My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Anales de Psicología
On-line version ISSN 1695-2294Print version ISSN 0212-9728
Anal. Psicol. vol.30 n.3 Murcia Oct. 2014
https://dx.doi.org/10.6018/analesps.30.3.168911
The development of the therapeutic alliance and the emergence of alliance ruptures
El desarrollo de la alianza terapéutica y la aparición de rupturas en la alianza
Joana Coutinho1, Eugenia Ribeiro1, Catarina Fernandes1, Inês Sousa2 and Jeremy D. Safran3
1School of Psychology, University of Minho, Braga (Portugal)
2Department of Mathematics and Applications, University of Minho, Braga (Portugal)
3New School for Social Research and Beth Israel Medical Center, New York (New York)
The authors want to thank Ariel Westermen for her support on the editing of this paper and revision of the English writing quality.
This article was supported by the Portuguese Foundation for Science and Technology (FCT) - PhD Grant: SFRH/BD/27654/2006.
ABSTRACT
Objectives: This study evaluated the development of the therapeutic alliance and the emergence of alliance ruptures, in a sample of patients with different diagnosis and different therapeutic outcome.
Design: We examined the longitudinal data of 38 therapeutic dyads receiving cognitive-behavioural therapy, including dropouts as well as successful and unsuccessful cases. The sample included cases with Axis I and Axis II disorders.
Method: At the end of each session, patients evaluated the alliance using the Working Alliance Inventory (WAI). Six judges trained in the observation of alliance rupture markers with an observational system of ruptures, rated 201 videotaped sessions. Longitudinal statistical models were applied to the data.
Results: We found that the pattern of alliance development of successful cases was different from the unsuccessful and dropouts cases. In addition on average, patients with personality disorders began therapy with a lower WAI score that decreased over time, whereas patients with Axis-I disorders began therapy with a higher WAI score that increased over time.
Key words: alliance development; alliance ruptures; axis I disorders; axis II disorders.
RESUMEN
Objetivos: Este estudio evaluó el desarrollo de la alianza terapéutica y la aparición de rupturas de alianzas, en una muestra de pacientes con diferentes diagnósticos y resultados terapéuticos.
Diseño: Se analizaron los datos longitudinales de 38 diadas terapéuticas que recibieran terapia cognitivo-conductual. La muestra incluyó a casos de abandonos, asi como casos exitosos y no exitosos. La muestra incluyó a casos con trastornos del Eje I y Eje II.
Método: Al final de cada sesión, los pacientes evaluaron la alianza mediante el Inventario de Alianza de Terapéutica (WAi). Seis jueces entrenados en la observación de los marcadores de ruptura de alianza con un sistema de observación de rupturas, codificaran 201 sesiones terapéuticas grabadas en video. Se aplicaran modelos estadísticos longitudinales a los datos.
Resultados: Se encontró que el patrón de desarrollo de la alianza de los casos de éxito era diferente de la de los casos sin éxito y abandonos. En media, los pacientes con trastornos de la personalidad iniciaran la terapia con una menor puntuación en el WAI que disminuyó con el tiempo, mientras que los pacientes con trastornos del Eje I iniciaran la terapia con una mayor puntuación en el WAI que aumentó con el tiempo.
Palabras clave: Desarrollo de la alianza terapéutica; rupturas en la alianza; trastornos del Eje I; trastornos del Eje II.
Introduction
Previous research has shown that the therapeutic alliance plays an important role in therapy. The alliance has been shown to be a consistent predictor of therapy outcome (e.g., Horvath & Bedi, 2002; Horvath Del Re, Fliickiger, & Symonds, 2011; Martin, Garske & Davis, 2002), as well as one of the most important common factors across various therapy modalities (Wampold, 2001; Horvath, 2011). More recently, however, Safran, Muran, and Eubanks-Carter (2011, p. 80) clarified the factors that contribute to the therapeutic alliance in what they refer to as "the second generation" of alliance research. This line of research on the processes of alliance development investigates phenomena such as alliance ruptures and its resolution. Within the same line of research, our study aims to evaluate the development of the alliance and the emergence of alliance ruptures in a sample of patients with different diagnosis and therapeutic outcome.
The process of alliance development and rupture emergence has been studied by several authors over the last decades. Several longitudinal studies (e.g., Golden & Robbins, 1990; Patton, Kivlighan, & Multon, 1997; Kivlighan & Shaughnessy, 2000; Stiles et al., 2004) tracked alliance development using different statistical methods and identified distinct patterns associated with the alliance evolution across time. In general, the aforementioned studies suggest that positive linear increase and quadratic high-low-high patterns of alliance development are related to good therapeutic outcomes. Stiles et al. (2004) did not find this quadratic pattern; however, they identified that a subset of patients who presented better outcomes experienced rupture-repair sequences signalled by brief V-shaped deflections on the alliance scores. Strauss et al. (2006) replicated these results in a sample of patients with either obsessive-compulsive or avoidant personality disorder who received cognitive behavioral therapy: they found that rupture-resolution sequences were significantly related to the relief of depressive and disordered personality symptoms. More recently, Stiles and Goldsmith, (2010) in a revision of studies on the development of the alliance over time, reflected on the higher plausibility for the -shaped alliance pattern when compared with the U-shaped pattern, considering the feasibility of therapy. Although these two patterns would be theoretically coherent, signalling alliance ruptures and resolutions events, produced by the therapeutic work in the middle phase of therapy, they are not empirically consistent across studies and their association with outcome was not always demonstrated.
