldstein-Joreskog Rho (DG) is above .750. All the construct's indicators jointly measure the construct adequately (Table 2).
Convergent validity
Average variance extracted (AVE) is higher than .500 in all cases (Table 2). For the global model, mean communality index is .687 and mean redundancy index is .198.
Discriminant validity
Fornell and Larcker (1981) demonstrated that there is discriminant validity if a latent variable's AVE is larger than the common variances (squared correlations) of this latent variable with any other of the model's constructs. This is true in all cases (see Table 2).
Despite the relatively low sample size, statistical power was moderate, attending the high loadings score values and bootstrap results (Marcoulides & Saunders, 2006).
Evaluation of the structural model (inner model). Model fit and fit criteria
Figure 2 represents the inner (structural) model. R -squared indices of endogenous variables (see Table 2) vary from .169, weak effect, to .414, moderate to substantial effect (Chin, 1998).
In Table 4 you can also find detailed information about the nonparametric bootstrap procedure, standard errors and 95% confidence interval for structural paths. All paths were significant at .05 probability level. Table 2 also shows interconstruct correlations.
The hypothesized model has an excellent fit, based on goodness of fit indices (GoF) by Tenenhaus, Amato and Esposito-Vinzi (2004). A GoF above the .900 threshold suggests a good model. Relative goodness of fit index (GoF) was .983; and reached a maximum value of .996 for the outer (measurement) model and .987 for the inner (structural) model.
Partial mediation effects of burnout (β = .139) on the relationship between Negative coping and distréss were also significant (t (120) = 3.23; p < .05), using the Sobel test (Sobel, 1982).
Discussion
The main purpose of this paper was to study the vulnerability and protective factors that lead to distréss in hospital doctors, their direct and indirect effects, and the direction and relative importance of these relationships.
This paper introduced a model about predictors of professional distréss that has been tested on Spanish hospital physicians. The model hypothesized that professional flow was a protective factor that influenced distréss, whereas burnout, negative coping and stress were vulnerability factors that lead to distréss in physicians.
The results confirm in general the proposed model, where burnout influences distréss directly, negative coping has a direct and indirect effect on distréss and stress has an indirect effect. On the other hand, professional flow has a direct and negative influence on distréss.
The hypotheses presented as part of the proposed model were confirmed except for the influence of distancing coping, as a part of negative coping factor, on distréss. This coping style was expected to be associated with burnout, but no findings were found in this sense. One possible explanation for why distancing is not associated with burnout, as was supposed, is that on the one hand, distancing may be related to low motivation, but on the other, it prevents overcommitment, which leads to burnout (Blomberg&Sahlber-Blom, 2007).
distréss, theorized here as a sum of anxiety, depression, hostility and somatization, has a defined concept which is explained by the anxiety-mood problems commonly reported by physicians (Firth-Cozens, 1998). These are also commonly reported symptoms of burnout. Partial mediational effects of burnout on distréss were also found. Therefore, one might think that, occupational stress does not produce distréss directly. These results agree with previous studies, where occupational stress increases burnout (Cherniss, 1980), and burnout along with avoidance causes distréss.
Regarding distréss, there have been reports in previous studies of links between depression and distréss (Hammen, 2005), hostility and vulnerability to distréss (Houston, Smith& Cates, 1989), anxiety and distréss (Gomez, 2004), and distréss and somatization (Bernaldo-Quiros& Labrador, 2008) in health professionals, but taken separately and not as part of a more complex model. It is interesting to consider that depression, anxiety, hostility and somatization can be symptoms found in physicians as a result of the influence of occupational stress, burnout and avoidance. Depression, anxiety, hostility and somatization can affect a physician's health and influence, what Wallace et al. (2009) call healthcare system outcomes, represented by reduced productivity and efficiency, and suboptimum quality of patient care. Avoidance is also an apparent characteristic in physicians, which is an important issue requiring further explanation and consideration with respect to interventions for improving physicians' health and the health system.
