Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.22 no.4 Zaragoza oct./dic. 2008
Changes in utilization of community mental health services in three boroughs of Athens (1979/1983-2000/2004)
Michael G. Madianos MD, MPH, Dr Med*, George Alevisopoulos MD*, George Kallergis MD*, Evi Koukia R.N., DrN*,**, Olga Rouvali MD**, Vlassios Tomaras MD***
* Department of Mental Health and Behavioral Sciences, Zografou Community Mental Health Center (CMHC) School of Health Sciences, Faculty of Nursing, University of Athens
** Attending Psychiatrist, Zografou CMHC
*** Department of Psychiatry, Medical School, University of Athens. GREECE
ABSTRACT
Background and Objectives: Several investigators reported that there is a gap between prevalence of mental disorders and utilization of mental health services. The trends in help -seeking from two Community Mental Health Centers (CMHC) serving three boroughs in Athens and having identical organizational profile were examined.
Method: Utilization rates were compared for the first four years of operation (1979-1983) of the first CMHC in Greece and the corresponding first years 2000-2004 of the most recent CMHC in the country. The sociodemographic characteristics of both catchment areas were almost identical.
Results: In the years 2000-2003 the time of untreated mental disorders was found to be lower than that of 1979-1983. Moreover only 4.6% of clients of the first CMHC were self referred contrasting the 51.7% of their counterparts of the second Center. More than 50% of persons, who have visited the second Center reported that this Center was the first psychiatric service in their life. Additionally between the years 2000-2004, the treated prevalence of depression was found to be much higher than that in the years 1979-1983.
Conclusions: Apparently these findings are probably linked with opinion changes towards psychiatry and mental illness, ability of early recognition of psychopathological symptoms, as well as, the attitudinal change in the need for help-seeking.
Key words: Community psychiatric care, Early detection, Public attitudes, Untreated mental disorders, Help-seeking.
Introduction
Over the past decades several studies have provided information on rates of help-seeking and mental health services utilization and the underlying factors1-10.
The main findings of the majority of these studies were the following: the history of prior contacts with psychiatric services predicts a higher current utilization. In some areas under investigation, the rates of treated schizophrenia decreased while the rates of other mental disorders increased yearly, especially the treated rates of mood disorders.
All these changes suggest the importance of accessibility to mental health services11. In the United States, the ECA Survey revealed utilization rates varying from 12.0% to 14.7%10. Next to the presence of a disorder, the ECA survey reported that self-perception of mental health was the strongest predictor of help-seeking behavior6.
Other studies on mental health services research compared the utilization patterns between services of similar organizational background5,12-17. Almost all these studies reported that the use of CMHC's doubled in recent decades and these trends in service use are explained by broad changes in help-seeking behaviour.
Finally another bulk of studies focused on the exploration of factors affecting the treatment of severe mental illness and the possible delays in help-seeking7,18-23.
From the Commorbidity Survey in United States the median delay time in help-seeking was found to be between 6-14 years across the mental disorders23.
Greece, a country rapidly changing through urbanization, industrialization and migration, had until the late seventies, a rather traditional mental health care delivery system, based on the existing at that time nine mental hospitals, with a lack of community based alternatives of care24.
In view of this situation, in 1978 the Department of Psychiatry of Athens University Medical School and the first of the authors, took the initiative to develop the first Community Mental Health Center (CMHC) in the country, as part of a network of University Mental Hospital services25.
The Center serves a catchment area of two neighboring boroughs, Byron and Kessariani, with approximately 200,000 mostly middle and lower class inhabitants. The area's sociodemographic characteristics are similar to those of the other boroughs of greater Athens. This area was lacking any private or public psychiatric facilities until the establishment of the Center. The Center's organizational stucture was based on community psychiatry principles25.
The local psychiatric morbidity and people's attitudes towards mental illness have been explored by systematic socio-psychiatric surveys11,26-28. The main findings were that 14% of the population, were identified as "cases" and the ratio between treated and untreated "cases" in 1981 was found to be 1:10. Several other studies have focused on the effectiveness of the Center's interventions29,30. The Center has proven to act as filter in the admissions in psychiatric inpatient services30. Between 1979 and 2000 eight additional CMHCs were gradually established in greater Athens31.