In this same revision, while the authors concluded for the higher consistency of the occurrence of the linear increasing pattern of alliance development, as well as for its positive relation with therapeutic outcomes, they discussed the diversity of findings reported in the literature. The authors argued that several factors influence the results in this line of alliance research, such as the process variables studied, the design, and the data collection and analysis method. Most of these longitudinal studies (e.g., Kivlighan & Shaughnessy, 2000; Stiles et al, 2004; Strauss et al., 2006) used self-report methods to discriminate different patterns of alliance development and their relationship to therapeutic outcome.
Despite the common occurrence of ruptures in therapy (Eubanks-carter, Muran & Safran, 2010), self-report methods of alliance evaluation filled by the client and the therapist at the end of each session, may hide the rupture - resolution episodic pattern that takes place within the session and thus obscure its association with therapeutic outcomes. Therefore, to study both the development of the quality of the alliance and the emergence of alliance ruptures over treatment, may contribute to better understand the association between alliance patterns and therapeutic outcomes.
The pattern of development of the alliance and its relationship with therapeutic outcome may take different forms with patients with personality disorders due to the well-known difficulty of these patients in establishing the therapeutic alliance (Benjamin & Karpiak, 2001). Personality disordered patients constitute a group of patients in which the emergence of alliance ruptures is not only more likely to occur (Benjamin & Karpiak, 2001; Muran, Segal, Samstag, & Crawford, 1994), but also more beneficial to the treatment process, when they are efficiently resolved (Muran, Safran, Samstag, & Winston, 2005). On the contrary as a previous study has shown, when not adequately addressed, ruptures may lead to the repetition in the therapeutic interaction of the patient's typical dysfunctional interpersonal cycle (Coutinho, Ribeiro, Hill, & Safran, 2011). Thus we decided to include patients with Axis II disorders in our study in order to explore eventual differences in the dynamics of the alliance between Axis II and Axis I patients.
The present paper has two main goals: (1) to describe the alliance and alliance ruptures indicators, assessed by self-report and observational methods, over treatment; (2) to explore the relationship between the alliance ruptures and therapeutic outcomes in a sample composed by different psychopathological diagnosis.
Method
Participants
The sample consisted of 38 patient-therapist dyads in a CBT treatment condition. The initial sample consisted of 50 dyads, but we eliminated 12 dyads due to incomplete data (e.g., missing videotapes or WAI scores). Patients presented with a variety of psychopathological symptoms from Axis I (30 cases with depression and anxiety disorders) and Axis II disorders (8 cases with personality disorders from Clusters B and C). Therapy was conducted at a university clinic. Except for patients with psychotic symptoms, who were not included in the study, all the patients who underwent treatment at the clinic during the two-year period of data collection were included in the study in case they wanted to participate. All the participants signed an informed consent contract. The sample of participants was evenly comprised of university students (50%) and community members (50%). Participants ranged in age from 18 to 56 years with a mean age of 29 years (SD = 8.24 years); 68% (n = 26) were female. All participants were Caucasian Portuguese. This sample included 14 successful cases, 17 dropouts and 7 unsuccessful cases. Successful and unsuccessful cases were determined by the Global Assessment of Functioning (GAF) of the DSM-IV. We defined an unsuccessful case as one in which there was no increase on the GAF, and patient and therapist agreed on termination. In successful cases, the therapist considered that the patient had made significant clinical improvement, which was reflected in an increase on the GAF (for example, from a score of 51 to 60 (moderate symptoms) at the beginning of therapy to 61 to 70 (some mild symptoms) at termination). Dropped cases were defined as cases in which the patients decided to terminate treatment without discussing the decision with the therapist. In many of the dropped cases, patients missed a scheduled therapy session without informing the clinic.
Treatment
The treatment consisted of weekly CBT sessions, which is the therapeutic approach most frequently employed in the clinic. The treatment process for patients with personality disorders also incorporated principles of cognitive interpersonal therapy (Safran & Segal, 1990). Fifteen therapists participated in this study. Nine therapists each treated three patients; five therapists treated two patients; and one therapist treated one patient. Therapist level of experience ranged from two to eight years of clinical practice. All therapists were Caucasian and either masters or doctoral students at the university. Therapists received weekly group supervision to monitor adherence to CBT protocols. Supervisors were senior therapists and faculty members at the university.
