Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Anales de Psicología
versão On-line ISSN 1695-2294versão impressa ISSN 0212-9728
Anal. Psicol. vol.31 no.3 Murcia Out. 2015
https://dx.doi.org/10.6018/analesps.31.3.193571
Social support during childhood cancer treatment enhances quality of life at survival
El apoyo social durante el cáncer infantil favorece la calidad de vida en periodo de supervivencia
Carmina Castellano-Tejedor1,2, Marta Pérez-Campdepadrós2,3, Lluís Capdevila2, Constantino Sábado-Álvarez3 y Tomás Blasco-Blasco2
1 Departamento de Psiquiatría, Hospital Universitari Vall d´Hebron, CIBERSAM-Fundació Institut de Recerca Vall d´Hebron, Barcelona (España).
2 Departamento de Psicología Básica, Universitat Autónoma de Barcelona, Bellaterra (España).
3 Servicio de Oncología y Hematología Pediátrica. Hospital Universitari Vall d´Hebron, Barcelona (España).
This work has been carried out thanks to the pre-doctoral research grant (FI00286UAB) awarded to the first author of the manuscript in 2007 and, partly, thanks to the funding provided by the Spanish Ministerio de Ciencia e Innovación (PSI2011-29807-C03-01/PSIC).
ABSTRACT
Background: Health-related quality of life (HRQoL) in cancer has been related to several protective and risk factors such as perceived social support (PSS) and coping. However, their effects on HRQoL once patients are in survivorship have not been fully described in pediatric samples.
Objective: To describe and explore the relationship between HRQoL in survivorship and some factors (PSS, coping) present while active treatment. Methods: Cross-sectional study. Forty-one pediatric cancer survivors answered HRQoL measures referred to survivorship, as well as PSS and coping measures referred to treatment period.
Results: The discriminant function obtained succeeds to correctly classify 78% of the sample. Survivors who showed high HRQoL were those who, in the hardest moment while hospitalization, perceived satisfactory emotional support (from nurses) and did not deploy a wide range of active coping resources to cope with stressful events (only social action coping strategy showed a significant relationship with HRQoL).
Conclusions and implications: Considering these outcomes, educational and counseling interventions to strengthen patients' social networks and supportive relationships are recommended, specially, among health providers (nurses). These results highlight the importance of not overlooking opportunities to address the emotional needs of patients while hospitalization, since a positive and endurable effect has been observed at survivorship.
Key words: Childhood cancer; health-related quality of life; social support; coping.
RESUMEN
Introducción: La calidad de vida en relación a la salud (CVRS) en cáncer se ha relacionado con distintos factores de riesgo y protección tales como el apoyo social percibido (ASP) y el afrontamiento. Sin embargo, la investigación acerca de los efectos de dichos factores sobre la CVRS de supervivientes pediátricos sigue siendo no concluyente.
Objetivo: Describir y explorar la relación entre CVRS en periodo de supervivencia y factores presentes durante el periodo de hospitalización (ASP y afrontamiento).
Métodos: Diseño transversal. 41 supervivientes de cáncer infanto-juvenil respondieron medidas de CVRS en referencia al periodo actual de supervivencia, así como medidas de ASP y afrontamiento en relación al periodo de hospitalización.
Resultados: La función discriminante obtenida logró clasificar correctamente al 78% de la muestra. Los supervivientes con mayores puntuaciones en CVRS, fueron aquellos que, en los peores momentos durante su hospitalización, percibieron un apoyo emocional satisfactorio (por parte del personal de enfermería) y no desplegaron un gran número de recursos de afrontamiento para hacer frente al evento estresante (sólo la estrategia de afrontamiento de acción social mostró relación estadísticamente significativa con CVRS).
Conclusiones e implicaciones: Considerando estos resultados, parece adecuado el llevar a cabo intervenciones de tipo psicoeducativo destinadas a fortalecer la red de apoyo social, sobre todo por parte del personal sanitario (enfermería). Estos resultados ponen de manifiesto la importancia de considerar todas las oportunidades para abordar las necesidades emocionales de los pacientes durante su hospitalización, ya que se ha observado que esto puede tener un efecto positivo perdurable en periodo de supervivencia.
Palabras clave: Cáncer infanto-juvenil; calidad de vida en relación a la salud; apoyo social; afrontamiento.
Introduction
Childhood cancer presents a unique challenge to patients and their families. The impact of the disease and its treatment threatens the successful acquisition of age-appropriate developmental milestones, as well as health-related quality of life (onwards, HRQoL) outcomes in survivorship (Cantrell, 2011). In this sense, pediatric oncological patients must face a complex treatment that can generally range from six months to several years. Moreover, most treatments might involve intrusive and painful techniques (e.g. surgery, bone marrow transplants, etc.) and can require numerous hospitalizations and follow-up appointments (Langeveld, Stam, Grootenhuis & Last, 2002). Thus, the adolescent's daily routines are usually disrupted over an extended period of time, even long after the end of treatment (Henderson, Friedman & Meadows, 2010). Consequently, HRQoL and adjustment could be hampered. HRQoL includes physical and mental health self-perceptions of the individual and their correlates; including health risks and conditions, functional status, social support and socioeconomic status (Ravens-Sieberer et al., 2008). Some scientific accounts have also described that cancer involves a period of identity re-construction, aimed to integrate the experience into one's self-concept and new life philosophy (Wallander, Varni, Babani, Banis & Wilcox, 1989; Zebrack, 2000). To these challenges, other additional illness-related stressors must be added: understanding the diagnosis, the treatment, the prognosis and adapting to all of it, as well as to possible related side-effects. Moreover, the adolescent will have to establish a relationship with health providers and his/her peers at the hospital. Dealing with such stressful situation may be overwhelming for many adolescents and their own coping resources could be insufficient.