In the year 2000 twenty one years after the opening of the first CMHC in Athens (and Greece) another Center was established, the last of its kind, to serve a neighboring borough of the previous ones, the Zografou borough of similar sociodemographic characteristics with 150,000 middle and middle lower class inhabitants. The Zografou Community Mental Health Center belongs also to the University of Athens. The initiative for its development was taken again by the first of the authors.
The ideology of staff and the organization structure of the new CMHC were identical with those of the Byron Kessariani CMHC.
This paper reports the findings of a comparative study focused on the first four years of the operation of both CMHCs in a time difference of more than twenty years.
The purpose of this study was to answer the following questions.
-Were there any differences in the frequency of attendances between 1979-1983 and 2000 and 2004?
-Was there any difference in the duration of untreated psychopathology between the two time periods?
-Were there any differences in the help-seeking patterns between the same two periods?
-Were there any differences in the diagnostic profiles of clients between 1979-1983 and 2000 and 2004?
Methods
The design of this study focused on the exploration of possible changes in the patterns of visits, in two different periods, of residents of the three boroughs of greater Athens area in the Kessariani Byron and Zografou Community Mental Health Centers respectively.
The period to be compared were the first four years of the operation of each CMHC, namely the years 1979-1983 for the first and 2000-2004 for the second Center. Information on the characteristics of attendances in each Center included their frequency (single and total visits) the sociodemographics of visiting individuals including age, gender and occupation, sources of referral and clinical information. The latter consisted of data on any previous help-seeking experiences, the time of onset of psychopathological symptoms, the time for the first help-seeking and diagnosis. Diagnoses were made using the International Classification of Diseases 10th revision (ICD-10). It should be noted that the diagnoses of clients, who visited in the years 1979-1983 the Byron Kessariani CMHC were transformed from the ICD-9 diagnostic system which was used at that time, into the recent ICD-10.
The sociodemographic and clinical data used in this study, were drawn from the Psychosocial Evaluation Schedule obtaining the relevant information from every individual, who had visited the Centers.
The structure of the schedule was identical in both Centers. Diagnoses were made by the psychiatrist in charge of each case.
Statistical Analysis
The Chi square with Yates correction was applied to test the possible association of previous help-seeking from mental health services between the clients of both centers, as well as their diagnostic nosological entities, during the years under investigation. Student t-tested the comparison of the average years of onset of psychopathology and the time of help-seeking of clients of both centers during the same period. No human subjects or lists of clients were used.
Moreover there are no known conflicts of interest in this study.
Results
The mean age of clients who visited the Kessariani-Byron CMHC (A) and the Zografou CMHC (B) were 37.5 (s.d. = 11.5) and 38.2 (s.d. = 12.5) for males and 39.3 (s.d. = 12.5) and 45.1 (s.d. = 14.8) for females respectively. The latter showed a statistically significant difference, the female clients of CMHC (B) were older.
The comparison of occupational status categories of clients provide an almost identical profile for both Centers. The majority of male clients were skilled workers and technicians, as well as public employees or housekeepers for females (data not shown).
The total of first visits in Center A were 283 for males and 523 for females for the years 1979 and 1983. In the Center B (years 2000-2004) the first visits were 299 for males and 476 for females (Table I).
The total number of visits during the first four years of operation were 5,628 and 6,975 for Center A and B respectively. It is of note that during the first year of operation of the Center B the single and total visits were more than three times than those of the Center A, 21 years previously. Additionally the percentage increase between the first and the fourth year in single and total visits was found to range between +25.6% and +90.5%.
The major resource of referral for both Centers were the local sociomedical services. Former clients referred 15% and 11% of the individuals who visited Center A and B respectively. Only 4.6% of clients of CMHC A were self referred contrasting the 51.7% of their counterparts of CMHC B. The primary complain was emotional problem for 43% and 64.2% of clients of Centers A and B respectively, while bizarre (psychotic) behaviour concerned 16.1% and 9.4% of persons who visited CMHC A and B respectively.
Lower average years of untreated of psychopathology were recorded among the clients who visited the Center B between 2000 and 2004 compared to the average years documented in 1979 - 1983 in Center A, a statistically significant difference (Table II).