Measures
The client version of the Working alliance - WAI- client version (Working Alliance Inventory, Horvath & Greenberg, 1989) was given to patients in the study. The WAI measures three aspects of the therapeutic alliance (goals, tasks, and bond) independent of the therapist's theoretical orientation. The internal consistency estimates for the WAI have ranged from α = .88 to α = .93 (Horvath & Greenberg, 1989; Ko-kotovic & Tracey, 1990). Considerable evidence has been obtained to support the validity of the WAI (Horvath & Symonds, 1991). The Portuguese version of the WAI has high levels of internal consistency and reliability for the overall scale and for each subscale (Machado & Horvath, 1999). The short form of the WAI, which was used in the present study, includes 17 seven-point Likert scale items anchored by 1 (never) and 7 (always); the items reflect judgments about the quality of the collaboration between patient and therapist. Higher scores reflect stronger therapeutic alliances. This questionnaire was administered at the end of each session. Internal consistency estimates for the global WAI in this sample was α = .78.
Alliance rupture events were measured by using the Rupture Resolution Rating System - 3Rs (Rupture Resolution Rating System, Eubanks, Mitchell, Muran, & Safran, 2009). The 3Rs is an observer-based system for detecting ruptures and rupture resolutions. While observing a therapeutic session, raters watch for a lack of collaboration and tension between patient and therapist. If either are present, raters determine if a confrontation rupture (when the patient moves against the therapist by expressing anger or dissatisfaction), or a withdrawal rupture (when the patient either moves away from the therapist or the patient moves toward the therapist, but in a way that denies an aspect of his or her experience) has occurred in the session. For each detected confrontation or withdrawal rupture event, raters choose a specific subtype of rupture event from a list (e.g., denial, complains about the progress of therapy). Once raters have defined the rupture, they rate its clarity and intensity on a 5-point Likert scale. Raters then assigned an overall withdrawal and confrontation score to the session. The score ranges from 1 (withdrawal/confrontation rupture(s) did not occur; not significant for the alliance) to 5 (withdrawal/confrontation rupture(s) occurred; very significant for the alliance).
A team of six judges rated 201 sessions using 3RS. Each judge rated approximately the same number of sessions (n = 33). Thirty percent of the 201 sessions (60 sessions) were rated by more than one judge to assess interrater reliability. Thus each of these 60 sessions was rated by three judges in order to calculate the intraclass correlation coefficient (ICC). We used the single-rater ICC because 70% of our data was coded by only one rater. Considering recommendations from previous studies (Shrout & Fleiss, 1979; Colli & Lingi-ardi, 2009; Dimagio et al, 2008), the interreliability values were adequate (ICC = .73 for withdrawal global ratings, ICC = .96 for confrontation global ratings).
Procedure
The study is part of a research project approved by the Scientific Council of the University of Minho. We obtained permission from the University Clinical Centre to sample its patients. Participants were informed of the requirements of their participation in the study and then signed a consent form. Research-clinicians that were in charge of intake administered the Structured Clinical Interview for DSM-IV, Axis I and Axis II, in order to determine patient diagnoses (First, Spitzer, Gibbon, & Williams, 1995). At the end of each session, patients completed the WAI and put the questionnaire in an envelope to ensure confidentiality of the answers. Participants were informed that only researchers would have access to the evaluations in an attempt to reduce social desirability effects.
Six judges received two months of weekly training sessions on how to use the observation-based 3RS system. The judges were Master and PhD-level students at the university. The training of judges included reading the manual, independently coding a different session each week, and discussing scores in team meetings. The process continued until raters achieved high reliability in ratings. Once reliable, the judges then rated 201 videotaped sessions. For example, for a case with four sessions, raters coded the first and fourth session; for a case with 20 sessions, raters coded the first, third, fourth, seventh, 11th, 13th, 15th, etc., and 20th sessions). The number of rated sessions per each case varied because 1) duration of treatment varied between cases (mean duration of treatment = 13.2 sessions; minimum = 4 sessions; maximum = 30 sessions), and 2) 10 sessions in the sample were not recorded properly due to technical problems. The number of rated sessions per case ranged from 2 (for cases with 4 sessions) and 15 (for cases with 30 sessions). Raters scored sessions from the beginning, middle, and concluding phases of treatment. We rated the first session, last session, and alternating sessions for all cases.
Data Analyses
Non-parametric smoothing spline analyses
We first performed an exploratory analysis. For that we used non-parametric regression and spline smoothing model to understand the progression of the variables (WAI, withdrawal and confrontation) as a function of diagnosis and therapy termination type. The advantage of this technique is that it does not impose a rigid function to the data. This non-parametric estimate emerged as a solution to an optimization problem: simultaneously minimizing the residual sum of squares and its second derivative (Hastie & Tibshirani, 1990). The non-parametric smoothing plots were used as exploratory tools to summarize the trend of the variables and not to make formal (test statistics) comparison between progressions.