Social support has been stated as a relevant factor influencing adaptation outcomes when facing stressful circumstances of diverse nature (Caplan, 1974; Cohen & Wills, 1985; Cutrona & Russell, 1990; McDougall & Tsonis, 2009) and also, it has been recognized as an important determinant of HRQoL among diverse clinical samples, suffering from both acute and chronic diseases (Maslow & Chung, 2013; McDougall & Tsonis, 2009; van Horn & Kautz, 2007; Yarcheski, Mahon & Yarcheski, 2001). It is important to note that when speaking about social support, the emotional, informative and instrumental dimensions of it are being considered (Bloom, 1982; House & Khan, 1985).
In research, conceptualizations of social support are usually divided into two models: 1) structural models and 2) functional models (Bloom, 1982; Cohen & Wills, 1985). Studies have mainly focused on studying the effects (functional models) of perceived social support (onwards, PSS), more than the simple availability or the extension (e.g. number of family members, social roles, etc.) of social support networks (structural models). Although the size of the network has proved to be directly related to higher HRQoL (Bloom, 2008), this article is focused on PSS of adolescent cancer survivors, also related to better psychosocial functioning in several studies (Decker, 2007).
The primary source of social support for pediatric patients is their parents who act as main caregivers (Haluska, Jessee & Nagy, 2002). However, in many cases, caregivers could experience even greater distress than patients themselves (Ljungman et al., 2003), hampering the provision of effective support to patients. Such situation may increase vulnerability of both patients and their caregivers (Grootenhuis & Last, 1997; Patenaude & Kupst, 2005). Patients could identify symptoms of distress in their caregivers and this could lead to a decrease in their search for social support, undermining the potential positive effects of it. Fortunately, many practitioners such as oncologists, hematologists and nurses form close relationships with patients and their families due to the extend period of time of close contact and intense treatment, becoming the primary source of social support for them while hospitalization. Physicians' communication and care behavior can greatly influence patients' HRQoL (Arora, 2003; Stewart, 1995). In this sense, some empirical accounts have demonstrated that good communication skills during treatment -characterized by an open, clear and a compassionate style-, promotes favorable outcomes (e.g. higher satisfaction with care and adherence to treatment) and foster HRQoL in patients. However, the support provided by nurses and practitioners (mainly, of an informative and emotional nature) usually finishes at the end of the treatment and most patients could experience a certain lack of support at discharge and at survival period. At this phase, this supportive role falls back on the family (McKenzie & Curle, 2012).
Nevertheless, the protective and buffering effect of PSS provided by the medical staff during the active phase of treatment could have a lasting effect on HRQoL once patients' are at survival. To our knowledge, there are no studies trying to explore this relationship; however, this possibility has been suggested in a work that describes a theoretical model of resilience in childhood cancer (Castellano et al., 2014). According to this model, HRQoL at survival will depend on the interaction of different risk and protective factors during the phase of treatment, among which PSS and coping are included.
For all these reasons, this study had two main objectives: firstly, to describe PSS, coping and HRQoL of adolescent's survivors of childhood cancer and secondly, to determine the relationship between global HRQoL outcomes in survivorship and some protective factors (coping strategies and PSS) present while active treatment.
Methods
Study design
Descriptive study with retrospective (PSS and coping during hospitalization) and cross-sectional measures (HRQoL).
Ethical considerations
The whole study was carried out at the University Hospital Vall d'Hebron, pediatric Oncological & Hematological Department. Ethical approval was obtained from the hospital ethics committee board. Informed consent was obtained before participation from each participant (and his/her parents/caregivers) after they have received an information sheet and oral explanations about the aims and characteristics of the study. This research complies with the Helsinki Convention norms and its subsequent amendments.
Participants
Inclusion criteria required that: (a) adolescents had been diagnosed with cancer (excluding central nervous system tumors in order to reduce bias due to possible cognitive impairment) after the age of 8. Survivors diagnosed after the age of 8 were chosen because of the need to ensure that these patients had the appropriate cognitive maturity during cancer treatment so that reliable memories of their illness and personal experiences could be obtained. (b) To be 13-20 years old at the time of the study (both included), (c) to be off-treatment ≥ 1 year at the time of the study, and (d) to have a follow-up appointment at the reference hospital between May 2009-May 2010. Survivors with learning disabilities or psychopathology diagnosed before the first primary oncological diagnosis were excluded from the study.
Measures
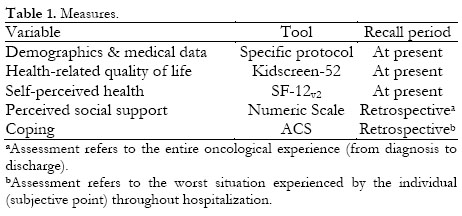
Table 1 summarizes the assessment tools administered to the sample.
Socio-demographic and illness-related data
Socio-demographic data (gender, age, education, people living at home) and illness-related data (oncological diagnosis, type of treatment, bone marrow transplant, relapse, second malignancy, age at the first diagnosis and time passed since first diagnosis) were retrieved from patients and their parents in a joint semi-structured interview and completed from medical records.
