Introduction
Addiction is a multifaceted problem and affects every aspect of the lives of those who develop it (López Durán et al., 2008; Carrol and Rounsaville, 2002), the population with substance use disorder is one of the most difficult in terms of clinical management (Pedrero, 2003). One factor explaining part of this difficulty is high psychopathological comorbidity. Attending to the individual characteristics of users is vital for an effective treatment approach to addictive conditions, or, as the National Institute on Drug Abuse (2010) states, “no single treatment is appropriate for everyone…effective treatment attends to multiple needs of the individual, not just his or her drug use”.
Improving the success rates of intervention programs has brought interest in the study of variables that limit or mediate the scope and effectiveness of these programs, with Personality Disorder (PD) the most common comorbid diagnosis in people with addiction. (Becoña and Cortés, 2008). Part of the problem of substance use is due to dysfunctional behavior patterns maintained over time with high stability which determine the persistence of addictive behavior and the failure of strategies aimed at their control (Larson, Desai, y Kates, 2018; Pedrero, Puerta, Lagares and Sáez, 2003).
We wish to stress the importance of studies relating to personality patterns with addictive behavior and other psychopathological conditions (Coriale et al, 2019; Karpyak et al, 2019). Some studies affirm that these patterns greatly influence diagnosis, therapeutic intervention and prognosis. Martínez & Trujillo (2003) highlight some consequences of personality disorders on a dual diagnosis drug dependent population if there is no proper approach to the comorbid disorder: difficulty in achieving abstinence with frequent relapse, less adherence and retention to treatment, misuse and abuse of psychopharmaceuticals, and deterioration of the patient-therapist relationship among others.
The relationship between personality disorders and substance use is complex, given there is great variability for prevalence rates, which depend both on substance and methodology used (criteria, questionnaires, cut-off points ...). Difficulties in establishing prevalence rates are based on both conceptual and methodological aspects, therefore, prevalence of personality disorders in cocaine-dependent subjects ranges from 36.7% (Lorea, Fernández-Montalvo, López-Goñi and Landa, 2008) and 97% (Calsyn and Saxon, 1990). The prevalence of PD ranges in the normal population is between 10% and 15% (Verheul, 2001).
It should also be noted that the prevalence of personality disorders found in drug dependent populations in treatment is questionable, since evaluation of these disorders is often carried out at the onset of treatment. Behaviors derived from the addiction itself often overlap with the descriptions of particular personality disorders (Rodriguez and Salgado, 2018).
Skinstad & Swain (2001), and San-Molina (2004) concluded that the most frequent personality disorders in the substance use population are firstly those belonging to cluster B, specifically borderline personality disorder (BPD) and antisocial personality disorder (ASPD). Followed by cluster C disorders such as avoidant personality disorder (APD), passive-aggressive personality disorder (PAPD), obsessive-compulsive personality disorder (OCPD); and lastly cluster A disorders, highlighting Schizoid personality disorder (SPD). Bravo De Medina, Echeburúa, & Aizpiri (2007), found the most prevalent personality disorders in an alcoholic population, those matching histrionic (63.6%), narcissistic (67.4%), and antisocial (67.5%) personality patterns, all from Cluster B. Similar results were found by López & Becoña (2006) in a cocaine dependent population, passive-aggressive (33.3%), antisocial (22.5%), and narcissistic (18.6%) personality patterns were most prevalent. Similarly, results from Fernández-Montalvo, López-Goñi, & Landa (2004), in a therapeutic community population showed greater prevalence of ASPD (42.9, followed by PAPD and narcissistic personality disorder (21.4%).