Parametric analyses
In the next stage of the analysis we used a longitudinal parametric statistical model. The longitudinal statistical model that we used included a subject-specific random intercept, as well as a serial correlation component with an exponential correlation structure (Diggle, Heagerty, Liang, & Zeger, 2002). This model is also known as a mixed-effects model because it parametrically models the expected values and the correlation structure in the data.
Let Yij be the WAI score measured for patient i in session j. Remember that j is the session number and has by design a distance of one. However, there are situations of intermittent missing data assumed to be missing completely at random (Little & Rubin, 1987). Next, let the following be true:
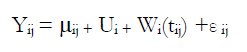
where Ui is the patient-specific random intercept with a distribution of N(0, π2), Wi,(tij) , is the stochastic process that represents the correlation between measurements within the same patient with variance σ2 and correlation structure of Corr(wi,(tij), wi,(tik)= exp (-φ| tij - tik |) and εij is the measurements error that cannot be explained by this function, with a distribution N(0, π2).
The component µij represents the expected value of WAI (i. e., µij = E [Yij]) and can be explained as the average WAI score for patient i at time j. In this case, the specified model is

This model allows us to separate the different sources of variability (i.e., the variability between participants, within participants, and measurement error). We fit the model to the data using maximum likelihood techniques and made inferences on the parameters of interest.
The data analysis was developed using R (http:llcran.r-project.org)
Results
We will present the results of the WAI ratings over treatment followed by the results of the 3RS observational system. The 3RS measures the intensity of the withdrawal and confrontation rupture markers that correspond to the global withdrawal and confrontation scores, respectively. We divided the sample according to outcome status (successful, unsuccessful, and dropped case) and diagnosis (Axis I vs Axis II) for each variable: the WAI score, the withdrawal score, and the confrontation score.
WAI and therapeutic outcome
The black solid line in Figure 1 represents the non-parametric estimate of the observed data (Keele, 2008) with 95% confidence intervals for each group. On average, there was an initial increase in the therapeutic alliance assessed by the WAI until the fifth session, after which the variability between cases increased. In successful and unsuccessful therapies, the score of the alliance continued to increase, whereas the alliance stopped increasing for dropouts.
By plotting the data in Figure 1 such that time 0 corresponded to each patient's last session, we were able to examine the status of the alliance immediately before the patient left treatment. We observed that in dropped cases, the alliance decreased before they left treatment, whereas the alliance did not decrease prior to termination for patients who did not leave treatment prematurely.
Confrontation and therapeutic outcome
In dropped cases, confrontation scores increased from the beginning to the end of treatment, whereas confrontation scores remained stable in the initial phase of therapy both for successful and unsuccessful cases (see Figure 2). When we plotted the data so that time 0 corresponded to the last session, we observed that confrontation scores for dropped cases increased directly before terminating treatment, whereas such an increase did not occur in either successful or unsuccessful cases.
Withdrawal and therapeutic outcome
We found that withdrawal scores increased for all cases in the beginning, but there were differences between cases in the concluding phase of therapy (see Figure 3). In dropout cases just before the patients terminated treatment prematurely, there was an increase in withdrawal scores, whereas these scores remained stable in both unsuccessful and successful cases.
Alliance Ruptures, Diagnosis and Therapeutic Outcome
Table 1 presents the statically significant effects of the parametric models.
Patients with Axis-I disorders began therapy with an average WAI score of 93.64, which increased 0.78 per week. Patients with Axis-II disorders began therapy with an average WAI score of 89.78, which decreased 0.22 per week (although this decrease was not significant).
Patients with Axis-I disorders began therapy with an average confrontation score of 0.90, whereas patients with Ax-is-II personality disorders began therapy with an average confrontation score of 0.95. Thus, diagnosis type distinguishes patients with regard to their initial confrontation scores. Dropouts' confrontation scores increased 0.17 per week but there was no evidence of significant variation in these scores across time for patients with either successful or unsuccessful therapies.
Finally, patients with Axis-I disorders began therapy with an average withdrawal score of 1.26 (1). Patients with Axis-II disorders began therapy with an average withdrawal score of 1.95 (2). Note that this difference corresponds to the difference between scores of 2 (Withdrawal ruptures may have occurred; possibly significant for the alliance) and 1 (Withdrawal ruptures did not occur; not significant for the alliance). Withdrawal scores increased 0.02 per week independently on the type of therapy termination.
Withdrawal scores increased in all cases, but confrontation scores only increased for dropouts.
Thus, the WAI's progression over time seem to depend on diagnosis type (i.e., Axis I vs. Axis II), whereas confrontation scores' progression seem to depend on the therapeutic outcome (i.e., dropout vs. successful therapy vs. unsuccessful therapy).
Discussion
Taken together the results of our study contributed to the understanding of the progression of three variables (self-reported quality of the alliance, withdrawal ruptures and confrontation ruptures) across time and more importantly to the way they reflect the dynamics of the therapeutic alliance in cases with Axis I vs Axis II disorders and with different outcome.