The introduction to this study states that the factors influencing burnout in physicians were unclear (Shanafelt et al., 2003). Beyond the specific factors, the results show the direct importance of stress in the generation of burnout, as well as the use of the avoidance coping strategy as a means of increasing distréss. Regarding the models mentioned in the introduction, this model coincides with McManus et al. (2002) regarding the point that stress increases emotional exhaustion (burnout includes this in the model presented) but differs with respect to the fact that cynicism acts together with emotional exhaustion and increases distréss. Another difference is that professional efficacy with flow decreases distréss. It also coincides with the model by Graham et al. (2002) regarding the fact that job stress increases emotional exhaustion (part of burnout), personal efficacy reduces psychiatric morbidity (distréss) and emotional exhaustion increases psychiatric morbidity. These differences exist because job stress increases psychiatric morbidity indirectly, but not directly; and cynicism and emotional exhaustion act together. To sum up, these results in general support the results from Graham et al. (2002), but disagree with the model by McManus et al. (2002). Other points to be considered in relation to the decrease of the effects of burnout are the importance of not having an avoidance coping style, the role of flow along with professional efficacy and a non-adequate coping style.
Conclusions
This study can help us to locate the explanatory mechanisms that lead to distréss in physicians; one of the main objectives considered. From these findings, when trying to predict the physician's distréss into the analyzed context, four key elements should be considered: avoidance coping and its indirect effect through burnout on distréss; occupational stress and its indirect effect through burnout on distréss; the burnout construct itself and professional flow.
Any potential interventions based in these conclusions can follow the suggestions contributed by Wallace et al. (2009) focus on physician self-care and prevention (avoidance) and physician treatment and recovery (distréss). Also, authors like Sime, Campbell, Saleh and Martin (2007) and Sotile and Sotile (2003) have proposed ways of treating burnout in doctors, and by following their advice it is possible to design a complex treatment package, including coping styles and teaching flow and professional efficacy as ways of reducing this distréss.
This study has of course limitations. Sample size was restricted by the number of volunteers participating, so in the future it will be important to study better ways of recruiting more physicians to participate in the study. Having access to data from other hospitals in Spain, as well as private hospitals, could complete this study. It would also be interesting to test this model using a Structural Equation Model (SEM) methodology. 41.40% variance of distréss has been explained, so other variables are affecting this distréss.
Future studies should investigate if protective and vulnerability factors change over time and what variables they depend on apart from those studied. A physician's personality traits can provide some ideas for this subject. It would also be helpful to know if special characteristics pertaining to the different specialties or wards influence the way physicians cope with stress and burnout and if they affect distréss. By changing these variables, we could noticeably improve a physician's distréss in professional contexts as a way of improving patient's health at the same time.
References
