Introduction
Stigma, and self-stigma faced by people with severe mental disorder (SMI) is one of the main concerns regarding mental health these days. Moved by this need, several awareness programs have been set in order. Most of these programs include three main elements: contact with users of mental health services, talks with professionals and protest or recognition activities (Comission of the European Communities, 2005; Evans-Lack, Henderson, Thornicroft & McCrone, 2013; Oexle et al. 2018; See me Scotland, 2006).
Unfortunately, stigma and self-stigma do not limit only to those directly affected by the illness, but their consequences affect their relatives and close people as well (Corrigan & Nieweglowski, 2019). In addition, we must take into consideration that after the psychiatric reform, relatives have mostly assumed the role of caregivers for people with mental illness. This situation causes important consequences within the family, both on the physical level (fatigue, exhaustion) and on the economic and social levels (Johnson et al., 1999; Navarro, 2013; Persson & Rossin-Slater, 2018).
At the same time, relatives suffer from some psychological consequences, such as stigma by association, which consists on an extension of this concept, suffering from social withdrawal and marginalization. The risks for physical and psychological health are evident, and they worsen because those affected by it cannot see an improvement of their situation in the future (Reever, Mathieu, Dennis & Gitlin, 2004). This burden and its repercussions represent a widespread phenomenon in different societies and cultures (Shibre et al., 2001; Silver, 1999; Yildiz, Kiras, Incedere & Abut, 2018).
Nevertheless, researchers have not paid too much attention to the repercussions of self-stigma in relatives of people with SMI in different spheres of their lives thus far (Rusch et al., 2014). On this matter, we must point out that internalized stigma or self-stigma can be defined as the subjective process of acceptation of the social stigma (Corrigan & Watson, 2002). The main sources of stigma and self-stigma among the relatives of people with mental illness are the statements generally made by the population about these issues (Corrigan & Nieweglowski, 2019).
Thus, on a social level, the belief that the raising and family interaction patterns, mainly inside the family group, are responsible for the development of illnesses in children, is maintained. For its part, the media sometimes encourage a gutter and distorted image of these illnesses, helping to create and perpetuate this misunderstanding within the society. Moreover, the lack of information and vague and inaccurate information that many times relatives have about the aetiology puts them in a situation of vulnerability, which increases the credibility of these theories and affirmations that blame them (Thornicroft et al., 2016). Thereby, relatives would internalise and assume their role as an etiologic agent, associated to feelings of guilt and shame (Muñoz, Perez-Santos, Crespo & Guillen, 2009).
Likewise, among the wide variety of strategies, reactions and behaviours used by relatives, we can find the total or partial concealment of the illness, denial and abandonment behaviour, or, on the contrary, paternalist behaviours since they consider people with SMI to be unable sick people (Young, 2018). All of this would prevent the independence and autonomy of the patient, and it would delay the search for treatment and social support at the same time (Muñoz et al., 2009). Thus, relatives would have difficulties or would avoid interpersonal relations, since they would anticipate social withdrawal and discrimination, negatively affecting their self-esteem and general state of mind.
Regarding the instruments of evaluation of self-stigma, there are different questionnaires that assess its impact on those personally affected by mental illnesses. These tools assess different emotional, cognitive and behavioural aspects related to the assimilation of stigma, the discrimination experienced and the ability to resist to stigma. Some examples are the Internalized Stigma of Mental Illness (ISMI; Risther, Otilingama & Grajalesa, 2003) which has been adapted to the Spanish language (Escala de Estigma Internalizado de Enfermedad Mental;Brohan, Elgie, Sartorius & Thornicroft, 2010). This scale comprises 29 items across five subscales (alienation, stereotype endorsement, discrimination experience, social withdrawal, and stigma resistance). In addition, the Internalized Stigma Scale (ISS) by King et al., (2007) (adapted to Spanish as Escala de estigma internalizado by Flores-Reynoso, Medina-Dávalos & Robles-García, 2011) comprises 28 items, including the discrimination and negative reactions perceived, shame and dissemination of information about the illness and the strategies to positively face that illness and the associated stigma. Finally, we must mention the Self-stigma in Mental Illness Scale (SSMIS); Corrigan, Watson & Barr, 2006) and its short form (Self-stigma of Mental Illness Scale-Short Form, SSMISSF; Corrigan et al., 2012) that include subscales such as alienation, stereotype endorsement, discrimination experience, social withdrawal and stigma resistance.