Although in recent years several studies have explored gender differences in substance dependence treatment, results are far from conclusive (Fernandez-Montalvo, López-Goñi, Azanza, and Cacho, 2014). The paucity of research addressing gender differences may be mediated by the difficulty of obtaining sufficiently large samples of women with drug use problems which allows incidence and features of drug dependence in women to be studied with a minimum of representativeness (Castillo, Llopis, Rebollida, Fernández yOrengo, 2003). In the scientific literature, it is found that most studies analyze the mixed population which proportionally is not generally above 20% of female users. López-Goñi, Fernández-Montalvo, and Arteaga, (2012) for instance, obtained a profile of 80.5% men, Roncero et al., (2016) a profile with 84% men, and data from users attended by UNAD (2018) estimate only 25% of care for women (including advisory services to families, employment, specific to women ...), while Proyecto Hombre nationwide has attended to a proportion of women at 16.6% (Proyecto Hombre Association 2018). This low number of female users attending treatment centers may be explained by the lower proportion of addicted women, or because women suffer greater social stigma, hindering their search for therapeutic assistance, neither possibility being exclusive (Fernández-Montalvo et al., 2014).
The Spanish National Strategy on Addictions focuses on the fact that women can suffer twice over: firstly, as victims of gender violence by a partner also a drug user and women themselves may also have a substance related disorder due to this violence (National Strategy on Addictions 2017-2024).
Studies indicate female drug users generally present more anxiety and depressive symptoms and more problems adapting to daily life than men, using alcohol later in life than men, being significantly older when this pattern becomes problematic. They also report more problems related to family, social life, and mental and physical health, while men report higher criminality rates and thus legal and financial problems (Ávila and González, 2007; Fernandez-Montalvo et al., 2014; Storbjörk, 2011)
As regards personality disorders, Miquel, Roncero, López-Ortíz and Casas (2011) following a systematic review of 40 published studies with information on gender differences in prevalence and clinical characteristics in dual diagnosed patients, reported a greater prevalence of psychotic and bipolar disorders in men, while in women a higher prevalence of anxiety and affective disorders, more daily life impairment, related to a higher prevalence of OCPD, dependent, and histrionic personality patterns.
Therefore, there appears to be a clearly defined gender profile. The higher presence of anxious depressive symptomatology and cluster C personality disorders lies in female drug users.
The aim of this work is to identify the socio-demographic and psychopathological features of users with an addiction problem, and differences amongst men and women with addiction problems.
Method
Design
