Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Anales de Psicología
versão On-line ISSN 1695-2294versão impressa ISSN 0212-9728
Anal. Psicol. vol.31 no.1 Murcia Jan. 2015
https://dx.doi.org/10.6018/analesps.31.1.168641
Group cognitive-behavioral therapy for insomnia: a meta-analysis
Terapia cognitivo-conductual grupal para el tratamiento del insomnio: metaanálisis
Beatriz Navarro-Bravo1,2, Ignacio Párraga-Martínez3, Jesús López-Torres Hidalgo4,5, Fernando Andrés-Pretel1 and Joseba Rabanales-Sotos6
1Unidad de Apoyo a la Investigación Clínica, Gerencia de Atención Integrada de Albacete, Fundación Hospital Nacional de Parapléjicos (Spain)
2Departamento de Psicología, Facultad de Medicina, Universidad de Castilla-La Mancha (Spain)
3Centro de Salud de la Roda, Gerencia de Atención Integrada de Albacete, Servicio de Salud de Castilla-La Mancha (Spain)
4Centro de Salud Zona IV de Albacete, Gerencia de Atención Integrada de Albacete, Servicio de Salud de Castilla-La Mancha (Spain)
5Departamento de Ciencias Médicas, Facultad de Medicina, Universidad de Castilla-La Mancha (Spain)
6Facultad de Enfermería, Universidad de Castilla-La Mancha (Spain)
ABSTRACT
Background: insomnia is a highly prevalent disorder in the general population and in clinical practice. Although pharmacological treatment is the most widespread choice, psychological treatment appears to have longer lasting effects. The main objective of this meta-analysis was to assess the cognitive-behavioural group therapy treatment for insomnia.
Method: a systematic search for cognitive-behavioural therapy clinical trials in Pubmed, PsycINFO, PsycARTICLES, Scielo, WOK, Cochrane, Scopus and Embase. 153 articles were reviewed, of which 9 met inclusion criteria for the metaanalysis. Adding up the data from all 9 trials, a total of 699 people completed the post-test phase.
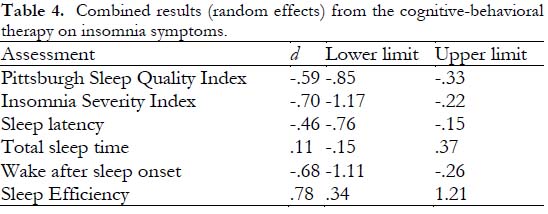
Results: after finishing cognitive-behavioural therapy, significant improvements regarding insomnia were found according to the Pittsburgh Sleep Quality Index and Insomnia Severity Index, sleep latency, wake after sleep onset and sleep efficiency. There were no significant improvements in total sleep time.
Conclusions: the results from experimental studies on cognitive-behavioural therapy as an insomnia treatment clearly suggest a positive impact on symptoms, as assessed using both validated scales and sleep diaries.
Key words: Insomnia; cognitive-behavioural therapy; meta-analysis; clinical trial.
RESUMEN
Antecedentes: el insomnio es un trastorno de elevada prevalencia tanto entre la población general como en la práctica clínica. Aunque el tratamiento farmacológico para el insomnio es el más extendido, es el tratamiento psicológico el que mantiene sus efectos a lo largo del tiempo. El objetivo principal de este metaanálisis es evaluar la eficacia de la terapia cognitivo-conductual grupal para el tratamiento del insomnio.
Método: búsqueda sistemática de ensayos clínicos de terapia cognitivo-conductual para el insomnio en Pubmed, PsycINFO, PsycARTICLES, Scielo, WOK, Cochrane, Scopus y Embase. Se revisaron 153 artículos, de los que 9 cumplieron con los criterios de inclusión para formar parte del metaanálisis. En estos 9 estudios 699 personas completaron el post-test.
Resultados: aparecen mejoras significativas con el tratamiento cognitivo-conductual para el insomnio en las escalas Pittsburgh Sleep Quality Index e Insomnia Severity Index, en latencia del sueño, en tiempo despierto después de iniciar el sueño y en eficiencia del sueño. No aparecen mejoras significativas en el tiempo total de sueño.
