Introduction
Hypochondriasis, currently called Illness Anxiety Disorder (APA, 2013), is characterized by preoccupation and fear of having a serious illness in the absence of somatic symptoms that explain it, and by a high level of anxiety and alarm about one's health status.
Cognitive models of the disorder propose that dysfunctional beliefs about body symptoms and illness are the basis for the development of hypochondriacal concerns (Abramowitz & Braddock, 2008; Rachman, 2012; Warwick & Salkovskis, 1990; Taylor & Asmundson, 2004). Based on these models, it has been hypothesized that such beliefs may lead a person to selectively attend to information that confirms his or her idea that he or she is suffering from a serious disease and, at the same time, ignore information suggesting that his/ her state of health is satisfactory (Chorot & Martínez-Narváez, 2012).
Several studies support these hypotheses, showing that individuals with high health anxiety hold dysfunctional beliefs about illness to a greater extent than those who are not concerned about their health status (for a review see Marcus, Gurley, Marchi & Bauer, 2007). Other authors have analyzed these beliefs. In an early paper on this topic, Barsky, Coeytaux, Remy, Sarnie, and Cleary (1993) found that people with high health anxiety considered that having good health was comparable to an ideal state with no symptoms or discomfort. In our context, Castañeiras (2001) found a similar result in people with a primary diagnosis of hypochondriasis (DSM-IV-TR criteria), as these patients presented overvalued ideas about health. Hadjistavropoulos et al. (2012) found that dysfunctional beliefs about illness predicted symptoms of health anxiety and a poor response to medical re-insurance in both healthy and sick people. It has also been observed that people who hold dysfunctional beliefs about illness also think that serious diseases are more frequent than they actually are (Marcus & Church, 2003), tend to overestimate the likelihood and danger of suffering from them (Fergus, 2014; Gellatly & Beck, 2016; Scarella et al., 2016), and think they have less control over the recurrence of the disease (Ferguson, 2000). In addition, other studies show that these people are highly intolerant of uncertainty (Abramowitz & Moore, 2007; Abramowitz, Schwartz & Whiteside, 2002; Boelen & Carleton, 2012; Deacon & Abramowitz, 2008; Fergus & Valentiner, 2011; Reuman et al, 2017), maintain dysfunctional beliefs about medical recommendations and adherence to treatment, and often show a skeptical attitude towards preventive treatments (Christensen, Moran & Wiebe, 1999; Fulton, Marcus & Merkey, 2011). Finally, other research has shown that these dysfunctional beliefs often promote catastrophic interpretations of body symptoms and sensations (e.g., Hadjistavropoulos, Craig & Hadjistavropoulos, 1998; Haenen, de Jong, Schmidt, Stevens & Visser, 2000; Marcus, 1999; Rief, Hiller & Margraf, 1998).
A second postulate of cognitive models of hypochondriasis suggests that early illness-related experiences, either their own or others', as well as negative experiences with health services, lead to dysfunctional beliefs about symptoms, illness, and health behaviors. Some studies indirectly support this idea by showing that experiences related to the illness and/or health services, both their own and vicarious, play an important role in the development and maintenance of hypochondriasis (e.g., Noyes et al., 2005; Noyes et al., 2002; Noyes, Happel & Yagla 1999; Robbins & Kirmayer, 1996; Weck, Bleichhardt,& Hiller, 2009; Weck, Harms, Neng, & Stangier, 2011).
However, as far as we know, very few studies specifically explore the initial hypothesis, that is, that there is a relationship between early experiences with illness and/or health services and the development of dysfunctional beliefs characteristic of hypochondriasis. In a relatively recent study, Alberts, Hadjistavropoulos, Sherry, and Stewart (2016) found that people whose parents had previously or currently suffered from a serious illness had higher levels of health anxiety and held the belief that they were more likely to have an illness than individuals with healthy parents.