1. Anderson, W. J. R., Cooper, C. L. & Willmott, M. (1996). Sources of stress in the national health services: A comparison of seven occupational groups. Work & Stress, 10, 88-95. [ Links ]
2. Belfer, B. (1989). Stress and the medical practitioner. Stress Medicine, 5, 109-113. [ Links ]
3. Bernaldo-Quirós, M. & Labrador, F. J. (2008). Relaciones entre estrés laboral, burnout y síntomas psicopatológicos en los servicios de urgencia extrahospitalaria del área 9 de Madrid. Anuario de Psicología Clínica y de La Salud, 4, 53-61. [ Links ]
4. Bethelmy-Rincón, L. & Guarino, L. (2008). Estrés laboral, afrontamiento, sensibilidad emocional y síntomas físicos y psicológicos en médicos venezolanos. Revista Colombiana de Psicología, 17, 43-58. [ Links ]
5. Blomberg, K. & Sahlberg-Blom, E. (2007). Closeness and distance: A way of handling difficult situations in daily care. Journal of Clinical Nursing, 16, 244-254. [ Links ]
6. Blust, L. (2009). Health professional burnout. Journal of Palliative Medicine, 12, 639-640. [ Links ]
7. Bowman, M. A. & Allen, D. I. (1985). Stress and women physicians. New York: Springer-Verlag. [ Links ]
8. Campbell, A. & Ntobedzi, A. (2007). Emotional intelligence, coping and psychological distréss. A PLS approach to developing a predictive model. Electronic Journal of Applied Psychology, 3(1), 39-54. [ Links ]
9. Caruana, A. (1989). Evaluación del estrés ocupacional en profesionales de la salud (Unpublished doctoral dissertation). University of Alicante, Alicante, Spain. [ Links ]
10. Cherniss, C. (1980). Staff burnout: Job Stress in the Human Services. London: Sage Publication. [ Links ]
11. Chin, W. W. (1998). The partial least squares approach to structural equation modeling. In G. A. Marcoulides (Ed.), Modern methods for business research (pp. 295-358). Mahwah, NJ: Lawrence Erlbaum Associates. [ Links ]
12. Chin, W. W. (2010). How to write up and report PLS analyses. In V. Esposito-Vinzi, W. W. Chin, J. Henseler & H. Wang (Eds.), Handbook of partial least squares. Concepts, methods and applications (pp. 655-690). New York: Springer. [ Links ]
13. Chin, W. W. & Newsted, P. R. (1999). Structural Equation Modeling Analysis with Small Samples Using Partial Least Squares. In R. Hoyle (Ed.), Statistical Strategies for Small Sample Research (pp. 307-341). Thousand Oaks, CA: Sage Publications. [ Links ]
14. Csikszentmihalyi, M. (1990). Flow: The psychology of optimal experience. New York: Harper & Row. [ Links ]
15. Csikszentmihalyi, M. (1997). Finding flow: The psychology of engagement with everyday life. New York: Harper Perennial. [ Links ]
16. Derogatis, L. R. (1983). SCL-90-R: Administration and scoring procedures manual II. Towson, MD: Clinical Psychometric Research. [ Links ]
17. Derogatis, L. R. (1994). SCL-90-R. Symptom Checklist-90-R. Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer System. [ Links ]
18. Derogatis, L. R. & Savitz, K. L. (2000). The SCL-90-R and brief symptom inventory (BSI) in primary care. In M. E. Maruish (Ed.), Handbook of psychological assessment in primary care setting (pp. 297-334). Mahwah: Lawrence Earlbaum. [ Links ]
19. Escribà-Agüir, V. & Bernabé-Muñoz, Y. (2002). Estrategias de afrontamiento ante el estrés y fuentes de recompensa profesional en médicos especialistas de la Comunidad Valenciana. Un estudio con entrevistas semiestructuradas. Revista Española de Salud Pública, 76(5), 595-604. [ Links ]
20. Esposito-Vinzi, V., Chin, W. W., Henseler, J. & Wang, H. (2010). Handbook of partial least squares. Concepts, methods and applications. London: Springer. [ Links ]