By examining the non-parametric WAI plots, we found that the WAI score increased leading up to the fifth session. After this initial increase, the variability between cases also increased. In fact after the fifth session, many patients dropped out, which suggest that patients who continued to come to therapy past the first five sessions had successfully moved beyond the initial period of alliance formation. Previous research (Horvath & Symonds, 1991) indicated that the quality of the therapeutic alliance measured during the first four sessions is the best predictor of therapeutic outcome. Other research showed that the creation of an alliance between patient and therapist occurs in early sessions (de Roten et al., 2004), but it is important to note that the therapeutic alliance must be worked on over the course of treatment in order to lead to good outcome (Kramer et al., 2009). Garfield (1994) found that treatment needs to include at least six sessions for an alliance to be formed between therapist and patient, a finding that may explain the reason why patients drop out in the initial phase of therapy. Garfield confirms the importance of strengthening the alliance even after the initial period of alliance formation. Since the beginning of the therapeutic process the occurrence of alliance ruptures can complicate the therapist's job. Thus the therapist should pay attention to the quality of the alliance as a way of preventing premature termination of therapy (Sharpless, Muran & Barber, 2010).
We found that successful therapies presented patterns of high and increasing alliance scores, which is consistent with the literature showing that both linear increase and quadratic patterns (in which the alliance scores decrease and increase again) may be associated with good outcome (Kivlighan & Shaughnessy, 2000; Stiles et al., 2004). In our study, only the linear pattern emerged; that is, we found no statistical support for a quadratic model to fit into our data, which is consistent with the results of Stiles and Goldsmith (2010), who reported a weak evidence for this pattern. This finding is also consistent with Kramer et al. (2009) who showed that a linear progression model more accurately explained the alliance for a sample of 50 patients receiving manual-based, time-limited therapy. The authors also acknowledged that the cubic pattern of alliance scores is more likely to occur in single case studies than in studies like ours, which used aggregated data based on mean scores. In addition, local V-shaped patterns (which indicate the presence of rupture-repair sequences) are more likely to be found when examining a specific dyad (Stiles et al., 2004). Likewise, we were only able to find rupture and repair sequences when we examined specific dyads more closely.
Another important finding of our study relates to the premature therapeutic termination: we found that of the three measures examined in this study (WAI, withdrawal, and confrontation), the confrontation score most closely related to therapy termination type (i.e., successful, unsuccessful, or dropout). In other words, the confrontation score was better able to discriminate between dropped cases and patients who completed treatment. This suggests that when compared with other measures, the confrontation score might be more sensitive to the alliance ruptures that lead to dropouts. This results offer an empirical support to Safran and Muran's (2000) model of alliance ruptures, namely in how there exists a difference between confrontation and withdrawal ruptures. As stated earlier in this paper, in confrontation ruptures, patients prioritize the expression of themselves at the expense of relatedness when faced with difficulties in negotiating his or her needs or desires with those of the therapist. In confrontation ruptures patients tend to express their dissatisfaction in a direct and even hostile way, which is often felt by therapists as an attack on their professional or personal abilities (Coutinho, Ribeiro, Hill, & Safran, 2011; Castonguay, Goldfried, Wiser, Raue, & Hayes, 1996). This in turn makes the therapist less able to empathize with their clients' experiences and respond to them in a flexible way in CF than in WD ruptures (Coutinho, Ribeiro, Hill, & Safran, 2011).
Our results offer additional support to the hypothesis that confrontation ruptures are thus more likely to lead to dropout if not navigated well by the therapist.
We conjecture that unsuccessful outcomes and dropped cases were the result of therapists not adequately resolving ruptures in sessions. This idea is supported by the increase in confrontation and withdrawal scores immediately before the patients' premature abandonment of therapy. The increase in rupture events prior to a patient's departure reinforces the importance of resolving ruptures in an adequate manner. Tryon and Kane (1995) also found that weakened alliances were associated with dropped cases. In addition, Muran, Safran, Samstag, and Winston (2005) found that patients in brief relational therapy (BRT), which focuses on the repair of alliance ruptures, had significantly lower dropout rates as compared to patients who received CBT. It is important to note that because we did not evaluate therapist interventions or therapist contributions to detected ruptures, we cannot confirm this possibility that the therapists were unable to resolve ruptures in unsuccessful and dropped cases. Also, it is possible that therapist's attempts to resolve ruptures actually led to more rupture events, which is especially likely in patients who withdraw when ruptures arise in therapy (Safran & Muran; 2000).
A last important finding of this study that we would like to stress was the apparently different "behavior" of the alliance in cases with Axis I disorders such as depression or anxiety, when compared with cases with Personality or Axis II disorders. The fact that Axis II patients started therapy with lower WAI scores and higher confrontation and withdrawal scores is consistent with previous theoretical and empirical evidence showing that there is a high likelihood of ruptures with such clients (Benjamin & Karpiak, 2001; Muran, Segal, Samstag, & Crawford, 1994), and personality disordered patients benefit the most from therapeutic interventions focused on alliance negotiation (Muran, Safran, Samstag, & Winston, 2005). In a qualitative study in which we explored the experience of rupture episodes of therapists and their patients with personality disorders we found that unresolved ruptures had a strong negative impact on the alliance and on_the client. (Coutinho, Ribeiro, Hill, & Safran, 2011). Moreover, we found that these events stimulated strong internal reactions in both therapists and client.