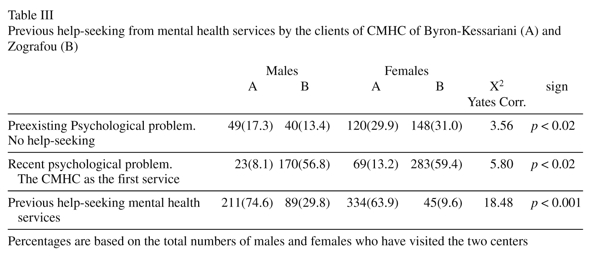
Table III presents the patterns of help-seeking of clients of both Centers.
More than 50% of persons of both sexes who have experienced a recent psychiatric episode and sought help by the Center B, reported that this Center was the first mental health service in their lifes to visit. This means that more than half of the clients of this Center were reached at an earlier stage, compared to their counterparts 21 years ago, of Center A, a difference at a statistical significant level of p < 0.002.
The vast majority of clients who visited the Center A (in 1979-1983) had previous experiences from other mental health services.
Finally in Table IV the diagnostic categories of clients who visited both Centers are shown.
Changes in three nosological entities of clients who visited the Center A and Center B (21 years later) were observed.
Particularly in 1979-1983 fewer individuals of both sexes were diagnosed as suffering by any type of mood disorders, compared to the ones in 2000-2004.
These changes were found to be statistically significant (p < 0.05). On the contrary fewer clients of Center B were found to suffer from any anxiety disorder compared to their counterparts of Center A twenty one years ago.
This difference was also statistically significant (p < 0.001).
Finally in the diagnostic category "other" there is a difference between the clients of the two periods, the clients of Center B being overdiagnosed as having "other diagnosis".
With respect to the delivery of care, almost identical distribution of the types of care was found in both Centers.
More than fifty percent of the clients of both Centers were given a combination of supportive psychotherapy and medication.
Counseling was offered to 20.3% and 18% of persons who visited CMHC A and B respectively. Very few individuals, in equal proportions, were referred to other services (7%) and fewer there admitted to inpatient psychiatric services (1.1%).
Completed suicides were not recorded during the periods under investigation. A 45.1% and 42% of clients of Centers A and B respectively continued their therapeutic contacts at the end or two evaluation periods.
Discussion
The results of this comparative study provide some evidence related to the following questions:
Are there any differences in the frequency of attendances between 1979-1983 and 2000-2004?
In the first year of operation of the CMHC B the single and total visits were more than three times than those of the Center A. However, there was almost equal number of first visits in both Centers in both periods, although the total visits in the Center B were found to be higher at 24.1%. In 1979 in Greece, there was an absolute lack of the concept that a serious psychiatric episode could be treated in the community.
The study of public attitudes in the catchment area of Center A (in 1979-1980) about mental illness detected discriminative views and increased social restriction32. These negative attitudes were reflected in the patterns of visits in the first years of operation (1979-1983) of Center A.
Is there any difference in the duration of untreated psychopathology between the two time periods?
In fact the difference between the average duration of untreated psychopathology (time between the onset of subjective symptoms and the first visit to a psychiatric service was found to be statistically significant with a lower average time of untreated mental disorders in the second time period. The possible explanation of the delayed treatment in the years 1979-1983 is the previously described negative atmosphere related to the existing views about psychiatric care and mental illness.
The phenomenon of delay in help-seeking has been described by several investigators3,7,10,12,13,17. In United States the median delay time was found to be between 6-14 years across the mental disorders7.
In 1994, the study of 1979-1983 on the opinions about mental illness, was replicated in the same area33. In this replication study the sample expressed more positive attitudes towards the social integration of the mentally ill, and did not favour the social discrimination and social restriction of mental patients. These results could be explained in the context of a more positive and tolerant social climate in the Athens area, strengthened by the implementation of systematic local community mental health intervention programmes undertaken by the staff of Byron Kessariani Community Mental Health Center29.
Are there any differences in the help-seeking patterns between the same time periods?