HRQoL
HRQoL was assessed with the Spanish self-reported version of the Kidscreen-52 questionnaire (Ravens-Sieberer et al., 2008). The Kidscreen consists of 52 items in 10 subscales: physical well-being, psychological well-being, mood & emotions, self-perception, autonomy, parent relations & home life, social support & peers, school environment, social acceptance/bullying and financial resources. T-scores (M = 50, SD = 10) can be calculated for each dimension stratified by age and gender. Higher scores indicate better HRQoL. The questionnaire has acceptable levels of reliability and validity. Cronbach's alpha values ranged from .77 to .89 (Ravens-Sieberer et al., 2008).
Self-perceived Health (SPH)
The Short Form-12 version 2 (SF-12v2) was used to assess overall SPH status measuring 8 domains of health: physical functioning, role limitations because of physical health, bodily pain, general health perceptions, vitality, social functioning, role limitations because of emotional problems and mental health. Responses are scored from 0 to 100 (M = 50, SD = 10) and the physical component summary scale and the mental component summary scale can be calculated. Higher scores indicate better SPH (Rebollo, 2008; Vilagut et al., 2008). Cronbach's alpha for each SF-12v2 components were satisfactory (PCS = .85, MCS = .78); (Vilagut et al., 2008).
Perceived social support
To assess PSS while hospitalization, a 2-item visual analogue scale was developed. The first item assessed perceived emotional support (e.g. displays of love, empathy, trust, etc.) and requested the adolescent to think back and to focus in the whole oncological experience, from diagnosis to survival, and rate to what extent (0 = none to 10 = very much) he/she considers to have received satisfactory emotional support from each of the people listed: parents, other relatives, friends, practitioners (oncologists and/or hematologists), nurses and others (e.g. teachers, social workers, psychologists, etc.). The second item had the same structure, however, it was focused on informative support (e.g. useful information to cope with the disease and/or related issues). In both cases, the score was obtained for each item (and for each source of support indicated) from the direct value rated by the adolescent. Perennial issues in the measurement of PSS include whether it is the number of social contacts a person has, or their quality (McDowell, 2006). The emphasis now commonly lies with assessing the functional and qualitative aspects of relationships rather than their number or type. Numeric scales serves to these purposes as some research has demonstrated (McDowell, 2006). This ad hoc numeric scale has been developed considering this theoretical approach (Barron-Lopez & Sanchez-Moreno, 2001; McDowell, 2006) and provides information about social support sources and self-reported satisfaction with support. It covers both the quantity of social contacts and their supportive quality rated by the respondent (Barron-Lopez & Sanchez-Moreno, 2001).
Coping
Coping was assessed with the Spanish version of the Adolescent Coping Scale (ACS); (Perena & Seisdedos, 1996). The ACS is a self-report checklist inventory that consists of 79 items scored on a 5-point Likert scale (ranging from 1 = doesn't apply or don't do it to 5 = used a great deal), which assesses the use of 18 coping strategies by adolescents in dealing with stress (Frydenberg & Lewis, 1993). Higher scores indicate higher use of these coping strategies (20-29 = unused strategy, 30-49 = strategy rarely used, 50-69 = strategy used sometimes, 70-89 = strategy used frequently, 90-105 = strategy used a great deal). The ACS provides normative data stratified by gender (Perena & Seisdedos, 1996). Cronbach's alpha for the specific form is .75 (Frydenberg & Lewis, 1993).
Procedure
Survivors eligible for the study were contacted via telephone by a qualified researcher in psychology. In this initial contact, they were informed about the purpose of the study and asked for participation. If they agreed to participate, an assessment appointment was scheduled. The assessment was conducted by the main researcher of the study, in a hospital office for a 45-minute session. The same psychologist provided oral and written information about the study when participants came to the assessment appointment and informed consent was obtained. Demographic and medical data was collected jointly with the patient and his/her parents (or the main caregiver identified) and completed with hospital records. Finally, parents were requested to remain in the waiting room while the patient completed the questionnaires.
Statistical analyses
This study provides descriptive statistics (M, SD, range, frequencies) about patients' demographic, clinical characteristics, PSS, coping strategies, HRQoL and SPH. To examine differences between groups regarding demographics, clinical characteristics and independent variables, correlational analyses and non-parametric tests were performed (X2 and Mann-Whitney U tests). A discriminant analysis (stepwise method) was performed to examine which variables classify the better the sample of survivors regarding their overall HRQoL. Independent variables for this analysis were selected according to the existence of significant differences between HRQoL groups (see descriptive outcomes section, below). The significance level for all the tests was set at p ≤ .05.
Results
Sample characteristics
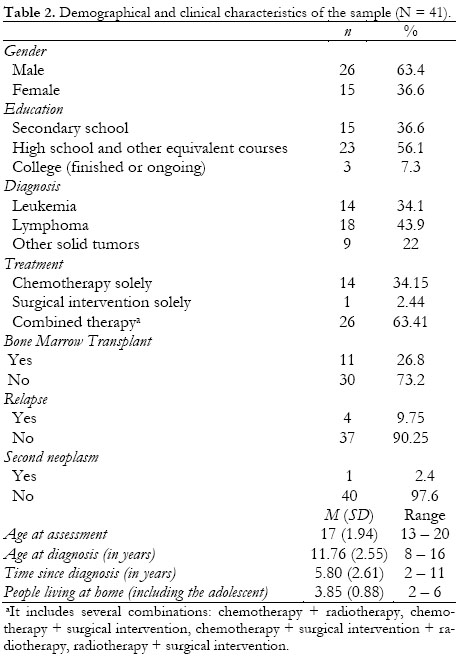
Initially, 93 potential participants were identified throughout hospital records, 46 of them not reaching or having not scheduled follow-up appointments in the reference hospital. Thus, 47 families were approached by telephone to explain the study and ask for participation. Among those who agreed to participate, an assessment appointment was scheduled. Finally, 41 adolescents enrolled into the study. Refusal rate was 12.77% (N = 6).