Limitations and Future Directions
The major limitation of this study has to do with characteristics of the sample, which is a naturalistic sample, that is, it is composed by a heterogeneous group of patients. We don't have a balanced sample in what concerns both the diagnosis (Axis I vs Axis II cases) and the outcome status (successful, unsuccessful and dropout). As an example we have a small number of successful cases compared to dropouts, but this may be seen as a result per se.
Another limitation has to do with the criteria used to define successful and unsuccessful cases, which was based on the clinical assessment made by the therapist at the end of the therapy. This was due to the absence of a standardized criteria of clinical significant change, which in turn relates to the fact that there was not a common symptomatic measure administered to all the cases in this convenience sample.
In future studies we think it would be important to include the therapist's perspective on the alliance (to use the therapist's version of the WAI as well). In addition and as we mentioned earlier, it would be important to analyze the process of rupture resolution and not only its emergence like we did in this study.
References
1. Bordin, E. S. (1979). The generalization of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research and Practice, 16, 252-260. [ Links ]
2. Castonguay, L. G., Goldfried, M. R., Wiser, S., Raue, P. J., Hayes, A. M. (1996). Predicting the effect of cognitive therapy for depression: a study of unique and common factors. Journal of Consulting and Clinical Psychology 64, 497-504. [ Links ]
3. Colli, A., & Lingiardi, V. (2009). The Collaborative Interactions Scale: A new transcript-based method for the assessment of therapeutic alliance ruptures and resolutions in psychotherapy. Psychotherapy Research, 19(6), 718-734. [ Links ]
4. Constantino, M. J., Marnell, M., Haile, A. J., Kanther-Sista, S. N., Wolman, K., Zappert, L., et al. (2008). Integrative cognitive therapy for depression: a randomized pilot comparison. Psychotherapy, 45, 122-34. [ Links ]
5. Corbella, S., & Botella, L. (2003). La alianza terapéutica: historia, investigación y evaluación. Anales de Psicología, 19(2), 205-221. [ Links ]
6. de Roten, Y., Fisher, M., Drapeau, M., Beretta, V., Kramer, U., Fravre, N., & Despland, J. (2004). Is one assessment enough? Patterns of helping alliance development and outcome. Clinical Psychology and Psychotherapy, 11, 324-331. [ Links ]
7. Dimaggio, G. , Nicolò, G. , Fiore, D. , Centenero, E , Semerari, A , Carcione, A., & Pedone, R. (2008). States of minds in narcissistic personality disorder: three psychotherapies analyzed using the grid of problematic states. Psychotherapy Research, 18(4), 466-480. [ Links ]
8. Coutinho, J., Ribeiro, E., Hill, C., & Safran, J. (2011). Therapists' and clients' experiences of alliance ruptures: a qualitative study. Psychotherapy Research, 21(5), 525-540. [ Links ]
9. Diggle P. J., Heagerty P., Liang K. Y., & Zeger S. L. (2002). Analysis of Longitudinal Data. (2nd ed.) Oxford: Statistical Science Series. [ Links ]
10. Eames, V., & Roth A. (2000). Patient Attachment Orientation and the Early Working Alliance- A Study of Patient and Therapist Reports of Alliance Quality and Ruptures. Psychotherapy Research, 10(4), 421-434. [ Links ]
11. Eubanks-Carter, C., Mitchell, A., Muran, J. C, & Safran, J. D. (2009). Rupture resolution rating system (3RS): Manual. Unpublished manuscript. [ Links ]
12. Eubanks-Carter, C., Muran, J. C., & Safran, J. D. (2010). Alliance ruptures and resolution. In J. C. Muran, & J. P. Barber (Eds.), The Therapeutic Alliance: An Evidence Based-Guide to Practice. (pp. 84-102). New York: Guilford Press. [ Links ]
13. Eubanks-Carter, C., Muran, J. C., Safran, J. D., & Hayes, J. A. (2011). Interpersonal interventions for maintaining an alliance. In L.M. Horowitz & S. Strack (Eds.), Handbook of interpersonal psychology: Theory, research, assessment, and therapeutic interventions. (pp. 519-531). Hoboken, NJ: John Wiley & Sons. [ Links ]
14. First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (1995). Structured Clinical Interview for DSM-IV. New York: Biometrics Research Department, New York Psychiatric Institute. [ Links ]
15. Garfield, S. L. (1994). Research on client variables in psychotherapy. In A. E. Bergin, & S. L. Garfield (Eds.), Handbook of psychotherapy and behavior change (4th ed., pp. 190-228). New York: Wiley. [ Links ]