Given the paucity of empirical studies on these aspects, we planned to analyze to what extent sharing similar experiences related to illness and health has an effect on the adoption of the dysfunctional beliefs characteristic of hypochondriasis. The immediate family context seemed particularly suitable for analyzing this aspect. The main objective of this paper was to explore whether the parents' dysfunctional beliefs about illness and thoughts are related to their offspring's beliefs about these same aspects. A secondary objective was to analyze the relationships between these beliefs and indicators of emotional distress considered important in relation to hypochondriasis in the specialized literature: health anxiety and depression.
Method
Participants and procedure
Fifty undergraduate psychology students (Universitat de València) were invited to participate in a family study of hypochondriasis in exchange for minor academic compensation. Interested students attended a seminar where the psychopathology and current treatments for hypochondriasis were presented and the purpose of the research was explained. Prior to the seminar, attendees signed an informed consent form and completed a questionnaire on socio-demographic data, along with the self-reports described below. After the seminar, each participant received two envelopes, one for her/his mother and one for his/her father, which included an informed consent form and the same evaluation protocol they had completed. For the evaluation of the relatives, the following instructions were given: (1) students had to evaluate two first-degree relatives, preferably their mother and father; (2) they had to briefly explain the study in terms similar to the following: "this is a study about ideas people have about health and illness, and to what extent these ideas are shared in the family"; (3) they had to emphasize the anonymity of the data, indicating that the participant's personal identity could not be inferred from the data; (4) they had to briefly explain how to complete each questionnaire and be accessible while the participant filled out the questionnaire in order to solve possible doubts; (5) once the questionnaires were completed, they had to check that there were no unanswered items, and then put the questionnaires in the envelope in front of their relative, who, once the envelope was closed, signed his/her name on the back to ensure anonymity.
Forty students returned questionnaires from at least one of their parents (57% mothers, 43% parents). Forty university students (65% women), 36 mothers, and 27 fathers made up the final sample. The average age of the students was 21.88 (SD = 4.345) years. In the case of the parents, the average age of the mothers was 51.94 years (SD = 6.334), and the average age of the fathers was 54.37 (SD = 5.759) years. The majority of the students had a medium socio-economic level (65%) and were single (95%). In the case of the parents, more than a quarter had completed university studies (37% mothers, 26% fathers), their socio-economic level was medium (58% mothers, 48% fathers), and the majority were married (75% mothers 62% fathers).
Instruments
Beck Depression Inventory-II (BDI-II, Beck et al., 1996, Spanish version: Sanz, Perdigón & Vázquez, 2003). This is a 21-item self-report instrument that assesses depressive symptoms. Items are answered on a 5-point response scale ranging from 0 (absence of the mood evaluated) to 3 (intense presence of the mood). The possible range of scores is from 0 to 63. Internal consistency was excellent (α = .90) in the sample evaluated.
Health Anxiety Inventory (SHAI, Salkovskis, Rimes, Warwick & Clark, 2002, Spanish version: Caballo, 2005). This is an 18-item self-report designed to assess health anxiety, regardless of the current health status. It is composed of two scales (1: Likelihood of becoming ill and 2: Negative consequences of illness). The items are answered on a Likert scale from 0 to 3, and they evaluate aspects such as concern for health, the monitoring of changes and bodily sensations, and/or fear of the consequences of suffering from a serious illness. In this study, the total SHAI score was used. The internal consistency in the sample was satisfactory (α = .87).
Obsessive Beliefs Inventory- Revised (ICO-R,Belloch et al., 2010). It is a 50-item self-report that assesses dysfunctional beliefs about one's thoughts that are involved in the development and/or maintenance of obsessive-compulsive disorder and other related disorders. The items are evaluated on a Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). Items are grouped into 8 scales. In this study, only the two scales most directly linked to health anxiety were considered: intolerance of uncertainty generated by the thoughts (6 items) and overestimation of threat associated with the thoughts (8 items). In the study sample, the internal consistency was satisfactory: α = .78 and α = .83, for the two scales, respectively.