The reasons for rejection were: 1) not willing to talk about cancer and remember all the experience (n = 4, 66.6%), 2) lack of time for the assessments (n = 1, 16.7%) and 3) the family did not attend the assessment appointment despite having accepted to on the telephone contact (n = 1, 16.7%). Demographical and clinical characteristics of survivors are displayed in Table 2.
Descriptive outcomes
No significant differences were found between groups for any of the demographic and clinical characteristics considered in this study (gender, age at assessment, age at diagnosis, time since diagnosis). Therefore, these variables were not included in the subsequent analyses.
HRQoL and SPH outcomes for each dimension according to groups described above are displayed in Table 3. For the whole sample, all HRQoL mean scores were within normative values (M = 50±10); (Ravens-Sieberer et al., 2008). No significant differences were found between HRQoL scores and clinical characteristics included in this study (see Table 2).
The nominal categorical variable overall HRQoL (high vs. average) was created taking into account the total standardized scores of each subject for each of the HRQoL and SPH dimensions. Thus, those who scored above 40 points in all dimensions and above 60 points in at least one dimension (+ one SD) were considered as survivors with a high HRQoL (H-HRQoL). By contrast, those who rated within the average range (between 40 and 60 points, ± one SD) or below 40 points (- two SD) in any dimension were considered as survivors with an average HRQoL (A-HRQoL). Following these criteria, 18 cases (43.9%) became part of the H-HRQoL group and 23 (56.1%) of the A-HRQoL group. PS S for adolescents is displayed in Table 4. As it can be observed, mean values for both HRQoL groups were above 6.7 points for both types of PSS (emotional and informative support) and for all people listed, except for the informative support provided for friends and other relatives where lower mean scores were indicated. Globally, emotional support from family members was high (M = 18.49, SD = 1.99, range 12-20) followed by that received from healthcare professionals (M = 16.76, SD = 2.92, range 8-20) and a little bit lower from friends and other persons (M = 15.64, SD = 3.13, range 11-20). Regarding information, higher mean scores were obtained in the case of healthcare professionals (M = 15.68, SD = 4.31, range 0-20) compared to that received from family members (M = 12.29, SD = 4.90, range 1-20) or friends and other people (M = 12, SD = 5.15, range 7-20). No statistically significant differences were observed between HRQoL groups, except for emotional support provided by nurses that shows a strong tendency towards statistical significance (p = .056).
Survivors' coping is displayed in Table 5. In our sample, 9 coping strategies were rarely used (30-49 points; invest in close friends, not coping, tension reduction, social action, ignore the problem, self-blame, keep to self, seek spiritual relief and physical recreation), 5 coping strategies were used sometimes (50-69; social support, focus on solving the problem, seek to belong, wishful thinking and seek professional help) and the coping strategy of focus on the positive was used frequently (70-89 points). The use of the remaining coping strategies depended on the group: seek relaxing diversion worry coping strategies were used sometimes (50-69 points) for the H-HRQoL group and frequently used (70-89) for the A-HRQoL group respectively, and work hard and achieve was rarely used for the H-HRQoL and sometimes used for the A-HRQoL group. Significant differences were found between HRQoL groups for: work hard and achieve, seek spiritual relief, seek relaxing diversions and social action, with H-HRQoL group showing significantly lower use of all coping strategies mentioned.
Discriminant analysis
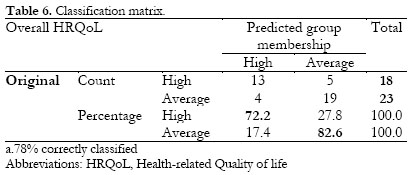
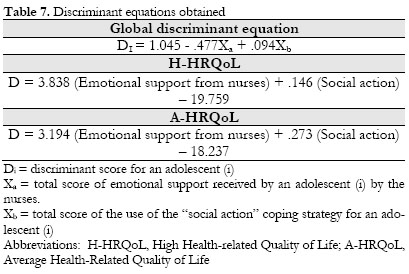
A discriminant analysis was performed with overall HRQoL as criterion variable and the following factors: emotional support from nurses (U = 137.500, p = .560), work hard and achieve (U = 118, p = .019), social action (U = 95, p = .003), seek spiritual relief (U = 116, p = .015) and seek relaxing diversions (U = 125.500, p = .031).
As a result, a discriminant function was obtained (Wilks lambda = .679; Χ2(2) = 14.683; p = .001); (Eigenvalue = .472; canonical correlation = .566).
The canonical linear discriminant function obtained succeeds to correctly classify 78% of cases with regard to HRQoL groups (H-HRQoL vs. A-HRQoL) with two variables: the coping strategy of social action and the perceived emotional supportfrom nurses (see Table 6). Table 7 summarizes the statistical indexes for the discriminant function obtained for the variable overall HRQoL (Box M = 11.270; p = .014).