16. Golden, B., & Robbins S. (1990). The working alliance within time-limited therapy: A case analysis. Professional Psychology: Research and Practice, 21(6), 476-48. [ Links ]
17. Gonçalves, A. (2009). Compreensão da mudança terapêutica a partir da co-construção de episódios terapêuticos significativos, Unpublished Dissertation. University of Minho. Braga. [ Links ]
18. Harper, H. (1989a). Coding Guide I: Identification of confrontation challenges in exploratory therapy. University of Sheffield, Sheffield, England. [ Links ]
19. Harper, H. (1989b). Coding Guide II: Identification of withdrawal challenges in exploratory therapy. University of Sheffield, Sheffield, England. [ Links ]
20. Hastie, T., & Tibshirani, R. (1990). Generalized additive models. Monographs on statistics and applied probability. (Vol.43) London: Chapman & Hall. [ Links ]
21. Horvath, A. O. (2011). Alliance in Common Factor Land: A view through the research lens. Research in Psychotherapy, 14(1), 121-135. http://www.researchinpsychotherapy.net. [ Links ]
22. Horvath, A. O., & Bedi, R. P. (2002). The alliance. In J. C. Norcross (Ed), Psychotherapy relationship that work (pp. 37-70). New York: Oxford University Press. [ Links ]
23. Horvath, A. O., & Greenberg, L. S. (1989). Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology, 36, 223-233. [ Links ]
24. Horvath, A. O., & Symonds, B. D. (1991). Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology, 38, 139-149. [ Links ]
25. Horvath, A. O., Del Re, A. C., Fluckiger, C., & Symonds, D. (2011). Alliance in Individual Psychotherapy. Psychotherapy, 48(1), 9-16. [ Links ]
26. Keele L. (2008). Semiparametric regression for the social sciences. London: John Wiley & Sons. [ Links ]
27. Kivlighan, D. M., & Shaughnessy, P. (2000). Patterns of working alliance development: A typology of client's working alliance ratings. Journal of Counseling Psychology, 47, 362-371. [ Links ]
28. Kokovic, A., & Tracey, T. (1990). Working alliance in the early phase of counseling. Journal of Counseling Psychology, 37(1), 16-21. [ Links ]
29. Kramer, U., De Roten, Y., Beretta, V., Michel, L., & Despland, J. (2009). Alliance patterns over the course of short dynamic psychotherapy: The shape of productive relationships. Psychotherapy Research, 19(6), 699-706. [ Links ]
30. Luborsky, L., McLellan, A. T., Woody, G. E., O'Brien, C. P., & Auerbach, A. (1985). Therapist success and its determinants. Archives of General Psychiatry, 42, 602-611. [ Links ]
31. Little, R., & Rubin, D. (1987). Statistical Analysis with Missing Data. London: John Wiley & Sons. [ Links ]
32. Machado P. P., & Horvath A. (1999). Inventário da Aliança Terapêutica - W.A.I. In M. R. Simões, M. M. Gonçalves, & L. S. Almeida (Eds.), Testes e Provas Psicológicas em Portugal (Vol.2, pp.87-94). Braga: AP-PORT/SHO. [ Links ]
33. Marmar, C. R., Weiss, D. S., & Gaston, L. (1989). Towards the validation of the California Therapeutic Alliance Rating System. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 46-52. [ Links ]
34. Martin, D. J., Garske, J. P., & Davis, M. K. (2000). Relation of the therapeutic alliance with outcome and other variables: A Meta-Analytic Review. Journal of Consulting and Clinical Psychology, 68(3), 438-45. [ Links ]
35. Muran, J. C., Safran, J. D., Gorman, B. S., Eubanks- Carter, C., & Banthin, D. (2008, June). Identifying ruptures & their resolution from post session self-report measures. Paper presented at the annual meeting of the Society for Psychotherapy Research, Barcelona, Spain. [ Links ]
36. Muran, J. C., Safran, J. D., Gorman, B. S., Samstag, L. W., Eubanks-Carter, C., & Winston, A. (2009). The relationship of early alliance ruptures and their resolution to process and outcome in three time-limited psycho-therapies for personality disorders. Psychotherapy Theory, Research, Practice, Training, 46(2), 233-248. [ Links ]
37. Muran, J. C., Safran, J. D., Samstag, L. W., & Winston, A. (2005). Evaluating an alliance-focused treatment for personality disorders. Psychotherapy, 42, 532- 545. [ Links ]
38. Muran, J. C., Segal, Z. V., Samstag, L. W., & Cawford, C. (1994). Patient pretreatment interpersonal problems and therapeutic alliance in short-term cognitive therapy. Journal of Consulting and Clinical Psychology, 62, 185-190. [ Links ]