In the recent years 2000-2004 more than 50% of persons of both sexes, who have experienced a recent psychiatric episode and visited the Center B reported that this Center was the first service in their lives to visit, compared to 8.1% and 13.2% of males and females who sought help twenty one years ago. It is apparent that the clients of the Center B were reached at an earlier stage of psychopathology. Additionally, only 4.6% of clients of CMHC were self referred contrasting the 51.7% of their counterparts of CHMC B.
The organization of community intervention programs focusing on awareness and early identification of severe mental disorder, has been described as the method to abridge the gap between onset of mental disorder and help-seeking by several authors19,22,34,35.
This approach was also chosen by the staff of both CMHC's and proven to be effective29,30.
The widespread development of Community Mental Health Centers and psychiatric services in General Hospitals in Greece and especially in Athens, the last twenty years, added also to the lessening of the gap between untreated mental disorders and help-seeking31. The increased levels of recognition of a mental disorder as basic factor in early referral and treatment of psychiatric symptoms, suggest the importance of accessibility to effective community based mental health services, securing continuity of care12,19,20,36.
Are there any differences in the diagnostic categories of clients between 1979-1983 and 2000-2004?
In 1979-1983 fewer clients o both sexes were diagnosed as suffering from mood disorders compared to the ones in 2000-2004. On the contrary fewer clients of Center B were found to suffer from anxiety disorders contrasting their counterparts of Center A twenty one years ago. In the category "other diagnosis" the clients of Center B were over diagnosed.
In the same period 2000-2004, there was also a parallel increase in the proportion of persons treated for depression in the Byron Kessariani CMHC A. These findings are compatible with these reported by several others, inducing two nation-wide, cross sectional, surveys in Greece22,37-40. In England and Wales the prevalence of treated depression in general practice between 1994 and 1998 increased by 76.0% and 65.0% for males and females respectively (www.statistics.gov.uk, 1998).
In United States the rate of outpatient treatment for depression increased from 0.73 per 100 persons14 1987, to 2.3 in 199738. It seems that increased recognition of the depressive symptoms, the better tolerated new antidepressants and development of reliable and efficient procedures for diagnosing depression are the possible factors, for the higher use of individuals, suffering from mood disorders. On the other hand the increasing adversities in the lifes of million of people (economic recession, social disintegration, unemployment etc) are the possible underlying causes for the increasing prevalence of depression41,42.
To conclude the findings of this retrospective comparative study provide evidence that there are changes in the utilization of community based mental health care services in three boroughs of greater Athens (two catchment areas) especially in the untreated period of mental disorders. The level of recognition of psychopathology and the need for help-seeking is directly linked with the formation of positive attitudinal cognitions towards psychiatry, a finding already been reported by Madianos et al.31 in the first area under investigation.
On the other hand, the implementation of community mental health intervention programs on early recognition of psychiatric symptoms, could positively influence also the public concepts about psychiatric care, decreasing the untreated time period. These findings along with the prevention of admissions of local residents to inpatient psychiatric services, produce strong indications that community accessible mental health care could be proven to be effective to meet the needs of individuals suffering from a mental disorder.
Acknowledgements
This research outlined in this paper was part of a WHO collaborative study in the European region and was supported by grants from Research Projects Fund of the Ministry of Health and Welfare and the Special Fund for Research of the University of Athens.