Irrational Health Belief Scale (IHBS, Christensen et al., 1999, translated and re-translated into Spanish for the present study). This self-report assesses the individual's tendency to value health-related information in an irrational or distorted manner. It includes 20 cartoons that describe different situations or experiences related to health. Participants have to indicate to what degree their thinking would be similar to what is described in the vignette if they were in the same situation, responding on a 5-point Likert scale (1 = It does not look anything like what I would think - 5 = I would think exactly the same thing). In the study sample, the internal consistency was acceptable (α = .77).
Statistical analysis
Statistical analyses were carried out using the statistical package SPSS for Windows v. 20. Central tendency (M) and dispersion (SD) statistics were analyzed. Student t tests with Levene corrections were used to analyze the differences between two independent groups (e.g., fathers vs. mothers, sons vs. daughters). Effect size was estimated with Cohen's d statistic. To study the associations between the variables included in the study, Spearman's correlation coefficient was calculated because the data did not follow a normal distribution. The minimum level of statistical significance required was p ≤ .05.
Results
Preliminary analysis: differences between groups
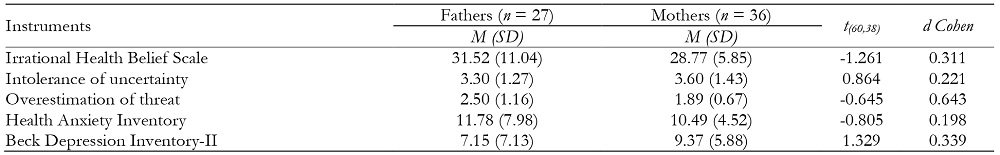
First, we analyzed whether fathers and mothers differed significantly on the assessed variables. The results indicated that there were no significant differences between the parents on any of the variables (Table 1). The differences between sons and daughters on the different variables were also analyzed, and daughters scored higher on intolerance of uncertainty (Table 2).
Relationships between the dysfunctional beliefs of parents and offspring about illness and thoughts
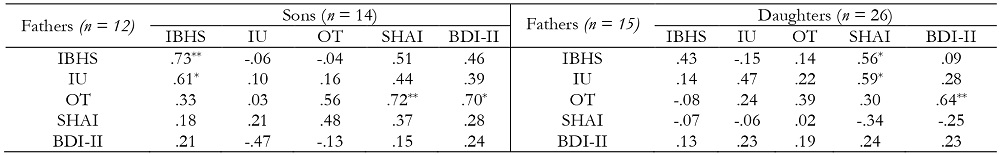
Although no significant differences were observed between the parents in the variables evaluated, correlation analyses were carried out separately to analyze the differential contributions of each. Results are shown in Table 3.
In the case of the fathers, a moderate and significant association was found between their dysfunctional beliefs about illness and overestimation of threat and the beliefs hold by their offspring, without differentiating the sex. However, in the case of the mothers, no significant relationship was observed between their beliefs and those of their offspring. Given these results, which suggest a greater influence of fathers on their offspring's beliefs about illness, the analyses were again conducted, but differentiating the sex of the parents and their offspring.
Table 2. Differences in beliefs, health anxiety, and depression between sons and daughters.
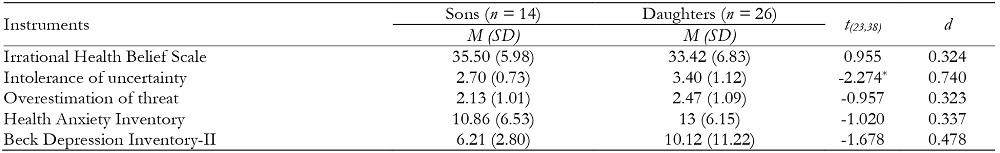
*p ≤ .05; **p ≤ .01
Fathers' dysfunctional beliefs about illness were clearly associated with those of their sons. In the case of daughters, a similar trend was observed (r 2 = .18), although the association was not statistically significant. Associations were also found between the overestimation of threat of fathers and their sons (r 2 = .31) and daughters (r 2 = .15), which, although not statistically significant, did share significant rates of variance. A similar result was obtained for intolerance of uncertainty: although the association between the scores of fathers and daughters was not significant, the shared variance was high (r 2 = .22).