Conclusiones: los resultados de los estudios experimentales sobre terapia cognitivo-conductual para el tratamiento del insomnio sugieren que esta tiene un claro impacto positivo sobre los síntomas, evaluados tanto mediante escalas validadas como mediante diarios del sueño.
Palabras clave: Insomnio; terapia cognitivo-conductual; metaanálisis; ensayo clínico.
Introduction
According to the DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision), the main characteristic of insomnia is difficulty initiating or maintaining sleep, or the feeling of non restorative sleep lasting for at least one month, which causes clinically significant distress or impairment in social, occupational or other important areas of functioning (American Psychiatric Association, 2002). Although The above manual divides the sleep disorders into four big groups (primary sleep disorders, those related to other mental disorders, disorders due to a general medical condition and substance-induced sleep disorder), these distinction have disappeared in the DSM-V (American Psychiatric Association, 2013). The new edition of this manual has removed the insomnia classification "related to another mental or physical disorder" to avoid causal attributions and allows to alert about any relevant comorbidity requiring independent clinical attention. In this way, insomnia diagnosis includes primary insomnia, insomnia related to other mental disorders and insomnia due to a general medical condition. This new terminology was recommended by the NIH (National Institutes of Health) in 2005 and is being widely adopted by sleep experts. The suggestion is to make the diagnosis of "insomnia disorder" when the patient meets the insomnia criteria, regardless of the presence of other medical, psyquiatric or sleep disorders.
Insomnia is a highly prevalent disorder in the general population and in the clinical practice. It has been proven that more than a half of the primary care patients suffer sleep problems, particularly insomnia and hypersomnia (Tubtimes, Sukying and Prueksaritanond, 2009). In the same study the results showed that 35.5% of the sample had difficulties initiating sleep, 40.6% maintaining it and 24.6% suffered early awakening. Several epidemiologic studies on insomnia in the general population have shown high prevalence rates, but not many of them have applied the diagnostic criteria from the available classification manuals. This makes it difficult to distinguish whether these subjects suffer from insomnia disorder or only insomnia symptoms.
Patients with sleep difficulties have a poorer quality of life, more depression and anxiety symptoms, slower reaction times, poorer memory (Hauri, 1997) and attention deficit (Walsh et al., 1999). Of all the sleep disorders, insomnia, apnoea and restless legs syndrome have the greatest impact on concentration and memory (Ram, Seirawan, Kumar and Clark, 2010). Patients with sleep problems are more predisposed to develop hypertension, depression and cardiovascular and cerebral vascular disease. The same occurs the other way around, people with those health disorders have higher risk of suffering sleep problems (Bloom et al., 2009).
Despite the high prevalence of sleep disorders and their negative impact on daily life, evidence suggest that insomnia is underdiagnosed (Ram et al., 2010) and undertreated (Roth, 2001, get from Benca, 2005).
There are different recommended interventions in the bibliography for the treatment of sleep problems, but the most widely applied to treat insomnia are the pharmacological treatments (Rosekind and Gregory, 2010). The American Academy of Sleep Medicine establishes that both pharmacological and behavioral treatments are effective in the short term, but, only the behavioral treatment maintains its effects long term. However, there are few studies with follow-up periods longer than a year (Bootzin and Epstein, 2011).
The psychological therapies proposed for insomnia treatment include cognitive-behavioral therapy, which combines multiple approaches, such as sleep restriction, stimulus control or cognitive therapy. Both psychological and behavioral interventions are effective in treating chronic and secondary insomnia (Mongerthaler et al., 2006). Besides, regarding the type of patients, it has been proven that these therapies are also effective in elderly people and long term hypnotic consumers (Mongerthaler et al., 2006). Finally, concerning treatment method, cognitive-behavioral therapy for insomnia has shown good efficacy in groups, individually or in self-help format (Morin, Bootzin, Buysse, Edinger, Espie and Lichstein, 2006).