References
1. D' Arcy C, Fritz W. A mental health system in transition: profiles of change. Can J Psychiatry 1979; 24: 121-131. [ Links ]
2. Lavik NJ. Utilization of mental health services over a given period. Acta Psychiatr Scand 1983; 67: 404-413. [ Links ]
3. Leaf PJ, Livingston J, Bruce M, Tichler GL, Holzer CE. The relationship between demographic factors and attitudes forward mental health services. J Community Psychol 1987; 15: 275-284. [ Links ]
4. Hansson L, Sandlund M. Utilization and patterns of care in comprehensive psychiatric care organizations: A review of studies and some methological considerations. Acta Psychiatr Scand 1992; 86: 225-261. [ Links ]
5. De Salvia D, Barbato A. Recent trends in mental health services in Italy: An analysis of national and local data. Can J Psychiatry 1993; 38: 195-201. [ Links ]
6. Regier DA, Goldberg ID, Taube CA. The de facto US mental health services system: A public health perspective. Arch Gen Psychiatry 1978; 35: 685-693. [ Links ]
7. Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after ontset of psychiatric disorders. Am J Psychiatry 1998; 155: 62-69. [ Links ]
8. Lefebre J, Legage A, Cyr A, Toupin J, Fournier L. Factors related to utilization of services for mental health reasons in Montreal, Canada. Soc Psychiatry Psychiatr Epidemiol 1998; 33: 291-298. [ Links ]
9. Adrews G, Henderson S, Hall W. Prevalence, comorbidity disability and service utilization: Overview of the Australian National Mental Health Survey. Br J Psychiatry 2001; 178: 145-153. [ Links ]
10. Regier NA, Narrow WE, Rae DS, Mandersheid RW, Lock BZ, Goodwin FK. The de facto US mental and addictive disorders services system. Arch Gen Psychiatry 1993; 50: 85-94. [ Links ]
11. Stefansson CG, Culberg J, Steiholtz-Ekecrantz L. From community mental health services to specialized psychiatry: The effects of a change in policy on patients accessibility and care utilization. Acta Psychiatr Scand 1990; 82: 157-164. [ Links ]
12. Ten Horn GHMM, Madianos M, Giel R, Madianou D, Stefanis C. A cross-cultural comparison of mental health care delivery in Athens and Groningen. Soc Psychiatry Psychiatr Epidemiol 1989; 24: 1-9. [ Links ]
13. Valbak K, Sorensen LV, Lindhardt A. Evaluation of community Psychiatry: A cross - sectional study. Acta Psychiatr Scand 1992; 85: 183-188. [ Links ]
14. Wells JE, Robins LN, Bushnell JA, Jarosz D, Oakley-Browne M.A. Perceived barriers to care in St Louis (USA) and Christchurch (NZ): Reasons for not seeking professional help for psychological distress. Soc Psychiatry Psychiatr Epidemiol 1994; 29: 155-164. [ Links ]
15. Saarento O, Oiesvold T, Göstas G, Lindhardt A, Sandlud M, Vinding HR, Zandven T, Hansson L. The Nordic comparative study on sectorized psychiatry. II Resources of psychiatric services and treated incidence. Acta Psychiatr Scand 1995; 92: 202-207. [ Links ]
16. Narrow WE, Regier DA, Rae DS, Kennedy C, Arons B. Mental health service use by Americans with severe mental illness. Soc Psychiatry Psychiatr Epidemiol 2000; 35: 147-155. [ Links ]
17. Ten Have M, Te Grotenhuis M, Meertens V, Scheeoers P, Beekman ATF, Vollebergh W. Upward trends in the use of community mental health and social work services in the Netherlands between 1979 and 1995: Are particular sociodemographic groups resposible? Acta Psychiatr Scand 2003; 108: 447-454. [ Links ]
18. Madianos M, Madianou D, Stefanis C. Help-seeking for psychiatric disorder from physicians of psychiatrists III Greece. Soc Psychiatry Psychiatr Epidemiol 1993; 28: 285-291. [ Links ]
19. Krstev H, Carbone S, Harrigan SM, Curry C, Elkins K, McGorry P. Early intervention in first-episode psychosis: The impact of a community development campaign. Soc Psychiatry Psychiatr Epidemiol 2004; 39: 711-719. [ Links ]
20. Malla A, Norman R, Scholten D, Manchanda R, McLean T. A community intervention for early identification of first episode psychosis: Impact on direction of untreated psychosis (DUP) and patient characteristics. Soc Psychiatry Psychiatr Epidemiol 2005; 40: 337-344. [ Links ]
21. Afifi TO, Cox BJ, Sareen J. Perceived need and help-seeking for mental health problems among Canadian provinces and territories. Can J Commun Ment Health 2005; 24: 51-61. [ Links ]