21. Etzion, D. & Pines, A. (1986). Sex and culture in burnout and coping among human service professionals. Journal of Cross Cultural Psychology, 17, 191-209. [ Links ]
22. European Agency for Safety and Health at Work (2009). Stress at work- facts and figures. Luxembourg: Office for Official Publications of the European Communities. Retrieved from https://osha.europa.eu/en/publications/reports/TE-81-08-478-EN-C_OSH_in_figures_stress_at_work. [ Links ]
23. Firth-Cozens, J. (1998). Individual and organizational predictors of depression in general practitioners. British Journal of General Practice, 48, 1647-1651. [ Links ]
24. Folkman, S. & Lazarus, R. S. (1988). Ways of coping questionnaire. Redwood, CA: Mind Garden. [ Links ]
25. Fornell, C. & Larcker, D. F. (1981). Evaluating structural equation models with unobserved variables and measurement error. Journal of Marketing Research, 18, 39-50. [ Links ]
26. García, T., Jiménez, R., Santos-Rosa, F. J., Reina, R. & Cervelló, E. (2008). Psychometric properties of the Spanish version of the flow state scale. The Spanish Journal of Psychology, 11, 660-669. [ Links ]
27. Goehring, C., Gallacchi, M. B., Kunzi, B. & Bovier, P. (2005). Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: A cross-sectional survey. Swiss Medical Weekly, 135, 101-108. [ Links ]
28. Goldberg, R., Boss, R. W., Chan, L., Goldberg, J., Mallon, W. K. & Mora-dzadeh, D. (1996). Burnout and its correlates in emergency physicians: Four years' experience with a wellness booth. Academy Emergency Medicine, 3, 1156-64. [ Links ]
29. Gómez, R. (2004). El estrés laboral del médico: Burnout y trabajo en equipo. Revista de la Asociación Española de Neuropsiquiatría, 24 (90), 3102-3115. [ Links ]
30. González de Rivera, J. L., Derogatis, L.R., de las Cuevas, C., Gracía Marco, R., Rodríguez-Pulido, F., Henry-Benítez, M. & Monterrey, A. L. (1989). The spanish version of the SCL-90-R. Normative data in the general population. Towson, MD: Clinical Psychometric Research. [ Links ]
31. Götz, O., Liehr-Gobbers, K. & Krafft, M. (2010). Evaluation of structural equation models using the partial least squares (PLS) approach. In V. Esposito-Vinzi, W. W. Chin, J. Henseler & H. Wang (Eds.), Handbook of partial least squares. Concepts, methods and applications (pp. 691-711). Berlin: Springer. [ Links ]
32. Graham, J., Potts, H. W. W. & Ramirez, A. J. (2002). Stress and burnout in doctors. The Lancet, 360, 1975-1976. [ Links ]
33. Grau, A., Flichtentrei, D., Suñer, R., Font-Mayolas, S., Prats, M. & Braga, F. (2008). El burnout percibido o sensación de estar quemado en profesionales sanitarios: Prevalencia y factores asociados. Informació Psicològica, 91-92, 64-79. [ Links ]
34. Greenglass, E. R., Burke, R. J. & Moore, K. A. (2003). Reactions to increased workload: Effects on professional efficacy of nurses. Applied Psychology: An International Review, 52, 580-597. [ Links ]
35. Hammen, C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1, 293-319. [ Links ]
36. Hanson, D. (2009). Physicians sufferingfrom "silent desperation", says WMA leader. Retrieved from http://www.wma.net/en/40news/20archives/2009/2009_16/. [ Links ]
37. Houston B. K., Smith M. A. & Cates D. S. (1989). Hostility patterns and cardiovascular reactivity to stress. Psychophysiology, 26, 337-342. [ Links ]
38. Jackson, S. A. & Marsh, H. (1996). Development and validation of a scale to measure optimal experience: The flow state scale. Journal of Sport & Exercise Psychology, 18, 17-35. [ Links ]
39. Jackson, S., Martin, A. J. & Eklund, R. C. (2008). Long and short measures of flow: The construct validity of the FSSS-2, DFS-2, and new brief counterparts. Journal of Sport & Exercise Psychology, 30, 561-787. [ Links ]