In the last 20 years several meta-analyses and reviews have been published on results from psychological interventions in their different formats for the treatment of sleep problems (Morin, Culbert and Schwartz, 1994; Murtagh and Greenwood, 1995; Harvey and Tang, 2003; Irwin, Cole and Nicassio, 2006; Van Straten and Cuijpers, 2009; Cheng and Dizon, 2012). These publications show results from different formats of psychological therapies for insomnia such as self-help (Van Straten and Cuijpers, 2009) or computerized cognitive-behavioral therapy (Cheng and Dizon, 2012). In most cases, the article selection was based on the description of certain symptoms by the authors, rather than on proper insomnia diagnosis (van Straten and Cuijpers, 2009). In addition, many of them have excluded papers recruiting participants suffering from other mental or physical diseases (Murtagh and Greenwood, 1995) or only selected those papers including samples of participants diagnosed with primary insomnia (Irwin, Cole and Nicassio, 2006).
In view of the characteristics of the published meta-analyses, we consider that a systematic review of the results from the psychological treatments in patients with an actual insomnia diagnosis, and not just with certain insomnia symptoms will be of interest. In addition, considering the latest changes in the DSM diagnostic criteria, we find it appropriate to include all patients with insomnia in this meta-analysis, regardless primary or secondary diagnosis. The main objective of this meta-analysis is to assess the efficacy of cognitive-behavioral therapy in group format for the treatment of insomnia, be it primary or concurrent with other medical or psychological diseases. To the best of our knowledge, this is the first meta-analysis with these characteristics.
Methods
Literature search
The literature search was performed using several data-bases. Specifically, and in this order: Pubmed, PsycINFO, PsycARTICLES, Scielo, WOK, Cochrane, Scopus and Embase. We also consulted with experts in the field. The search was performed between January and February 2012. Articles were selected as they appeared resulting from the sequence of database search, provided that they did not appear in a previous database search. Using this system, we reviewed 121 papers from Pubmed, 5 from PsycINFO or PsycARTICLES, 22 from Embase, 4 from Scopus and 1 sent by a researcher who was an expert on the subject, up to a total of 153 papers reviewed. Of those, 9 met all the inclusion criteria to be part of the meta-analysis. The search strategies used for the different databases are shown in Table 1.
Inclusion criteria
To be part of the meta-analysis the reviewed articles had to meet the following criteria: 1) Randomized controlled clinical trials (RCTs) including clinical data relevant for meta-analysis, 2) RCTs including results from insomnia treatments, 3) with a cognitive-behavioral intervention group, 4) participants older than 18 years, 5) diagnosed with primary or secondary insomnia according to DSM-IV, ICD-10 (International Classification of Diseases-10) or ICSD (International Classification of Sleep Disorders) criteria, 6) written in either English or Spanish and 7) published between 1994 and 2012. We chose 1994 as the starting date because that was the year of publication of the DSM-IV.
Data extraction
Three different researchers collaborated in the review of the 153 papers selected in the search. Each paper was independently reviewed for inclusion criteria by at least 2 researchers. Discrepancies were solved by consensus. This process reduced the number of studies included in the review to 9 which met all the established criteria. The Kappa coefficient between the different researchers was .735. We also applied the Jadad scale to check the quality of the 9 studies included in the meta-analysis. This scale was applied by 2 researchers independently (Jadad et al., 1996). The score of this scale ranges from 0 to 5. Blinding is not achievable in this type of study due to the characteristics of the interventions, therefore the highest score possible was 3. The researchers concurred regarding 91% of the items in the scale, and showed discrepancies in 4 of them (Kappa coefficient between researchers .822). The final score of these items was reached by consensus. Considering the 9 studies included in the review, 699 participants finished the post-test phase, of which 352 belonged to the cognitive-behavioral therapy group and 347 to the control group.
We gathered data regarding the authors of the papers, date of publication, intervention used, groups size, age and sex of the participants, the duration of treatments, diagnostic criteria, the inclusion and exclusion criteria and the clinical data that we found relevant for the analysis, such as: sleep latency (minutes), total sleep time (hours), wake time after sleep onset (minutes), sleep efficiency, Pittsburgh Sleep Quality Index score and Insomnia Severity Index score (post-test). The extraction of relevant clinical data was performed two times (totally independent from each other) by two different researchers. Out of the 138 values that formed the clinical data 4 were considered mistakes when we compared the results from both researchers. These mistakes were errors regarding the N value in some groups, which were solved by consensus after reviewing the original papers. The authors of the selected publications were contacted to try to complete the information from the published papers, when considered insufficient.