We performed a non-experimental cross-sectional descriptive study with two independent groups paired by gender (male, female).
This protocol has been designed following the principles in the Helsinki Declaration, and with the approval of Solidaridad y Reinserción Foundation (Proyecto Hombre Murcia). All participants provided written informed consent for inclusion of their data in the study.
Participants
The sample consisted of people, who voluntarily requested treatment for addiction from the Solidarity and Reinsertion Foundation in the residential treatment program from January 2013 to December 2016. This program caters for patients throughout the region with addiction problems.
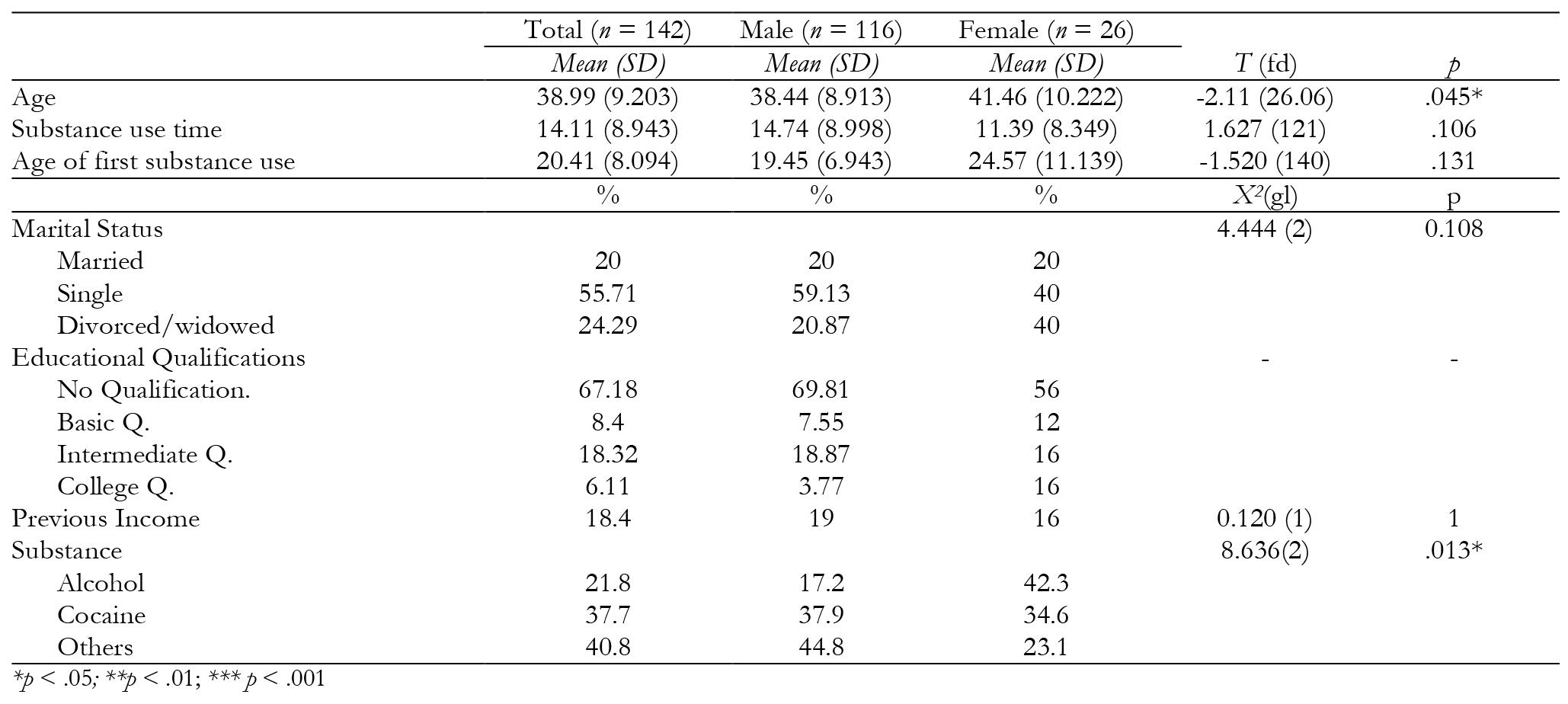
Participants were 142 drug users 81.69% (n = 116) male and 18.31% (n = 26) female, aged between 18 and 62 (M = 38.99 years; SD = 9.203), mostly single (55.71%), followed by 24.29% divorced and 20% married. 67.18% of the sample had no formal education, while 8.4% had completed basic education, 18.325 intermediate, and 6.11% university.
Cocaine motivated most treatment requests (37.7%). The mean age of first substance use was 20.41 years old (SD = 8.094). Patients had been consuming on average 14.11 years (SD = 8.943) before entering treatment.
Instruments
The evaluation instruments used are part of the center´s clinical evaluation protocol; and not specifically selected for this study.
The EuropASI (Kokkevi and Hartgers, 1995) is the European version of the Addiction Severity Index (ASI), (McLellan, Luborsky, Woody, and O'Brien, 1980), we used the Spanish version by Bobes, González, Saiz, and Bousoño for this study (1996). This is a semi-structured, hetero-applied clinical interview with a total of 159 items, widely used for evaluation and diagnosis of patients on admission to treatment programs. It explores six areas of special relevance to addiction problems: physical health, employment and resources, alcohol and / or drug use, legal situation, family history, family and social relationships, and mental health. Besides different items for each area, the instrument also returns a severity index for each. Scores range from 0 (no problem) to 9 (extreme problem). Taking into account that from 4 it is already considered that treatment may be indicated.
The Millon Multiaxial Clinical Inventory (MCMI III), (Millon, Davis and Millon, 2007), is a self-applied clinical questionnaire of 175 dichotomous response items (true / false). It is used both in clinical practice and research in the field of addiction (Perea-Baena, Compán and Ortíz-Tallo, 2009; Pérez, Durán and del Río, 2012; Pedrero, 2003; López-Goñi, Fernández-Montalvo and Arteaga, 2015; Arteaga, Fernández‐Montalvo and López‐Goñi, 2015; etc.). As well as four modifying indices (sincerity, social desirability, devaluation and validity), it presents 24 scales divided into four blocks according to severity level : eleven clinical personality patterns defined in Axis II of the DSMIV-TR (American Psychiatric Association, 2000), three serious pathological personality patterns of seven clinical syndromes of moderate severity and three other syndromes of severity.