40. Karim, J. & Weisz, R. (2010). Emotional labour, emotional intelligence and psychological distréss. Journal of the Indian Academy of Applied Psychology, 36 (2), 187-196. [ Links ]
41. Keeton, K., Fenner, D. E., Johnson, T. R. B. & Hayward, R. A. (2007). Predictors of physician career satisfaction, work-life balance, and burnout. Obstetrics & Gynecology, 109, 949-955. [ Links ]
42. Knesebeck, O., Kelin, J., Grosse-Frie, K., Blum, K. & Siegrist, J. (2010). Psychosocial stress among hospital doctors in surgical fields. Results of a nationwide survey in Germany. Deutsches Arzteblatt International, 107 (14), 248-253. [ Links ]
43. Lazarus, R. & Folkman, S. (1984). Stress, appraisal and coping process. New York: McGraw Hill. [ Links ]
44. Lemkau, J., Rafferty, J. & Gordon, R. J. (1994). Burnout and career-choice regret among family practice physicians in early practice. Family Practice Research Journal, 14, 213-22. [ Links ]
45. Marcoulides, G. A. & Saunders, C. (2006). PLS: A Silver Bullet? MIS Quarterly, 30 (2), iii-ix. [ Links ]
46. Martin, A. & Jackson, S.A. (2008). Brief approaches to assessing task absorption and enhanced subjective experience. Examining 'short' and 'core' flow in diverse performance domains. Motivation and Emotion, 32, 141-157. [ Links ]
47. Martínez-Íñigo, D., Totterdell, P., Alcover, C. M. & Holman, D. (2007). Emotional labour and emotional exhaustion: Interpersonal and intrapersonal mechanisms. Work & Stress, 21, 30-47. [ Links ]
48. Maslach, C. & Jackson, S. E. (1982). Burnout in health professions: A social psychological analysis. In G. Sanders & J. Suls (Eds.), Social psychology of health and illness (pp. 227-251). Hillsdale, NJ: Lawrence Erlbaum. [ Links ]
49. McCue, J. D. (1982). The effects of stress on physicians in their medical practice. The New England Journal of Medicine, 306, 458-464. [ Links ]
50. McCue, J. D. (1986). Doctors and stress: Is there really a problem? Hospital Practice, 1 (5), 7-16. [ Links ]
51. McManus, I. C., Winder, B. C. & Gordon, D. (1999). Are UK doctors particularly stressed? The Lancet, 354 (9187), 1358-1359. [ Links ]
52. McManus, I. C., Winder, B. C. & Gordon, D. (2002). The causal links between stress and burnout in a longitudinal study of UK doctors. The Lancet, 359 (9323), 2089-2090. [ Links ]
53. Ministerio de Trabajo e Inmigración (2007). VI Encuesta Nacional de Condiciones de Trabajo. Madrid: Ministerio de Trabajo e Inmigración. Retrieved January from http://www.insht.es/Observatorio/Contenidos/InformesPropios/Desarrollados/Ficheros/Informe_VI_ENCT.pdf. [ Links ]
54. Moreno-Jiménez, B. & Peñacoba, C. (1999). El Estrés asistencial de los servicios de salud. En M. A. Simón (Ed), Manual de Psicología de la salud (pp. 739-764). Madrid: Siglo XXI. [ Links ]
55. Moreno-Jiménez, B., Seminotti, R., Garrosa-Hernández, E., Rodríguez-Carvajal, R. & Morante-Benadero, M. E. (2005). El burnout medico: la ansiedad y los procesos de afrontamiento como factores intervinientes. Ansiedady Estres, 11(1), 87-100. [ Links ]
56. Reig, A. & Caruana, A. (1990a). Consumo de tabaco en profesionales de la salud y su relación con el estrés ocupacional. In COP (Ed.), Actas del II Congreso del Colegio Oficial de Psicólogos. Comunicaciones. Psicología del Trabajo y de las Organizaciones (pp. 155-160). Madrid: Colegio Oficial de Psicólogos. [ Links ]
57. Reig, A. & Caruana, A. (1990b). Cuestionario de estres ocupacional para profesionales de la salud: Propiedades psicométricas preliminares. In COP (Ed.), Actas del II Congreso Del Colegio Oficial De Psicólogos. Comunicaciones. Psicología del Trabajo y de las Organizaciones (pp. 137-143). Madrid: Colegio Oficial de Psicólogos. [ Links ]