Analysis
The statistical analyses were performed using the software program Epidat 3-1 (Xunta de Galicia y Organización Panamericana de la salud, 2006). Due to the characteristics of the selected variables, the option "standardized means difference" was chosen for the post-test analysis.
Firstly we performed a heterogeneity analysis for all the variables (DerSimonian and Laird's heterogeneity test) followed by appropriate statistical analysis incorporating heterogeneity (random effects) to assess the variance between studies (the variance of the weighted mean of the effects from all studies multiplied by the number of studies), RI coefficient or the proportion of the total variance due to the variance between studies and variance within studies (variance between studies divided by the weighted global effect mean). Then we analyzed the combined results using the random effects model, which takes into account the heterogeneity in the analysis of the intervention effects. A reduction in the score of the two scales (Pittsburgh Sleep Quality Index e Insomnia Severity Index) is considered an improvement in sleep, as well as a reduction in the sleep lateny and in the wake after sleep onset value. However, for total sleep time and its efficiency, an increase in the score is considered an improvement. Finally, we also analyzed the publication bias (Begg and Egger tests), as well as the sensitivity to assess the influence of any of the studies in the estimation of the global effect.
In studies with more than 2 groups, we compared the cognitive-behavioral group with the placebo group.
It was not possible to find a variable that was present in all the studies for our statistical analysis. For this reason the N varied across the different variables studied.
Results
Description of the Studies Reviewed
The literature search in the different databases rendered a total of 153 papers. We rejected 97 because they did not meet all the inclusion criteria, 47 because they were not related to the main objective of the meta-analysis and 9 were accepted.
Using the Jadad scale, we checked the quality of the studies included in the meta-analysis. All of them scored between 2 and 3 and met the criteria of random allocation of the participants in the different study groups. Table 2 contains the main characteristics of the 9 studies that were included in this meta-analysis.
Heterogeneity
The DerSimonian and Laird's heterogeneity test as well as the Galbraith graph indicated heterogeneity between the studies for all the analyzed variables except the Pittsburgh Sleep Quality Index. For this reason, we used the random effects model for the combined estimation of the standardized mean differences. The heterogeneity analysis is detailed in Table 3.
Combined results
Table 4 shows the combined results, according to the random effects model, from the group cognitive-behavioral intervention for insomnia for the different variables assessed. Improvements were found for all of them excepting for the total sleep time. The same analyses were done splitting the studies into those which used a control group without any kind of intervention and those which did not do it in that way (tables 5 and 6). In addition, Figures 1-6 show the forest plots for the different study variables.





Publication bias
Regarding the presence of publication bias in the different variables studied, the p values from the Begg and Egger tests were .46 and .31 for the Pittsburgh Sleep Quality Index, .73 and .89 for the Insomnia Severity Index, .37 and .78 for sleep latency, .39 and .31 for the total sleep time, .23 and .14 for wake after sleep onset and finally, .06 and .12 for the sleep efficiency, respectively. No statistical significance was found and, therefore, we dismissed the publication bias as a threat to the validity of the results from this meta-analysis.
Sensitivity analysis
We performed sensitivity analysis to assess the influence of any of the studies in the global effect estimation. We did not find important changes in the results direction when we eliminated any of the studies. The results can be observed in Table 7.

Discussion and conclusions
In this meta-analysis we compared the post-treatment results of cognitive-behavioral therapy for insomnia, in group format, with the results from different control groups, aiming to assess the efficacy of cognitive-behavioral therapy for this sleep disorder. The different measurements employed across the studies reviewed made the N vary across variables and comparison of results difficult.
After checking the inclusion criteria, 9 studies remained in the meta-analysis. The limited number of publications is precisely due to the inclusion criteria, since the more strict they are, the fewer studies remain in the analysis. In particular, it was especially difficult to find studies performing a formal diagnosis of their participants according to the criteria from the most used manuals (DSM-IV, ICD-10 and ICSD). The number of studies included in this meta-analysis can be considered a limitation. As a consequence, it has not been possible to perform analysis of moderator variables.