Discussion
This study was designed as a twofold exploratory investigation. Firstly, it was aimed to describe PSS, coping and HRQoL of adolescent's survivors of childhood cancer; and secondly; to test the relationship between overall HRQoL outcomes in survivorship and some protective factors during treatment (coping strategies and specially PSS), as proposed by the model of Castellano and colleagues (Castellano et al., 2014).
Globally, regarding the former objective, survivors' PSS seems satisfactory since mean scores are above 7 points for each person listed, except for the informative support from friends and other relatives. It must be taken into account that in this developmental stage, peers are crucial and during hospitalization they can serve as a link with the adolescent's previous normal life outside the hospital. For this reason, more than providing useful information to cope with cancer, friends could have a buffering effect providing emotional support and they could help the adolescent to disconnect from hospital routines and treatments. A similar role could be attributed to other relatives (e.g. cousins, grandparents, etc.). As pointed out in some reviews in the field (Bloom, 2008; van Horn & Kautz, 2007), in our sample, emotional support was mainly provided by parents and other relatives and, with little difference, by health providers during hospitalization. As expected, informative support was primarily covered by practitioners and, in a second front, by other people (5 cases mentioned social workers, teachers and psychologists), parents and nurses. These results agree with previous studies (Arora, 2003; Haluska et al., 2002; Stewart, 1995). Nurses spend a lot of time taking care of patients and trying to establish boundaries to facilitate compliance and adherence to treatments (Forsey, Salmon, Eden & Young, 2013). Therefore, they regularly talk to patients and their parents about whatever they need, which often includes emotional needs (Forsey et al., 2013). As a consequence, close relationships are usually developed and they could become an important asset in the social network of patient's support providers. In fact, there is a lot of literature on nursing role providing emotional support to both patients and their relatives, and how it could turn professionals vulnerable to burnout or emotional distress (Trufelli et al., 2008). The impact of support provided by parents has not appeared to be crucial on survivors' HRQoL; however, this could be explained because of the lack of variability in this variable. All parents were very present while hospitalization and all of them provided full support to their children, as the latter stated (Decker et al., 2007; Haluska, Jessee & Nagy, 2002). Additionally, this impact could be also modulated by the mixed feelings parents could experience in front of this stressful situation (Schor, 2003). In such situations, the wellbeing of children is inextricably linked to their parents' emotional well-being and, in some cases, the incidence of behavior problems among pediatric patients attests to some families' inability to cope with the situation or the negative effect that depending again on parents could have on adolescents' self-perception and well-being (Norberg & Boman, 2007; Schor, 2003).
Coping strategies were quite similar between HRQoL groups and statistically significant differences were only found for 4 out of 18 coping strategies assessed (seek relaxing diversions, work hard and achieve, seek spiritual relief and social action). For all coping strategies mentioned, the group of H-HRQoL showed lower mean scores, pointing out a lower deployment of coping resources compared to the average group (A-HRQoL). Some research has pointed out a certain pattern of disengagement among pediatric patients with cancer (Phipps, 2007; Phipps, Steele, Hall & Leigh, 2001). In this sense, an interesting concept in this field is the repressive adaptative style (Gil, 2005; Phipps & Srivastava, 1997). Repressive coping style has been defined by the combination of low trait anxiety and high defensiveness in an individual (Weinberger, Schwartz & Davidson, 1979). The biopsychosocial processes and mechanisms that involve repressive coping style lead to both adaptive and maladaptive pathways. Accordingly, the literature shows contradictory results. On the adaptive side, repressive coping style has been associated with reduced psychopathology and increased resilience (Bonanno, Moskowitz, Papa & Folkman, 2005; Phipps, 2007). On the maladaptive side, it has been associated with increased medical risks, limited self-awareness, denial, alexithymia and worse interpersonal relationships (Weinberger & Schwartz, 1990). Considering these results, these predominantly independent trajectories have succeeded to gain enough empirical evidences that it seems reasonable to integrate them. Although repressive coping style has been traditionally understood as an individual trait style coping, there is some research that has pointed out that this model fails to provide explanations to other complex processes when facing severe stressors (Myers, 2010). In this sense, repressive coping style has been also understood as a posttraumatic or stressor adaptation mechanism that affords both protective and risk factors within distinct domains (Pedersen & Zachariae, 2010; Weiss, 2009). The resulting model (based on findings from resilience and posttraumatic adaptation research) includes two components: 1) the development and stability of repressive coping style in response to environmental stressors and 2) major life trajectories for repressors. We believe that our coping results could be partially understood from this perspective (Weiss, 2009).
With regard to HRQoL outcomes, the sample showed satisfactory values and within the normative range (40 and 60 points). Moreover, the group of H-HRQoL scored significantly higher in 8 out of 10 HRQoL dimensions, and 1 out of 2 SPH dimensions. Previous research has reported similar findings (Cantrell, 2011; Castellano et al., 2009). On the face of these results, it seems that pediatric cancer survivors succeed to achieve satisfactory HRQoL and adjustment outcomes, or even higher than healthy population. Possible explanations have been addressed on literature (Castellano et al., 2014; Noeker, 2012). Briefly, resilience and positive psychology (including posttraumatic growth and adaptation frameworks) could reveal changes in survivors selfperception, life values, priorities and own resources in front of stressful and difficult situations, and this could have implications on their self-perceived health and quality of life in the aftermath of trauma (Noeker, 2012; Wallander et al., 1989; Zebrack, 2000).