Regarding mothers, the most relevant data is the absence of significant relationships between their beliefs about illness and those of their sons and daughters.
Associations between dysfunctional beliefs about illness and thoughts and indicators of emotional distress of parents and their offspring
To meet the second objective, and in line with the previous analyses, independent correlation analyses were carried out taking into account the sex of the parents and their offspring. The results are shown in Table 4.
Table 3. Relationships between parents' and offspring's beliefs about thoughts and illness.

*p ≤ .05;**p ≤ .01
Table 4. Correlations between parents' and their offspring's dysfunctional beliefs about thoughts and illness, and indicators of health anxiety and depression
*p ≤ .05;**p ≤ .01.IBHS= Irrational Health Belief Scale; IU= Intolerance of uncertainty; OT= Overestimation of threat;SHAI= Short Health Anxiety Inventory; BDI-II= Beck Depression Inventory-II
Significant and high correlations were found between fathers' intolerance of uncertainty and sons' dysfunctional beliefs about illness, and between fathers' overestimation of threat and sons' health anxiety and depressive symptoms.
High correlations were also found between fathers' dysfunctional beliefs about illness and intolerance of uncertainty and daughters' health anxiety. In addition, as in the case of fathers and sons, a significant correlation was observed between fathers' overestimation of threat and daughters' depressive symptoms.
No significant associations were found between mothers and their children on the variables assessed.
Discussion
The first objective of this study was to assess whether parents and their offspring share dysfunctional beliefs about illness and thoughts.
Before addressing this objective, no differences were observed between fathers and mothers on the variables evaluated, although differences were observed in the younger generation (sons vs. daughters), specifically on intolerance of uncertainty, where daughters scored higher than sons. In the past decade, several studies have addressed the role of intolerance to uncertainty in hypochondriasis, given that it is a belief with transdiagnostic value that is present in various anxiety and depressive disorders (Belloch, 2012; McEvoy & Mahoney, 2012). Regarding gender differences in this variable, our data coincide with those of Robichaud, Dugasa and Conway (2003), who found that women scored higher than men on intolerance of uncertainty.
When analyzing the beliefs about illness, intolerance of uncertainty, and overestimation of threat of parents and their offspring, the results showed that fathers' beliefs about illness and overestimation of threat were closely related to those of their offspring. However, these associations were not found for the maternal figure. Cognitive-behavioral theories of hypochondriasis postulate that patients with hypochondriasis hold dysfunctional beliefs about illness (e.g., Kellner, 1985, 1989; Warwick & Salkovskis, 1990). In addition, the tendency of patients with hypochondriasis to overestimate the likelihood and danger of disease is particularly important in these theories (e.g., Olatunji, Deacon, & Abramowitz, 2009; Rachman, 2012, Reuman et al., 2017; Wheaton, Berman, Franklin, & Abramowitz, 2010). Our results seem to indicate that fathers play an essential role in the transmission of these beliefs to their descendants, at least in our context. Consequently, and according to cognitive-behavioral theories, the beliefs held by fathers, but not mothers, could be a vulnerability factor in the development of hypochondriacal symptoms in their offspring. Similar results were found in studies on obsessive-compulsive disorder, where the relationship between the beliefs of parents and their offspring were analyzed in relation to "not just right" experiences (Sica et al., 2013) or "looming vulnerability" (Riskind, Sica, Bottesi, Ghisi, & Kashdan, 2017). These studies found that fathers' beliefs played a more relevant role than mothers' in predicting their offspring's beliefs.