We selected studies where the interventions in the experimental groups and in control groups were as similar as possible. When evaluating the results we have to take into consideration that cognitive-behavioral therapy can be very different depending on the decisions of the authors and the fact that the control groups were not exactly identical. Specifically, the control groups experienced different conditions with regard to waiting list, sleep hygiene education, treatment by their usual family physicians, placebos or stress management and wellness training. When we performed the analysis splitting the studies by the type of control group (intervention or waiting list) to try to homogenize them, we found that heterogeneity remained in half of the variables in the case of the studies with active placebo and in all the variables in the studies with passive placebo. Regarding the analysis performed taking into account the type of control group, the limitation posed by the low number of these studies should be taken in consideration, 5 with an "active" control group and only 2 with a control group "without intervention".
Considering the level of heterogeneity found in both the intervention and control groups, this meta-analysis points out the need to standardize these aspects for future research, in order to facilítate the comparison of results across studies. A similar situation occurs with the variables used to assess the sleep improvement in participants. Although most of the studies use the standard measures from sleep diaries, it has not been possible to find a variable that appears in all the selected studies, which has made the final sample used in each comparison notably lower. Specifically, 4 studies showed data from the Insomnia Severity Index, 5 from the Pittsburght Sleep Quality Index, 7 from sleep latency and wake after sleep onset and 8 from total sleep time and sleep efficiency.
After we confirmed the heterogeneity between studies in all the selected variables (except the Pittsburgh Sleep Quality Index), we decided to use the random effects model for the analysis. When we compared the combined results from the 6 variables employed in this meta-analysis we observed that cognitive-behavioral therapy generates positive results for the Pittsburg Sleep Quality Index, the Insomnia Severity Index, sleep latency, wake after sleep onset and sleep efficiency. On the contrary, in the case of the total sleep time there was no significant improvement between cognitive-behavioral therapy and the control group. These results were somewhat expected, showing that the cognitive-behavioral therapy is of great utility for the treatment of insomnia problems. The differences found in sleep latency, total sleep time, sleep efficiency and wake after sleep onset are very similar to those published in previous studies, the effect was moderate in sleep latency and wake after sleep onset and high in sleep efficiency (Irwin, Cole and Nicassio, 2006). The result from the total sleep time is not necessarily contradictory with the results from the other parameters, since the questions about satisfaction with sleep in the two scales used, the drop in sleep latency, the wake after sleep onset and the increase in sleep efficiency do not require an increase in the total sleep time. These improvements in the sleep parameters are in line with those previously found by other authors, using both empirical research as well as reviews or meta-analyses. The review by Benca (2005) suggested that the nonpharmacological therapies obtain reliable improvements in people who suffer from insomnia, with the advantage of producing minimal side effects. In conclusion, this author recommends offering behavioral therapies to all insomnia patients, both as independent therapy or combined with pharmacological therapy. Also, in the parameters for insomnia treatment published by the American Academy of Sleep Medicine (Morgenthaler et al., 2006) it was specified that psychological and behavioral treatments are effective for both primary and secondary insomnia. Specifically, these authors show that cognitive-behavioral therapy, with or without relaxation, is effective and advisable for chronic insomnia treatment, although they recommend more studies aimed to asses the efficacy of different psychological therapies alone versus combined with pharmacological therapy.
Regarding the clinical significance of the results from the articles included in our study, according to the criteria specified in the paper by Rybarczyk et al. (2005), an improvement in sleep efficiency of at least 0.5 SD can be considered clinically significant, which is the case of the results reviewed in our meta-analysis. Other criteria widely used to assess clinical relevance in sleep efficiency establishes good sleep efficiency as equal to or higher than 85% (Savard, Simard, Ivers and Morin, 2005). In this meta-analysis, we observed that in the control group only 1 out of 8 studies just reached this efficiency, whereas in the intervention group it was achieved in 5 out of 8 studies.