The discriminant analysis supports the thesis that PSS and a controlled used of social-type coping strategies while hospitalization, are of crucial importance for patients (Maslow & Chung, 2013; McDougall & Tsonis, 2009; van Horn & Kautz, 2007; Yarcheski et al., 2001). In this sense, a valid and genuine patient-health provider relationship during the active phase of treatment has shown to have lasting effects on HRQoL survivorship, as stated by other authors (Anderzen-Carlsson, Kihlgren, Skeppner, & Sorlie, 2007; Eilerstsen et al., 2009; Kiernan, Meyler & Guerin, 2010). Specifically, in the present study it has been found that those survivors perceiving higher emotional support from nurses were also those who showed higher HRQoL scores in survivorship. Consequently, care behavior from health providers has proved to have direct effects on HRQoL of patients beyond hospitalization (Anderzen-Carlsson et al., 2007; Arora, 2003; Eilersten et al., 2009; Kiernan et al., 2010; Stewart, 1995). Besides, a restricted use of the coping strategy of social action (characterized by a personal seek for social resources to handle personal, developmental age issues and cancer-related issues and worries) has proved to be also effective to cope with cancer during the process and helps to adjust and foster HRQoL once patients' are in survivorship. Although we believe that the timely use of a repressive coping (strategies such us not coping or keep to self) may be favorable to preserve HRQoL at mid or long term, we cannot exclude from our results that survivors with a repressive style of coping (more stable and not limited to certain stressors) were precisely those who showed better HRQoL at survival. Additionally, it can't be ruled out that self-perceived HRQoL might follow a certain general coherent pattern throughout lifespan in relation to stressful circumstances. This coherent general pattern could be related to other more stable individual characteristics not considered in the present research.
In any case, the resulting equation from these two variables -emotional support from nurses and social action- succeed to correctly classify 78% of cases, with a difference of 10.4% between those who achieve high HRQoL (72.2%) and those with average HRQoL (82.6%).
Conclusions
In line with previous researches and the suggested resilience model for pediatric cancer survivors (Castellano et al., 2014), our results highlight that adolescent survivors of childhood cancer who show satisfactory or high values on HRQoL, are those who in the hardest moments while hospitalization perceived satisfactory social support (emotional) and did not deploy a wide range of coping resources to cope with stressful events (only a restricted use of social action appears to be a relevant coping strategy), which agrees with previous research on repressive coping and adaptation (Phipps et al., 2001; Phipps, 2007). That is to say, to rely on their social networks -such as parents, other relatives and health providers- has proved to be effective to cope with severe chronic stressful conditions such as cancer (Decker, 2007; Haluska et al., 2002). The fact that nurses have appeared as key professionals to provide emotional support to adolescents has been explained in previous researches (Hegelson & Cohen, 1996), outlining that this collective is very present in patients' routines while hospitalization and assume most of the care and medical procedures of their treatment (e.g. more hours of close contact, more times entering into the room, etc); (Askins & Moore, 2008).
Clinical implications
To sum up, we believe that identifying a set of variables that can predict with a fairly high probability the HRQoL of cancer patients once they are in remission, could be extremely useful in clinical contexts; for instance, to design and target early interventions. Therefore, and according to our results, the intervention aimed to increase and foster HRQoL of this population of survivors, should be targeted to promote and provide social support throughout the process, rather than to promote a particular coping style. Additionally, repressive coping during hospitalization may be favorable to HRQoL at mid-long term.
These results are in line with previous studies that highlight the importance of training health professionals to provide social support throughout the oncological process and therefore, helping families to cope with the shock of the diagnosis and subsequent treatment demands, until its end with either remission or palliative care (Askins & Moore, 2008; Decker, 2007; Dixon-Woods, Findlay, Young, Cox & Heney, 2001; Haluska et al., 2002; Ljungman et al., 2003; Maru, Gibson & Hinds, 2013; Norberg & Boman, 2007; Schor, 2003). It is expected that this will lead to a higher emotional adjustment and arguably, better coping with the various stressful situations to which both, patient and parents and/or primary caregivers may be subjected. Ultimately, it is hoped that this will have a positive impact on their final HRQoL.
Limitations
Longitudinal investigations without retrospective measures would be necessary to confirm the associations found and provide more conclusive results to the research question proposed. Besides, more specific research on repressive style and adaptation among pediatric cancer survivors should be carried out. Additionally, an all-encompassing model adding parents' experiences and variables would be preferable. However, to include all these variables in future studies, higher sample size is required.
Acknowledgments
The authors specially thank all the adolescent cancer survivors for their disinterested contribution to this study.