22. Broome MR, Wooley JB, Johns LC, Valmaggia LR, Tabraham P, Gafoor R, et al. Outreach and support in South London (OASIS): Implementation of a clinical service for prodromal psychosis and the at risk mental state. Eur Psychiatry 2005; 20: 372-378 [ Links ]
23. Kessler RC, Cliu WT, Demler O, Merikankas KR, Walters EE. Prevalence, severity and comorbidity of 12-month DSMIV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 617-627. [ Links ]
24. Madianos M. Mental illness and mental health care in Greece. Publ Health Rev 1983; 11: 73-93. [ Links ]
25. Madianos M, Stefanis C. Developmental issues and intervention strategies in a community mental health center in Greece. In: Hudolin V, editor. Social Psychiatry. New York: Plenum; 1984. p. 283-290. [ Links ]
26. Madianos M, Vlachonikolis I, Madianou D, Stefanis C. Prevalence psychological disorders in Athens area: Prediction of causal factors. Acta Psychiatr Scand 1985; 71: 479-487. [ Links ]
27. Madianos M, Stefanis C, Madianou D. Prevalence of mental disorders and utilization of mental health services in two areas of greater Athens. In: Cooper B, editor. Psychiatric Epidemiology: process and prospects. London: Croom Helm; 1987. p. 372-386. [ Links ]
28. Gournas G, Madianos M, Stefanis C. Psychological functioning and psychiatric morbidity in an elderly urban population in Greece. Eur Arch Psychiatry Clin Neurosci 1992; 242: 127-134. [ Links ]
29. Madianos M, Madianou D, Gournas G, Stefanis C. Multilevel approaches in the prevention of mental disorders in the community: The Athenian experience. In: Cooper B, Helgason T, editors. Epidemiology and prevention of mental disorders. London: Croom Helm; 1989. p. 255-271. [ Links ]
30. Madianos M, Economou M. The impact of a Community Mental Health Center on Psychiatric hospitalizations in two Athens areas. Community Ment Health J 1999; 35: 313-321. [ Links ]
31. Madianos M, Christodoulou G. Reform of the mental health care system in Greece, 1984-2006. Int. Psychiatry 2007; 4: 16-19. [ Links ]
32. Madianos M, Madianou D, Vlachonikolis J, Stefanis C. Attitudes towards mental illness in the Athens area: Implications for Community mental health intervention. Acta Psychiatr Scand 1987; 75: 158-165. [ Links ]
33. Madianos M, Economou M, Hatziandreou M, Papageorgiou A, Rogakou E. Changes in public attitudes towards mental illness the Athens area (1979/1980-1994). Acta Psychiatr Scand 1999; 99: 73-78. [ Links ]
34. Birchwood M, Todd P, Jackson C. Early intervention in psychosis: The critical period Hypothesis. Br J Psychiatry 1998; (Suppl. 33):S53-S58. [ Links ]
35. McGorry PD, Edwards J, Mihalopoulos C, Harrigan SM, Jackson HJ. EPPIC: An evolving system of early detection and optimal management. Schizophr Bull 1996; 22: 305-326. [ Links ]
36. Ito H, Mori T, Kumagai N, Miyauchi M, Marada S, Yamamura M, Nakauo R, Korita M, Sasaki Y. Changing patterns of mental health utilization in Hachijojima. Psychiatry Clin Neurosci 1995; 49: 185-187. [ Links ]
37. Madianos M, Stefanis C. Changes in the prevalence of symptoms of depression and depression across Greece. Soc Psychiatry Psychiatr Epidemiol 1992; 27: 211-219. [ Links ]
38. Olfson M, Marcus S, Druss B, Elinson L, Tanielian T, Pincus HA. National trends in the outpatient treatment of depression. JAMA 2002; 287: 203-209. [ Links ]
39. Dowrick C, Mateos-Ayuso JL, Barquero-Vazquez JL. From epidemiology to intervention for depressive disorders in the general population: The ODIN study. World Psychiatry 2002; 1: 169-174. [ Links ]
40. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003; 289: 3095-3105. [ Links ]
41. Brown GW, Harris, TO. Aetiology of anxiety and depressive disorders in an inner-city population. 1 early adversity. Psychol Med 1993; 23: 143-154. [ Links ]
42. Wilson IB, Cleary PD. Linking clinical variables with health related quality of life: a conceptual model of patient outcomes. JAMA 1995; 273: 59-65. [ Links ]
![]() Correspondence:
Correspondence:
Professor Michael G. Madianos
Zografou CMHC
42 Davaki - Pindou Street Zografou
157 73 Athens, Greece
E-mail: madianos@nurs.uoa.gr
Received 21 November 2007
Revised 2 October 2008
Accepted 17 October 2008