Nevertheless, there is an important lack regarding the development and validation of instruments that allow the assessment of stigma in relatives, and the scientific literature on this matter is scarce despite its great impact and terrible consequences. For this reason, Morris et al. (2018) developed the only available scale to evaluate self-stigma in relatives of people with SMI. For the development of the Self-Stigma in Relatives of People with Mental Illness (SSRMI; Morris et al. (2018) they followed both a deductive and inductive method through a process with several phases. During the first phase, of inductive nature, they worked with first-degree relatives of people with mental disorder. By means of a group interview, they created a database of possible items. In the second phase, of deductive nature, they assessed the potential of these items and chose those which adjusted better to the theorical constructs which are available in the literature about stigma. In the third phase, they took into considerations the comments made by the relatives during the interviews in order to reduce the number of items, obtaining a scale which comprises 30 items. In the final phase, they validated the questionnaire by using it with 195 first-degree relatives of people with mental disorder (schizophrenia, schizoaffective disorder and bipolar disorder). Statistical analyses confirmed its accurate psychometric properties regarding the internal consistency and test-retest reliability. However, unlike the hypothesis of the researchers, the statistical tests did not support the existence of the five subscales that the authors had considered at first (stereotypes, separation, devaluation, culpability and loss of status), proving that it was more accurate to use an unifactorial structure.
For all these reasons, the goal of this study consisted on adapting and validating to the Spanish context this innovative scale, the Self-stigma in Relatives of People with Mental Illness Scale, which will provide a valid and reliable instrument to assess the degree of self-stigma in relatives of people with SMI in Spain. It is expected that this scale will show good signs of adjustment, as the original version, in addition to gender invariance.
Method
Participants
304 adults (155 men and 149 women) aged between 35 and 57 (M = 44.57; SD = 15.29) from the autonomous region of Madrid participated in the study. An accidental, non-probability sample was carried out, since all participants were first-degree relatives of people diagnosed with schizophrenia or schizoaffective disorder.
Measures
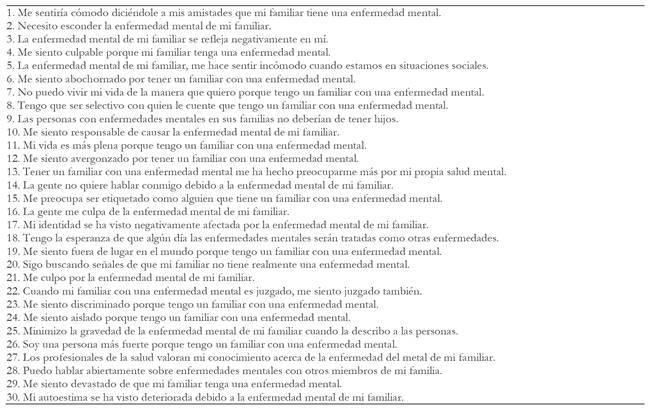
Self-stigma in Relatives of People with Mental Illness Scale. In order to assess the self-stigma perceived by the relatives of a child with mental illness, the Self-stigma in Relatives of People with Mental Illness (SSRMI) by Morris, et al., (2018) was adapted. The questionnaire is preceded by the following introduction: “The following questions ask how you currently feel about your family member's mental illness. Although we use the term 'mental illness', please think of this in whichever way you feel most comfortable. If you have had a diagnosis of mental illness yourself, as you answer the questions, please focus on how you feel related to your family member with a mental illness, rather than your own diagnosis. Please mark whether you strongly disagree, disagree, feel neutral, agree, or strongly agree.”