References
1. Anderzen-Carlsson, A., Kihlgren, M., Skeppner, G., & Sorlie, V. (2007). How physicians and nurses handle fear in children with cancer. Journal of Pediatric Nursing, 22, 71-79. [ Links ]
2. Arora, N. K. (2003). Interacting with cancer patients: the significance of physicians' communication behavior. Social Science & Medicine, 57(5), 791-806. [ Links ]
3. Askins, M. A., & Moore, B. D. (2008). Psychosocial support of the pediatric cancer patient: lessons learned over the past 50 years. Current Oncology Reports, 10(6), 469-476. [ Links ]
4. Barrón-López, A., & Sánchez-Moreno, E. (2001). Estructura social, apoyo social y salud mental. Psicothema, 15(1), 17-23. [ Links ]
5. Bloom, J. R. (1982). Social support, accommodation to stress and adjustment to breast cancer. Social Science & Medicine, 16(14), 1329-1338. [ Links ]
6. Bloom, J. R. (2008). Improving the health and well-being of cancer survivors: past as prologue. Psychooncology, 17(6), 525-532. [ Links ]
7. Bonanno, G. A., Moskowitz, J. T., Papa, A., & Folkman, S. (2005). Resilience to loss in bereaved spouses, bereaved parents, and bereaved gay men. Journal of Personality & Social Psychology, 88(5), 827-843. [ Links ]
8. Cantrell, M. A. (2011). A narrative review summarizing the state of the evidence on the health-related quality of life among childhood cancer survivors. Journal of Pediatric Oncology Nursing, 28(2), 75-82. [ Links ]
9. Caplan, G. (1974). Psychosocial processes and Stress: Theoretical formulation. International Journal of Health Services, 4, 471-482. [ Links ]
10. Castellano, C., Blasco, T., Pérez-Campdepadrós, M., & Capdevila, L. (2014). Making sense of resilience: a review from the field of paediatric psychooncology and a proposal of a model for its study. Anales de Psicología, 50(3), 865-877. [ Links ]
11. Castellano, C., Blasco, T., Oller, A., Pérez-Campdepadrós, M., Sánchez de Toledo, J., & Capdevila, L. (2009). Quality of life in adolescent survivors of childhood cancer. Medicina Clínica (Barc), 155(20), 783-786. [ Links ]
12. Cohen, S., & Wills, T. (1985). Stress, Social Support and the buffering hypothesis. Psychological Bulletin, 98, 310-357. [ Links ]
13. Cutrona, C. E., & Russell, D. Type of social support and specific stress: toward a theory of optimal matching. In saranson, I. G., Saranson, B. R., & Pierce, G. R. (Eds.), Social support: An international view (p. 319-366). New York: Wiley, 1990. [ Links ]
14. Decker, C. L. (2007). Social support and adolescent cancer survivors: a review of the literature. Psychooncology, 16(1), 1-11. [ Links ]
15. Dixon-Woods, M., Findlay, M., Young, B., Cox, H., & Heney, D. (2001). Parents accounts of obtaining a diagnosis of childhood cancer. Lancet, 357, 670-674. [ Links ]
16. Eilerstsen, M. E. B., Kristiansen, K., Reinfjell, T., Rannestad, T., & Indredavik, Vik. T. (2009). Professional collaboration -support for children with cancer and their families- focus group interview -a source of information and knowledge- professionals' perspectives. Journal of Interprofessional Care, 23, 356-368. [ Links ]
17. Frydenberg, E, & Lewis, R. Adolescent Coping Scale: Administrator's manual. Hawthorn, Australia: The Australian Council for Educational Research, 1993. [ Links ]
18. Forsey, M., Salmon, P., Eden, T., & Young, B. (2013). Comparing doctors' and nurses' accounts of how they provide emotional care for parents of children with acute lymphoblastic leukaemia. Psychooncology, 22(2), 260-267. [ Links ]
19. Gil, A. (2005). Repressing distress in childhood: a defense against health-related stress. Child Psychiatry & Human Development, 56(1), 27-52. [ Links ]
20. Grootenhuis, M. A., & Last, B. F. (1997). Adjustment and coping by parents of children with cancer: a review of the literature. Support Care Cancer, 5(6), 466-484. [ Links ]
21. Haluska, H. B., Jessee, P. O., & Nagy, M. C. (2002). Sources of social support: adolescents with cancer. Oncology Nursing Forum, 29(9), 1317-1324. [ Links ]
22. House, J. S., & Khan, R. L. Measures and concepts of social support. In Sheldon Cohen & S Leonard Syme (Eds.), Social support and Health (p. 83-108). New York: Academic Press, 1985. [ Links ]
23. Hegelson, V. S., & Cohen, S. (1996). Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychology, 15(2), 135-148. [ Links ]
24. Henderson, T. O., Friedman, D. L., & Meadows, A. T. (2010). Childhood cancer survivors: transition to adult-focused risk-based care. Pediatrics, 126(1), 129-136. [ Links ]
25. Kiernan, G., Meyler, E., & Guerin, S. (2010). Psychosocial issues and care in pediatric oncology. Cancer Nursing, 55, 12-20. [ Links ]
26. Langeveld, N. E., Stam, H., Grootenhuis, M. A., & Last, B. (2002). Quality of life in young adult survivors of childhood cancer. Support Care Cancer, 10(8), 579-600. [ Links ]
27. Ljungman, G., McGrath, P. J., Cooper, E., Widger, K., Ceccolini, J., Fernández, C. V., Frager, G., & Wilkins, K. (2003). Psychosocial needs of families with a child with cancer. Journal of Pediatric Hematology & Oncology, 25(3), 223-231. [ Links ]
28. Maru, M., Gibson, F., & Hinds, P. S. (2013). Pediatric oncology nursing research goes global. Cancer Nursing, 56(5), 339. [ Links ]
29. Maslow, G. R., & Chung, R. J. (2013). Systematic review of positive youth development programs for adolescents with chronic illness. Pediatrics, 131(5), e1605-1618. [ Links ]