Procedure
All participants were interviewed by psychology professionals with experience in the area of addiction; this evaluation was performed in three sessions before starting treatment. In the first session, data related to sociodemographic conditions and drug use was collected throug h EuropASI, and the remaining protocol questionnaires were applied in the following sessions.
Inclusion criteria: a) meet criteria for diagnosis of substance dependence disorder according to DSM-IV-TR (American Psychiatric Association, 2000), b) be aged between 18 and 65 c) consume any addictive substance, with or without other associated addictive behaviors, with serious impairment in personal, social, family and work functioning, d) carry out three initial interview sessions and e) have completed questionnaires.
Statistical Analysis
Descriptive analyzes were performed for all variables calculating frequency and percentage distribution, as well as calculations of mean and standard deviations. We used Pearson’s Chi-Square and Fisher’s exact test to measure and compare significant differences between male and female participants based on distribution of prevalence of variables. For continuous variables, both parametric (Student T) and non-parametric tests (U Mann of Whithney) were used, depending on whether these variables fit the normal distribution (K-S Kolmogórov-Smirnov). Differences were considered statistically significant when p < .05. To calculate the effect size of nonparametric tests, we calculated r (r = Z / √N) in accordance with the procedure described by Rosenthal (1991) for nonparametric tests, and G Heghes for t tests with non-equivalent groups. All statistical data was performed using SPSS v.18.0.
Results
The mean age of men (Table 1) accessing treatment (38.44 years / SD = 8.913) is lower than women (41.46 years / SD = 10.222) (t (26.06) = -2.11, p < .05). Although percentage of married people is the same for both sexes, the percentage of divorced or widowed is significantly higher (40% women to 20.87% men). There are no statistically significant differences between gender and level of studies, as most users had no educational qualification (67.18%).