The scale includes 30 items, distributed in five factors: stereotyping, discrimination, separation, culpability and devaluation. Items1, 11, 18, 26, 27, 28 are reverse coded. Participants had to answer by means of a Likert scale from 1 (strongly disagree) to 5 (strongly agree). Additionally, Morris et al., (2018) pose a short version of the SSRMI, which comprises ten items: 6, 13, 14, 15, 16, 21, 23, 24, 25 and 30.
Procedure
In order to validate the scale, direct and reverse translations were used (Hambleton, 1996). This method consists on translating the original questionnaire directly into Spanish by a group of expert translators, and then back-translating it into its original language by another group of translators. Both groups are formed by two sworn translators graduated in Psychology. The members of the first group are Spanish speakers, and those of the second group are English speakers. The final version was analysed by three experts in clinical psychology with great knowledge of hospital centres and research experience, ensuring that the items were correctly designed to assess the intended construct without losing the original meaning (Lynn, 1986).
Once the questionnaire was ready, the Bioethics Committee on Human Research of the University of Almeria (ref. UALBIO 2019/014) was asked to approve the research, in order to contact several medical centres and associations of the region of Madrid to request their collaboration, after informing them of the aim of the investigation. Relatives were required to sign an informed consent before they could participate in the study. Before giving the scale to all the participants, it was completed by a small group of eight people (three men and five women) to ensure the correct understanding of all items. The questionnaire was given under the supervision of the main researcher of this study, who explained and solved the questions that appeared in the process. The questionnaire was completed inside the clinical services. The estimated time to complete the questionnaire was about 15 minutes.
Data analysis
In order to determine the validity and reliability of the SSRMI in the Spanish context, the psychometric characteristics of the questionnaire were analysed. First, a confirmatory factor analysis (CFA) to test the factor structure of the 30-item questionnaire, a second higher-order confirmatory factor analysis and a third confirmatory factor analysis of the short version, a 10-item scale, were performed. Secondly, a multi-group analysis was carried out to analyse the gender invariance, both for the 10-item scale and the 30-item scale. Then, statistical analyses were performed and the reliability of the instrument was tested by using internal consistency analyses (Cronbach’s alpha). For the data analyses, the statistical packages SPSS 19.0 and AMOS 19.0 were used.
Since the Mardia’s coefficient turned out high (359.51), the maximum likelihood estimation method along the bootstrapping method was used for the CFA. Estimators were not affected by the lack of normality, so they were considered robust estimators (Byrne, 2001). For the purpose of accepting or rejecting the proposed models, a group of adjustment indexes was considered: χ2/gl, CFI (Comparative Fit Index), IFI (Incremental Fit Index), RMSEA (Root Mean Square Error of Approximation) and its confidence interval (CI) at 90%, and SRMR (Standardized Root Mean Square Residual). Since χ2 is very sensitive to the sample size (Jöreskog & Sörbom, 1993), χ2/gl was used, considering values lower than 5 acceptable (Bentler, 1989). Incremental indexes (CFI and IFI) show a good adjustment, with values higher than .90 (Shcumacker & Lomax, 2012), while the error indexes (RMSEA and SRMR) are considered acceptable when values are equal or less than .08 (Hu & Bentler, 1999).
Results
Confirmatory Factor Analysis
The adjustment indexes of the tested model (Figure 1) showed appropriate adjustment indexes for the 30-item scale χ2 (395, N = 304) = 888.86, p < .001; χ2/gl= 2.25; CFI = .93; IFI = .93; RMSEA = .064 (IC 90% = .059 - .070); SRMR = .049. The standardized regression coefficients fluctuated from .70 to .91 and they were statistically significant (p < .001).
Regarding the higher-order model, the adjustment indexes were appropriate: χ 2 (400. N = 304) = 917.91, p < .001; χ 2 /gl= 2.30; CFI = .93; IFI = .93; RMSEA = .065 (IC 90% = .060 -.071); SRMR = .062, with a correlation between the higher-order factor, called Self-stigma, with respect to separation .76, discrimination .65, stereotyping .68, culpability .79 and devaluation .47.