When associations between the beliefs about illness, intolerance of uncertainty, and overestimation of threat of parents and their offspring were studied taking into account the sex of the offspring, the results followed the same trend as in the total sample. More specifically, an important association was found between the dysfunctional beliefs about illness of fathers and sons, and a similar tendency was observed in the case of daughters. There was also a tendency toward an association between the overestimation of threat beliefs of fathers and their offspring, and between the intolerance of uncertainty of fathers and daughters. In the case of the mothers, no significant associations were found. These results are congruent with those obtained with the total sample, and they reinforce the approach that, in offspring's hypochondriacal symptoms, for both sons and daughters, fathers' beliefs have more weight than mothers'.
The second objective of the study was to analyze whether the dysfunctional beliefs assessed (i.e., beliefs about illness, overestimation of threat, and intolerance of uncertainty) were related to indicators of emotional distress associated with hypochondriasis, such as health anxiety and depression. The dysfunctional beliefs about illness held by fathers and sons are related, as the data show. Moreover, fathers' intolerance of uncertainty is related to their sons' beliefs about illness, and fathers' overestimation of threat is not only related to their sons' overestimation of threat, but also to their sons' health anxiety and depressive symptoms. In the case of fathers and daughters, associations have been found between fathers' dysfunctional beliefs about illness and intolerance of uncertainty and their daughters' health anxiety. In addition, as with sons, there is an association between fathers' overestimation of threat and daughters' depressive symptoms. These data are, in general, consistent with those referred to by other authors, and they highlight the important role that both intolerance of uncertainty (e.g., Abramowitz & Moore, 2007; Abramowitz et al., 2002; Boelen & Carlenton, 2012; Deacon & Abramowitz, 2008; Fergus & Valentiner, 2011; Reuman et al., 2017) and overestimation of threat (e.g., Fergus, 2014; Gellatly & Beck, 2016; Olatunji et al., 2009; Rachman, 2012; Reuman et al., 2017; Scarella et al., 2016; Wheaton et al., 2010) play in hypochondriacal symptoms. Again, no significant associations were found in the assessed variables between mothers and their offspring. Therefore, our data suggest that fathers' influence would not be limited to beliefs because it would also be present in health anxiety and depression, which are considered fundamental elements of hypochondriasis.
This study has limitations. First, the sample size was small, making it difficult to generalize the data, although an attempt was made to correct this aspect by using a small number of variables in the statistical analyses. Secondly, only correlational analyses were carried out of the variables under study, which makes it impossible to examine potential causal relationships between them.
Finally, it is important to note that, although this is a preliminary study, the results obtained could be particularly useful in initiating a new line of research on the family transmission of dysfunctional beliefs about illness and its influence on the development and maintenance of hypochondriasis. As far as we know, there are no family studies of hypochondriasis that assess these aspects (i.e., beliefs and symptoms shared by parents and their offspring). Family studies have mainly focused on analyzing the presence of hypochondriacal symptoms in relatives of patients diagnosed with hypochondriasis. In fact, Noyes' group (2002, 2005) found a higher frequency of sick family members or friends in patients with hypochondriasis compared to people without the disorder, and they noted that people who reported being very concerned about the illness for at least one month had a family history of severe illness, unlike those who reported not having been concerned about the illness. These studies have also focused on analyzing the family and life history of patients diagnosed with hypochondriasis, primarily assessing the existence of previous traumatic events in childhood or adolescence related to illness or health services (e.g., Noyes et al., 1999, 2002, 2005; Robbins & Kirmayer, 1996; Weck et al., 2009; Weck et al., 2011). Other studies have examined whether the offspring of physically ill parents have increased health anxiety (Alberts et al., 2016). Therefore, we believe that studies like the one presented here can help to explain the role played by the family in the acquisition of beliefs about illness, which are considered key factors in hypochondriasis vulnerability models.











 text in
text in