To assess the clinical relevance of the interventions, the recommended as criterion has been the reduction of symptoms in at least 0.5 SD, as well as reduction in the sleep latency and wake after sleep onset down to less than 30 minutes (Espie et al., 2007). In relation to the Pittsburgh Sleep Quality Index and Insomnia Severity Index, despite the fact that the improvements found were of clinical relevance (higher than 0.5 SD), in most of the cases the authors' post-test results on these scales fall into the category of bad sleepers. In the control group, sleep latency went down to less than 30 minutes in 2 out of 7 studies, whereas wake after sleep onset was not reduced in any of the 7 studies where it was measured. In the experimental group reduction below 30 minutes was achieved in 5 out of 7 studies for sleep latency and 3 out of 7 for wake after sleep onset.
In conclusion, the results from experimental studies on cognitive-behavioral therapy for insomnia treatment show a clearly positive impact on insomnia symptoms, as assessed by both validated scales and sleep diaries. Regarding future research on insomnia treatment, it would be advisable that authors reach a consensus regarding the variables to assess the results as well as the interventions that should be used. In this sense, as recommended by Morgenthaler et al. (2006), it would be interesting to study the different therapies independently, with the objective of determining the individual contribution of each of them to insomnia improvement.
Acknowledgements
The authors wish to thank Dana Epstein, Kevin Morgan, Colin Espie and Josée Savard for providing unpublished data from their studies and Carlos de Cabo for his assistance with the translation of the manuscript.
References
1. American Psychiatric Association (2002). DSM-IV-TR Manual diagnóstico y estadístico de los trastornos mentales. Barcelona: Masson. [ Links ]
2. American Psychiatric Association (2010). DSM-5. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Publishing. [ Links ]
3. Benca, R. M. (2005). Diagnosis and treatment of chronic insomnia: a review. Psychiatric Services, 56, 332-343. [ Links ]
4. Bloom, H. G., Ahmed, I., Alessi, C. A., Ancoli-Israel, S., Buysse, D. J., Kryger, M. H. et al. (2009). Evidence-based recommendations for the assessment and management of sleep disorders in older persons. Journal of the American Geriatrics Society, 57, 761-789. [ Links ]
5. Bootzin, R. R. and Epstein, D. R. (2011). Understanding and treating insomnia. Annual Review of Clinical Psychology, 7, 435-458. [ Links ]
6. *Chen, H. Y., Cheng I. C., Pan, Y. J., Chiu, Y. L., Hsu, S. P., Pai, M. F. et al. (2011). Cognitive-behavioral therapy for sleep disturbance decreases inflammatory cytokines and oxidative stress in hemodialysis patients. Kidney International, 80, 415-422. [ Links ]
7. Cheng, S. K., and Dizon, J. (2012). Computerised cognitive behavioural therapy for insomnia: A systematic review and meta-analysis. Psychotherappy and Psychosomatics, 81(4), 206-216 [ Links ]
8. *Currie, S. R., Wilson, K. G., Pontefract, A. J., and deLaplante, L. (2000). Cognitive-behavioral treatment of insomnia secondary to chronic pain. Journal of Consulting and Clinical Psychology, 68, 407-416. [ Links ]
9. *Epstein, D. R. and Dirksen, S. R. (2007). Randomized trial of a cognitive-behavioral intervention for insomnia in breast cancer survivors. Oncology Nursing Forum, 34, E51-E59. [ Links ]
10. *Epstein, D. R., Sidani, S., Bootzin, R. R., and Belyea, M. J. (2012). Dismantling multicomponent behavioral treatment for insomnia in older adults: a randomized controlled trial. Sleep, 35, 797-805. [ Links ]
11. *Espie, C. A., MacMahon, K. M., Kelly, H. L., Broomfield, N. M., Douglas, N. J., Engleman, H. M. et al. (2007). Randomized clinical effectiveness trial of nurse-administered small-group cognitive behavior therapy for persistent insomnia in general practice. Sleep, 30, 574-584. [ Links ]