For male participants cocaine is the primary used substance motivating treatment (37.9%), and alcohol for female participants (42.3%). However, the mean age of first substance use in men is 19.45 years old (SD = 6.943), an average of 14.11 years (SD = 8.943) of substance use before entering treatment. As for women, mean age of first drug substance use is noticeably higher (M = 24.57 years; SD = 11.139), entering treatment after a mean of 11.39 years (SD = 8.349), with no significant differences found.
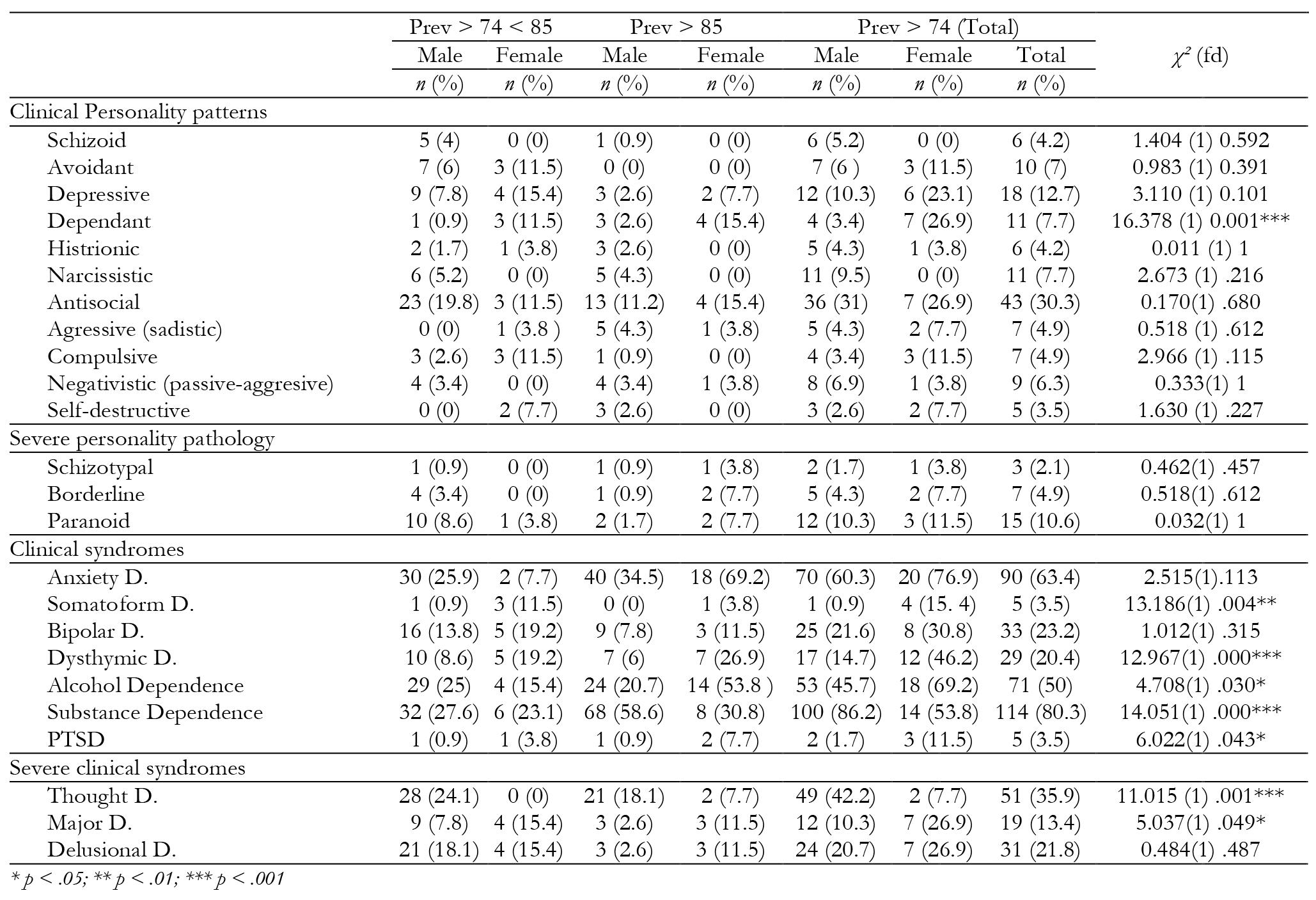
Regarding symptomatology prevalence (Table 2), according to results obtained through the MCMI-III questionnaire, we found 79% of prevalence of mild symptomatology (PREV > 74), suggesting the presence of personality disorders (80.8% women and 66.4% men). By applying stricter criteria (PREV > 84) the rate of personality disorders would be 31.7% (34.6% for women and 31% for men) (see Table 2).
As for prevalence of personality disorders, when we crossed the variable with gender, significant differences were only found for the dependent pattern (χ² = 16.378 (1) p < .001), much higher in women (26.9%) than men (3.4%). Similar to the depressive pattern (23.1% women, 10.3% men), compulsive (11.5% women, 3.4% men), avoidant (11.5% women, 6% men) and self-destructive (7.7% women, 2.6% men), these differences not being statistically significant. Nevertheless, although also without significant differences, a higher prevalence was found for schizoid personality disorders in men (5.2% men, 0% women), narcissistic (9.5% men, 0% women) and antisocial (31% men, 26.9% women).
Women show higher prevalence for clinical syndromes and differences are statistically significant in somatoform (15.4% women, 0.9% men), bipolar (30.8% men, 21.6% women), dysthymic (46.2% women, 14.7% men), post-traumatic stress (11.5% women, 1.7% men) and major depression (26.9% women, 10.9% men). Men present more prevalence in thought disorder (42.2% men, 7.7% women) and substance dependence (86.2% men, 53.8% women).