30. McDougall, J., & Tsonis, M. (2009). Quality of life in survivors of childhood cancer: a systematic review of the literature (2001-2008). Support Care Cancer, 17(10), 1231-1246. [ Links ]
31. McDowell, I. Measuring health. A guide to rating scales and questionnaires (3rd Ed.), Social Health (p.150-203). Owford University Press: New York, 2006. [ Links ]
32. McKenzie, S. E., & Curle, C. (2012). "The end of treatment is not the end": parents' experiences of their child's transition from treatment for childhood cancer. Psychooncology, 27(6), 647-654. [ Links ]
33. Myers, L. B. (2010). The importance of the repressive coping style: findings from 30 years of research. Anxiety Stress Coping, 22(1), 3-17. [ Links ]
34. Noeker, M. (2012). Survivors of pediatric cancer. Developmental paths and outcomes between trauma and resilience. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschultz, 55(4), 481-492. [ Links ]
35. Norberg, A. L., & Boman, K. K. (2007). Parents' perceptions of support when a child has cancer: a longitudinal perspective. Cancer Nursing, 30(4), 294-301. [ Links ]
36. Patenaude, A. F., & Kupst, M. J. (2005). Psychosocial functioning in pediatric cancer. Journal of Pediatric Psychology, 30(1), 9-27. [ Links ]
37. Pereña, J., & Seisdedos, N. Manual ACS: escalas de afrontamiento para adolescentes (ACS Manual: Adolescent Coping Scales). Madrid, Spain: Ediciones TEA; 1996. [ Links ]
38. Phipps, S. (2007). Adaptative style in children with cancer: implications for a positive psychology approach. Journal of Pediatric Psychology, 32(9), 1055-1066. [ Links ]
39. Phipps, S., & Srivastava, D. K. (1997). Repressive adaptation in children with cancer. Health Psychology, 16(6), 521-528. [ Links ]
40. Phipps, S., Steele, R. G., Hall, K., & Leigh, L. (2001). Repressive adaptation in children with cancer: a replication and extension. Health Psychology, 20(6), 445-451. [ Links ]
41. Pedersen, A. F., & Zachariae, R. (2010). Cancer, acute stress disorder, and repressive coping. Scandinavian Journal of Psychology, 51(1), 84-91. [ Links ]
42. Ravens-Sieberer, U., Gosch, A., Rajmil, L, Erhart, M., Bruil, J., Power, M., Duer, W., Auguier, P., Cloetta, B., Czemy, L., Mazur, J., Czimbalmos, A., Tountas, Y., Hagguist, C., Kilroe, J., & The KIDSCREEN Group. (2008). The KIDSCREEN-52 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Value in Health, 11(4), 645-658. [ Links ]
43. Rebollo, P. (2008). Utilización del "grupo SF" de los cuestionarios de calidad de vida (SF-36, SF-12 y SF-6D) en el marco de ensayos clínicos y en la práctica clínica habitual. Medicina Clínica (Barc), 130(19), 740-741. [ Links ]
44. Schor, E. L., & American Academy of Pediatrics Task Force on the Family (2003). Family pediatrics: report of the Task Force on the family. Pediatrics, 111(6 Pt 2), 1541-1571. [ Links ]
45. Stewart, M. A. (1995). Effective physician-patient communication and health outcomes: a review. Canadian Medical Association Journal, 152(9), 1423-1433. [ Links ]
46. Trufelli, D. C., Bensi, C. G., García, J. B., Narahara, J. L., Abrao, M. N., Diniz, R. W., Miranda, Vda, C., Soares, H. P., & del Giglio, A. (2008). Burnout in cancer professionals: a systematic review and meta-analysis. European Journal of Cancer Care (Engl), 17(6), 524-531. [ Links ]
47. Van Horn, E. R., & Kautz, D. (2007). Promotion of family integrity in the acute care setting: a review of the literature. Dimensions of Critical Care Nursing, 26(3), 101-109. [ Links ]
48. Vilagut, G., Valderas, J. M., Ferrer, M., Garin, O., López-García, E., & Alonso, J. Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: componentes físico y mental. Medicina Clínica (Barc), 130(19):726-735. [ Links ]
49. Wallander JL, Varni JW, Babani L, Banis, H. T., & Wilcox, K. T. (1989). Family resources as resistance factors for psychological maladjustment in chronically ill and handicapped children. Journal of Pediatric Psychology, 14(2), 157-173. [ Links ]
50. Weinberger, D. A., & Schwartz, G. E. (1990). Distress and restraint as superordinate dimensions of self-reported adjustment: a typological perspective. Journal of Personality, 58(2), 381-417. [ Links ]
51. Weinberger, D. A., Schwartz, G. E., & Davidson, R. J. (1979). Low-anxious, high-anxious, and repressive coping styles: psychometric patterns and behavioral and physiological responses to stress. Journal of AbnomalPsychology, 88(4), 369-380. [ Links ]
52. Weiss, E. Toward an integrative model of repressive coping style in stress adaptation. (Dissertation). Pro Quest, UMI Dissertation Publishing, 2009. [ Links ]
53. Yarcheski, A., Mahon, N. E., & Yarcheski, T. J. (2001). Social support and well-being in early adolescents. Clinical Nursing Research, 10(2), 163-181. [ Links ]
54. Zebrack, B. J. (2000). Cancer survivor identity and quality of life. Cancer Practice, 8(5), 238-242. [ Links ]
![]() Correspondence:
Correspondence:
Carmina Castellano Tejedor.
Department of Psychiatry,
Hospital Universitari Vall d'Hebron
Institut de Recerca Vall d'Hebron,
Passeig de la Vall d'Hebron 119-129,
P.O. Box 08035, Barcelona (Spain).
E-mail: ccastellano@vhebron.net,
castellano.teiedor@yahoo.es
Article received: 27-02-2014;
revised: 07-10-2014;
accepted: 22-10-2014