12. Harvey, A. G., and Tang N. K. (2003). Cognitive behaviour therapy for primary insomnia: Can we rest yet? Sleep Medicine Reviews, 7(3), 237-262. [ Links ]
13. Hauri, P. J. (1997). Cognitive deficits in insomnia patients. Acta Neurological Belgica, 97, 113-117. [ Links ]
14. Irwin, M. R., Cole, J. C., and Nicassio, P. M. (2006). Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 25(1), 3-14. [ Links ]
15. Jadad, A.R., Moore, A., Carroll, D., Jenkinson, C. Reynolds, J.M., Gavaghan, D.J., et al. (1996). Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Controlled Clinical Trials, 17, 1-12. [ Links ]
16. *Miró, E., Lupiánez, J., Martínez, M. P., Sánchez, A. I., Díaz-Piedra, C., Guzmán, M. A. et al. (2011). Cognitive-behavioral therapy for insomnia improves attentional function in fibromyalgia syndrome: a pilot, randomized controlled trial. Journal of Health Psychology, 16, 770-782. [ Links ]
17. Morgenthaler, T., Kramer, M., Alessi, C., Friedman, L., Boehlecke, B., Brown, T., et al. (2006). Practice parameters for the psychological and behavioral treatment of insomnia: an update. An american academy of sleep medicine report. Sleep, 29, 1415-1419. [ Links ]
18. Morin, C. M., Bootzin, R. R., Buysse, D. J., Edinger, J. D., Espie, C. A., and Lichstein, K. L. (2006). Psychological and behavioral treatment of insomnia: update of the recent evidence (1998-2004). Sleep, 29, 1398-1414. [ Links ]
19. *Morin, C. M., Colecchi, C., Stone, J., Sood, R., and Brink, D. (1999). Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. Journal of the American Medical Association, 281, 991-999. [ Links ]
20. Morin, C. M., Culbert, J. P., and Schwartz, S. M. (1994). Nonpharmacological interventions for insomnia: A meta-analysis of treatment efficacy. The American Journal of Psychiatry, 151(8), 1172-1180. [ Links ]
21. Murtagh, D. R., and Greenwood, K. M. (1995). Identifying effective psychological treatments for insomnia: A meta-analysis. Journal of Consulting and Clinical Psychology, 63 (1), 79-89. [ Links ]
22. National Institutes of Health (2005). National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13-15, 2005. Sleep, 28, 1049-1057. [ Links ]
23. Ram, S., Seirawan, H., Kumar, S. K., and Clark, G. T. (2010). Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath, 14, 63-70. [ Links ]
24. Rosekind, M. R. and Gregory, K. B. (2010). Insomnia risks and costs: health, safety, and quality of life. American Journal of Managed Care, 16, 617-626. [ Links ]
25. Roth, T. (2001). New developments for treating sleep disorders. Journal of Clinical Psychiatry, 62 (10), 3-4. [ Links ]
26. *Rybarczyk, B., Stepanski, E., Fogg L., Lopez, M., Barry, P., and Davis, A. (2005). A placebo-controlled test of cognitive-behavioral therapy for comorbid insomnia in older adults. Journal of Consulting and Clinical Psychology, 73, 1164-1174. [ Links ]
27. *Savard, J., Simard, S., Ivers, H., and Morin, C. M. (2005). Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. Journal of Clinical Oncology, 23, 6083-6096. [ Links ]
28. Tubtimes, S., Sukying, C., and Prueksaritanond, S. (2009). Sleep problems in out-patients of primary care unit. Journal of the Medical Association of Thailand, 92, 273-278. [ Links ]
29. Van Straten, A., and Cuijpers, P. (2009). Self-help therapy for insomnia: A meta-analysis. Sleep Medicine Reviews, 13(1), 61-71. [ Links ]
30. Walsh, J. K., Benca, R. M., Bonnet, M., and et al. (1999). Insomnia: assessment and management in primary care. American Family Physician, 59, 3029-3037. [ Links ]
31. Xunta de Galicia y Organización Panamericana de la salud (2006). EPIDAT. Programa para el análisis epidemiológico de datos tabulados. Versión 3.1. (Computer software). [ Links ]
![]() Correspondence:
Correspondence:
Beatriz Navarro Bravo
Edificio Unidad de Investigación
Complejo Hospitalario Universitario de Albacete
C/ Laurel s/n. 02008 Albacete (Spain)
E-mail: bnavarrob@sescam.jccm.es
Article received: 11-2-2013
Revision received: 6-11-2013
Accepted: 26-11-2013