Regarding the 10-item scale: χ2 (35. N = 304) = 143.87, p < .001; χ2/gl= 4.11; CFI = .93; IFI = .93; RMSEA = .078 (IC 90% = .072 - .086); SRMR = .054. The standardized regression coefficient fluctuated from .54 to .90.
Analysis of Gender Invariance
In order to check if the factor structure of the 30-item scale is invariant to gender, a multi-group analysis was performed. No significant differences were found, as shown in chart 1, between model 1 (unrestricted model) and model 2 (weighted invariance model). However, there were significant differences between model 3 (structurally invariant covariance model) and model 4 (invariant model of mean residuals). The absence of significant differences between model 1 and model 2 is a minimum standard to accept that the structure of the model is invariant to gender (Byrne, Shavelson & Muthén, 1989).
Regarding the 10-item scale, no significant differences were found between model 1 (unrestricted model), model 2 (weighted invariance model) and model 3 (structurally invariant covariance model). However, there were significant differences between model 1and model 4 (invariant model of mean residuals). These results also confirm the gender invariance of the 10-item model.
Statistical descriptions, correlation and reliability analyses
The correlation between the five factors can be seen in chart 2, which shows that this correlation is significant, proving a clear reciprocity between the factors. Likewise, in order to obtain evidence of the reliability of the scale, an internal consistency analysis was performed, with satisfactory results, over .80.
Discussion
The main aim of this study was the analysis of the psychometric properties of SSRMI (see appendix). To do so, three CFA were carried out: one for the long version of the questionnaire, another for the short version with 10 items, and a last one for the higher-order model, as well as an analysis of internal consistency and an analysis of gender invariance. The results of the study confirmed the SSRMI as a valid and reliable scale to assess family self-stigma.
The CFA of the factor structure of SSRMI showed proper adjustment indexes both for the long version of the questionnaire and for the 10-item short version. Accordingly, the CFA supported the existence of five independent factors, stereotyping, culpability, devaluation, discrimination and separation. These results partially concur with the results of the original study, in which the factor structure of the scale by Morris et al., (2018) showed adequate psychometric properties. Nevertheless, the results did not support the existence of five subscales, since the exploratory factor analysis that they performed showed that the four-factor model was the one which adjusted better.
The reliability analyses carried out by means of an internal consistency analysis showed acceptable adjustment indexes for each of the five factors that form the scale and for the single factor of the short version of the questionnaire.
Regarding the higher-order model, called Self-stigma, the factor structure was confirmed with an FCA. This model is interesting since it supports the use of a global value formed by the average of the five factors, that can be used by researchers in order to simplify models with several constructs. Moreover, its use is justified since the study carried out by Ritsher et al., (2003) and Ritsher & Phelan (2004) suggested that self-stigma factors tend to work like a single “body” in different situations.
Regarding the multi-group analysis, the results proved that the structure of the full questionnaire and that of the short version where invariant to gender. These results agree with the use of the questionnaire in future researches in order to compare the averages between men and women. Nevertheless, future studies must analyse the invariance structure regarding other variables, such as age, socioeconomic status or education.
Conclusions
The results support the suitability of the psychometric instrument to assess self-stigma in relatives of people with schizophrenia, a relevant matter given, for instance, the direct consequences that self-stigma causes in relatives when they assimilate the negative messages coming from the general society, other relatives or even healthcare professionals (Shibre et al., 2001). We must consider as well the cost of the indirect consequences, such as postponing the search for treatment for the person with mental illness and social support for themselves (Ritsher & Phelan, 2004; Navarro-Bayón, García-Heras, Carrasco-Ramírez & Casas-Toral, 2008).
The validated instrument can thus be useful, not only for the scientific community, in order to continue researching in a field of study which is relatively new and little analysed in current literature, but also for its use in clinical practice to find possible difficulties and obstacles within the family environment, providing the design of treatments that could minimize or eliminate the impact of self-stigma in these situations. Likewise, the possibility of using different factors might help to guide the treatment and to give a special importance to those aspects that seem more compromised.