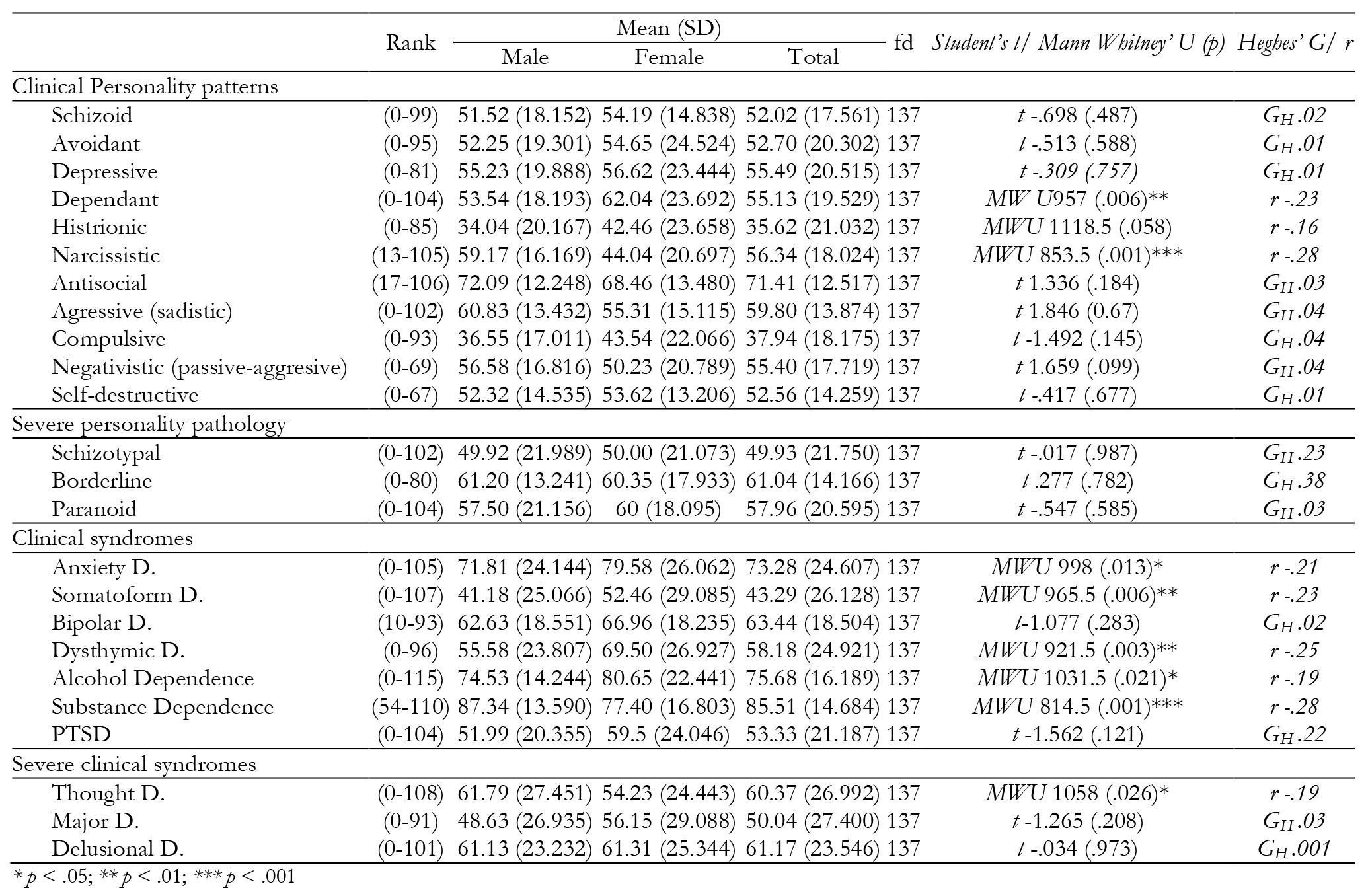
When focusing on descriptive data (Table 3), highest scores are found in substance and alcohol dependency scales. In both cases, cut-off points established as criteria in the MCMI-III are exceeded, with women most serious in alcohol dependence (80.65 women, 74.53 men). Men present higher scores in substance dependence (87.34 men, 77.40 women).
Among clinical syndromes, apart from substance dependence (UMW 814.5, p < .001) and thought disorder (UMW 1058, p < .05) where men obtained higher scores, women presented greater symptomatology severity for remaining scales. Statistically significant differences were found for anxiety disorder (UMW 998 p < .05), somatoform disorder (UMW 965.5, p < .01) and dysthymic disorder (UMW 921.5, p < .01).