58. Revicki, D. A., May, H. J. & Whitley, T. W. (1991). Reliability and validity of the work-related strain inventory among health professionals. Behavioral Medicine, 17 (3), 111-120. [ Links ]
59. Salanova, M., Schaufeli, W., Llorens, S., Peiró, J. M. & Grau, R. (2000). Desde el "Burnout" al "Engagement": una nueva perspectiva? Revista de Psicología del Trabajo y de las Organizaciones, 16, 117-134. [ Links ]
60. Sánchez, G. & Trinchera, L. (2010). Package 'plspm' (Computer software). Retrieved from http://cran.r-project.org/web/packages/plspm/plspm.pdf. [ Links ]
61. Sánchez-Cánovas, J. (1991). Evaluación de las estrategias de afrontamiento. In G. Buela & V. Caballo (Eds.), Manual de psicología clínica y aplicada (pp. 247-260). Madrid: Siglo XXI. [ Links ]
62. Schaufeli, W. B., Bakker, A. B., van der Heijden, F. M. M. & Prins, J. T. (2009). Workaholism, burnout and well-being among junior doctors: The mediating role of role conflict. Work & Stress, 23, 155-172. [ Links ]
63. Schaufeli, W. B., Leiter, M. P., Maslach, C. & Jackson, S. E. (1996). Maslach Burnout Inventory - General Survey. In C. Maslach, S. E. Jackson & M. P. Leiter (Eds.), The Maslach Burnout Inventory Test Manual (pp. 19-26). Palo Alto, CA: Consulting Psychologist Press. [ Links ]
64. Segura-Bernal, Ferrer-Ventura, M., Palma-Sevillano, C., Ger-Cabero, S., Domènech-Cortés, M., Gutiérrez-Blanch, I. & Cebria-Andreu, J. (2006). Valores personales y profesionales en médicos de familia y su relación con el síndrome del burnout. Anales de Psicología, 22 (1), 45-51. [ Links ]
65. Shanafelt, T. D., Sloan, J. A. & Habermann, T. M. (2003). The well-being of physicians. The American Journal of Medicine, 114, 513-519. [ Links ]
66. Sime, W. E., Campbell, J., Saleh, K. J. & Martin, W. (2007). Critical decisions, trauma, and burnout in medicine: A stress management challenge to physician well-being. Biofeedback, 35 (3), 95-100. [ Links ]
67. Sobel, M. E. (1982). Asymptotic confidence intervals for indirect effects in structural equation models. In S. Leinhardt (Ed.), Sociological Methodology 1982 (pp. 290-312). Washington DC: American Sociological Association. [ Links ]
68. Sotile, W. M. & Sotile, M. O. (2003). Beyond physician burnout: Keys to effective emotional management. Journal of Medical Practice Management, 18 (6), 314-318. [ Links ]
69. Spickard, A., Gabbe, S. G. & Christensen, J. F. (2002). Midcareer burnout in generalist and specialist physicians. JAMA: The Journal of the American Medical Association, 288 (12), 1447-1450. [ Links ]
70. Tenenhaus, M., Amato, S. & Espósito-Vinzi, V. (2004). A global goodness-of-fit index for PLS structural equation modeling. Proceedings of the XLII Italian Statistical Society Scientific Meeting (pp. 739-742). Padova, Italy. [ Links ]
71. Thornton, P. I. (1992). The relation of coping, appraisal and burnout in mental health workers. The Journal of Psychology, 126, 261-271. [ Links ]
72. Wallace, J. E., Lemaire, J. B. & Ghali, W. A. (2009). Physician wellness: A missing quality indicator. The Lancet, 374, 1714-21. [ Links ]
73. Wold, S., Ruhe, A., Wold, H. & Dunn, J. (1984). The collinearity problem in linear regression. The Partial Least Squares (PLS) approach to generalized inverses. SIAM Journal on Scientific and Statistical Computing, 5 (3), 735-743. [ Links ]
![]() Correspondence:
Correspondence:
Fermín Martínez Zaragoza.
Departamento de Psicología de la Salud.
Universidad Miguel Hernández.
Avda. de la Universidad s/n.
Edificio Altamira.
03202 Elche, Alicante (Spain).
E-mail: f.martinez@umh.es
Article received: 25-10-2012
Reviewed: 3-12-2012
Accepted: 22-2-2013