39. Nagy, J., Safran, J. D., Muran, J. C., & Winston, A. (1998, June). A comparative analysis of treatment process and therapeutic ruptures. Paper presented at the international meeting of the Society for Psychotherapy Research, Snowbird, UT. [ Links ]
40. Patton, M. J., Kivlighan, D. M., & Multon, K. D. (1997). The Missouri Psychoanalytic Counseling Research Project: Relation of changes in counseling process to client outcomes. Journal of Counseling Psychology, 44, 189-208. [ Links ]
41. Podsakoff, P. M., MacKenzie, S. B., Lee, J., & Podsakoff, N. P. (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88(5), 879-903. [ Links ]
42. Regan, A. M., & Hill, C. E. (1992). Investigation of what clients and counsellors do not say in brief therapy. Journal of Counseling Psychology, 39, 186-174. [ Links ]
43. Rhodes, R. H., Hill, C. E., Thompson, B. J., & Elliot, R. (1994). Client retrospective recall of resolved and unresolved misunderstanding events. Journal of Counselling Psychology, 41 (4), 473-483. [ Links ]
44. Rennie, D. L. (1994). Client's deference in psychotherapy. Journal of Counselling Psychology, 41 (4), 427-437. [ Links ]
45. Safran, J. D., & Muran, J. C. (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford Press. [ Links ]
46. Safran, J. D., & Muran, J. C. (2006). Has the concept of the alliance outlived its usefulness? Psychotherapy, 43, 286-291. [ Links ]
47. Safran, J. D., & Segal, Z. V. (1990). Interpersonal process in cognitive therapy. New York: Basic Books. [ Links ]
48. Safran, J. D., Muran, J. C. & Eubanks-Carter, C. (2011), Repairing Alliance Ruptures. Psychotherapy, 48(1), 80-87. [ Links ]
49. Safran, J. D., Muran, J. C., & Samstag, L. W. (1994). Resolving therapeutic alliance ruptures: A task analytic investigation. In A. O. Horvath, & L. S. Greenberg (Eds.) The Working alliance: Theory, research and practice (pp. 225-255), New York: Wiley. [ Links ]
50. Sharpless, B. A., Muran, J. C., & Barber, J.P. (2010). In J. C. Muran, & J. P. Barber (Eds), The Therapeutic Alliance: An Evidence Based-Guide to Practice. (pp. 338-350). New York: Guilford Press. [ Links ]
51. Samstag, L. W., Batchelder, S. T., Muran, J. C., Safran, J. D., & Winston, A. (1998). Early identification of treatment failures in short-term psychotherapy: An assessment of therapeutic alliance and interpersonal behavior. Journal of Psychotherapy Practice & Research, 7, 126-143. [ Links ]
52. Shrout, P. E., & Fleiss, J. L. (1979). Intraclass Correlations: Uses in Assessing Rater Reliability. Psychological Bulletin, 86(2), 420-428. [ Links ]
53. Sommerfeld, E., Orbach, I., Zim, S., & Mikulincer, M. (2008). An in-session exploration of ruptures in working alliance and their associations with clients' core conflictual relationship themes, alliance-related discourse, and clients' postsession evaluations. Psychotherapy Research, 18, 377-388. [ Links ]
54. Stevens, C. L., Muran, J. C., Safran, J. D., Gorman, B. S., & Winston, A. (2007). Levels and patterns of the therapeutic alliance in brief psychotherapy. American Journal of Psychotherapy, 61, 109-129. [ Links ]
55. Stiles, W. B., Glick, M. J, Osatuke, K., Hardy, G. E., Shapiro, D.A., Agnew-Davies, R., Rees, A., & Barkham, M. (2004). Patterns of Alliance Development and the Rupture-Repair Hypothesis: Are Productive Relationships U-Shaped or V-Shaped? Journal of Counseling Psychology, 51, 81-92. [ Links ]
56. Stiles, W. B., & Goldsmith, J. Z. (2010). In J. C. Muran, & J. P. Barber (Eds.), The Therapeutic Alliance: An Evidence Based-Guide to Practice. (pp. 53-72). New York: Guilford Press. [ Links ]
57. Strauss, J. L., Hayes, A. M., Johnson, S. L., Newman, C. F., Brown, G. K., Barber, J., Laurenceau, J., & Beck, A. T. (2006). Early alliance, ruptures, and symptom change in a nonrandomized trial of cognitive therapy for avoidant and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology, 74(2), 337-345. [ Links ]
58. Tryon, G. S., & Kane, A. S. (1995). Client involvement, working alliance and type of therapy termination. Psychotherapy Research, 5, 189-198. [ Links ]
59. Wampold, B. E. (2001). The Great Psychotherapy Debate. Mahwah NJ: Erlbaum. [ Links ]
![]() Correspondence:
Correspondence:
Joana Coutinho
School of Psychology
University of Minho
Campus de Gualtar
4710-057 Braga (Portugal)
E-mail: ioana.coutinho@psi.uminho.com
Article received: 15-2-2013
Revision received: 23-3-2013
Accepted: 30-6-2013