As for personality disorders, the antisocial pattern achieves higher scores for both sexes though higher in men (72.09 men, 68.46 women). There exist differences between sexes for two traits, women present higher scores for the dependent pattern (UMW 957, p < .01), while men for the narcissistic pattern (UMW 853.5, p < .001).
Discussion
The aim of this paper is to learn the socio-demographic and psychopathological characteristics of addiction treatment patients in Murcia, and specific characteristics defined by gender.
As a result of this study, we found that the profile of a person entering treatment in PH Murcia is a man (81.89%), mean age 39 years, single (55.71%), and with no formal education (86.18%), a cocaine user (37.7%) alcohol user (21.8%), began consuming at 20 years old, and is seeking treatment after 14 years of active substance use.
This profile is similar to those provided by other associations working in the area in Spain in 2017 such as the Proyecto Hombre Association (2018) with 2960 cases and UNAD (2018) with 44787 cases evaluated across the country. In the Spanish scientific literature these results have been stable in the last decade. López-Goñi, Fernández-Montalvo, & Arteaga, (2012), obtained a profile of 80.5% men, aged 37.6 years and 49.9% cocaine users. However, data obtained by López-Goñi, Fernández-Montalvo, Arteaga, & Esarte (2017) showed 73.5% of male participants with a mean age of 36.4, mainly cocaine user (39.3%), and Roncero et al. (2016) a profile of 84% males, with a mean age of 38.9, cocaine users (36.9%). This profile already provided by the Spanish National Plan on Addiction (2009-2016) reported higher cocaine use than heroin.
Other relevant data is the scarce percentage of women seeking addiction treatment (18.31%), in line with data from other studies in the Spanish population usually 11% to 25% of female participants (Fernández Del Río, López, & Becoña, 2011; García Rodríguez et al., 2005; Iraurgi Castillo, Sanz Vázquez, & Martínez, 2004; Pérez del Río, 2012; Rodriguez & Salgado, 2018; Roncero et al. 2016; UNAD 2018; Proyecto Hombre Association, 2018).
Another variable where we found statistically significant differences is the mean age when treatment begins (38.44 years for men and 41.26 for women). There are notable differences in years of drug use before starting treatment (14.74 men / 11.39 women) and mean age of starting substance use (19.45 men / 24.57 women), although there is no statistical significance. These differences coincide with data provided by other studies; Ávila and González (2007), in a sample of 370 patients with alcohol addiction, 325 men (87.8%) and 45 women (12.2%), with a mean age of 42.83 and 44.60. respectively, indicated that women begin drinking significantly later than men (19.61 and 16.90), were quite older when the drinking pattern became problematic (30.93 and 24.68 years), had fewer years of substance use (13.26 versus 17.85 years). This pattern is repeated in data provided by the UNAD addiction report (2018), where percentage of users over 45 years of age is higher in women (24% women, 22% men), a trend reversed in years of substance use before start of treatment, where percentage of men with over 11 years history of substance use is 40% while 32% for women.
The main substance motivating treatment for each gender group is different, for men cocaine 37.9% and women alcohol consumption 42.3%. These data coincide with scores obtained in MCMI-III where women had higher mean scores for alcohol dependence (80.65 women, 74.53 men) while men higher mean scores in severity scale in substance dependence (87.34 men, 77.40 women). Blanco, Sirvent and Palacios (2005), affirm alcohol and tobacco use is substantially higher in women. Men consume cocaine or cannabis to a greater degree, data contributed by the EDADES report (2017), UNAD (2018) or the Proyecto Hombre Association (2018), show that most women seek treatment for their alcohol and tobacco dependence and men tend to seek treatment for their cannabis and cocaine dependence.
This study indicates that the presence of psychopathology in the analyzed sample is quite high, 79% of participants present scores with clinical indicators of personality disorders (80.8% women and 66.4% men). Although following the strictest criteria, 31.7% have at least one personality disorder (43.6% women and 31% men).
These results coincide with other studies such as Pedrero et al. (2003) and Fernández Montalvo et al. (2014) finding 83% and 76.2% of users with at least one personality disorder respectively. Craig (2000) obtained 91% prevalence of comorbid personality disorder in a sample of 160 opiate users and 283 cocaine users, using MCMI II.
This study finds a greater presence of psychopathology associated with substance use in women than men, however no clear evidence whether dual pathology is more common in either sex. Research in mental health settings found greater rates of male patients with dual pathology than women, whereas in drug dependency treatment units data showed the opposite (Miquel et al, 2011). In Spain, a study carried out with a population from several drug dependency treatment units found 47.5% of women meet criteria for dual pathology, while 30.3% of men met the same criteria (Gual, 2007). Rodríguez-Jiménez et al (2008) instead conducted a study in a sample of 257 patients from a psychiatric hospitalization unit (UHPHG) in Madrid finding 24.2% of patients met criteria for both substance dependence disorder and comorbid psychopathological disorder, 87.5% men and 12.5% women.
As for personality disorders more concomitant with substance use, in this study, using the least strict criterion (PREV > 74), we have antisocial personality disorder, presented by 30.3%, paranoid (10.6%), narcissistic (7.7%) and dependent (7.7%). These data coincide with other studies, thus, Rodriguez and Salgado, (2018) found 42.5% of patients (N: 106) with some personality disorder, antisocial disorder being most prevalent (25.5%), paranoid (13.2%) and narcissistic (11.3%). Fernández-Montalvo, López-Goñi and Landa (2004) found 42.86% of a sample of 42 patients who sought treatment diagnosed with antisocial personality disorder, followed by passive-aggressive personality disorder (40.5 %) and narcissistic personality disorder (21.4%). Data similar to that by Skinstad and Swain (2001) and San-Molina (2004) mentioned in the introduction. As for differences between men and women, the dependent pattern is highest in the former (26.9 % vs. 3.4% in men) coinciding with the findings of Pedrero et al. (2003) (47.2% vs. 31.4%).
In addition to substance and alcohol dependence, anxiety disorder is among the most frequent clinical syndromes, diagnosed in 62.7% of participants, higher in women (76.9%) than men (59.5%). This data coincides with a study by (Ortiz-Tallo, Cardenal, Ferragut and Cerezo, 2011) in the clinical population (N = 7011), finding anxiety the most diagnosed clinical syndrome, also more common in women (53.74% than men (46.26%). There are also significant differences in this study in somatoform disorder (15.4% women and 0.9% men), dysthymic disorder (46.2% vs.13.8%), post-traumatic stress disorder (11.5% vs. 1.6%) and finally major depression (26.9% vs. 10.3%) in favor of women, while only in thought disorder did men (41.4%) present higher rates than women (7.7%). It should be noted that despite finding no statistically significant differences, narcissistic disorder (11.2% and 0% respectively) is higher in men than in women.
Conclusions
The studies analyzed and the data provided in this research indicate high prevalence of psychopathological disorders and high comorbidity (dual pathology) in those who have substance and alcohol abuse. It is also observed that men seek most care and treatment, generally exceeding 80% of samples analyzed, therefore it is essential to analyze the social and clinical conditions of women who seek treatment for addictive problems.
Data provided indicate two different impairment paths: clinical disorders and personality disorders. The MCMI questionnaire brings diverse psychopathological and functional impairment aspects, and together with the EuropASI, may bring a good pre and post evaluation protocol.
There are several methodological difficulties and limitations that should be taken into account in this study. Firstly, the sample comprises people actively seeking treatment for addiction, posing a serious difficulty in generalizing this data to those who are active substance abusers not seeking treatment. Another limitation is the non-control of variables such as relationship of substance of consumption with psychopathological variables, severity of addiction, time of abstinence and age, all variables that can mediate results. Our lack of control of the history of onset was also important and limited our explanations of gathered data. This work has taken gender differences into account; however women only comprise 18.31% of the sample. Data obtained from this subgroup can provide relevant information toward improving treatment efficacy.











 texto em
texto em