Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.25 no.2 Zaragoza abr./jun. 2011
https://dx.doi.org/10.4321/S0213-61632011000200002
Randomised controlled trial of cognitive-motivational therapy program for the initial phase of schizophrenia: a 6-month assessment
Carol Palma-Sevillano, PhD*,**; José Cañete-Crespillo, PhD**; Núria Farriols-Hernando, PhD*,**; Jordi Cebrià-Andreu, PhD*,***; Maria Michael, PhD****; Isabel Alonso-Fernández**; Maria Fernández-Vargas**; Gerard Segarra-Gutiérrez*
* Blanquerna Faculty of Psychology and Educational and Sport Sciences. Ramon Llull University, Barcelona. Spain
** Sanitary Consortium of Maresme. Mataro´s Hospital. Spain
*** Sant Miquel´s Primary Care Centre. Granollers. Barcelona. Spain
**** Department of Primary Care and General Practice. Primary Care Clinical Sciences Building. The University of Birmingham. United Kingdom
ABSTRACT
Background and Objectives: The aim of this study is to investigate the relative effectiveness of routine care (RC) in addition to a specific early intervention program (PIPE) compared to routine care alone.
Methods: A total of 34 participants in the initial phase of schizophrenia took part in randomized, single-blind controlled trial. Participants were randomized to receive either routine care (RC; n = 13) or routine integrated with Cognitive-Motivational Therapy (PIPE; n = 21). PIPE comprised individual and family Cognitive-Motivational therapy plus routine care for 12 months. In this paper we present preliminary results at 6 months after the beginning of the intervention. Clinical assessments were carried out at pre-treatment, and in this manuscript the results at 3 and 6 months after starting the intervention by external raters are presented, using the Positive and Negative Syndrome Scale, Brief Psychiatry Rating Scale, the Clinical Global Impression Scale, the Global Assessment of Functioning scale, and relapses. Mann-Whitney test and MANOVAs analysis for variance effects were used for the statistical analysis.
Results: Significant greater clinical effects were observed in those patients treated in RC+PIPE at three months from baseline assessment and at six months in PANSS scale (Mann-Whitney test; p < 0.000). Other benefits of the program included increase in global activity, reduced relapse rates, and reduction of the pharmacological treatment.
Conclusions: These findings show the effectiveness of a program of routine care integrated with cognitive-motivational interventions (individual and family therapy) over routine psychiatric care alone for patients who are in the initial phase of schizophrenia.
Key words: Schizophrenia; First-episode; Initial phase; Early intervention.
Introduction
Studies carried out to assess the effectiveness of cognitive-behavioral therapy (CBT) in the early phases of schizophrenia present very favorable results for symptomatic treatment1-11. A large body of recent research has arisen from the critical period hypothesis12 investigating interventions at the prodromal stage of schizophrenia, at the acute phase and the late recovery phase.
In relation to the post-acute and posterior phase, studies comparing CBT with other therapeutic modalities show their superiority in reducing clinical symptoms in short periods of time13-17.
Nowadays, many therapeutic programs use motivational interventions as a style and technical resource in the treatment of schizophrenia, like the treatment of associated substance use or programs addressed to promoting changes in behavior or attitudes towards intervention being two good examples1,8,18,19.
It is important to consider the intrinsic motivation in patients with schizophrenia because of its effectiveness in psychotherapy programs. This could be explained because the effect of the motivation over the learning processes during the therapy. According to relevant authors intrinsic motivation should enhance learning outcomes20,21. Other authors found that intrinsic motivation strongly mediated the relationship between neurocognition and psychosocial functioning22,23.
From this perspective, we designed an early intervention program for the initial phase of schizophrenia with the aim of assessing its effectiveness as an integrated (cognitive-motivational) psychological program versus the usual treatment of schizophrenia.
Materials and method
Design
A randomized, controlled, single-blind clinical trial was carried out. Patients and families were allocated either to the experimental intervention program plus routine care (PIPE) or to routine care alone (CG).
Selection of patients and group allocation
In this trial, inclusion criteria were: (a) patients should be at the initial phase of schizophrenia (<3 years from first episode), according to DSM-IV criteria, excluding the diagnosis of schizoaffective disorder, severe mental retardation and language difficulties were not included in the trial24; (b) they should have used the Mataró's psychiatry service (Barcelona). Diagnoses were established by two experienced professionals based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID)25 to improve reliability of diagnosis.
Participants were identified through a computerized database that collects all contacts with health services in a centralized manner regarding admissions into the Hospital of Mataró, visits to emergency services, outpatient consultations, visits to the Mental Health Centre, and admissions into the Day Hospital in Mataró. Patients and families were contacted and invited to participate in the study. Both patients and their family had to sign a consent form in order to be accepted into the trial. Patients and families were assessed by using different instruments: the Positive and Negative Syndrome Scale for Schizophrenia (PANSS)26, the Brief Psychiatric Rating Scale (BPRS)27, the Clinical Global Impression Scale28, and the Global Assessment of Functioning Scale (GAF)29. The assessment was carried out before being randomized to one of the two conditions in the clinical trial: (a) PIPE program plus routine care; and (b) only routine care. Randomization was carried out by an external researcher-epidemiologist through a computer program (SPSS.v.15) in charge of allocation.
Interventions
Integrated intervention program (PIPE)
The intervention program lasted for 12 months with a total number of 34 (weekly) sessions (of 45 minutes each), carried out in the Mental Health Centre. In this paper we only present preliminary results at 6 months after the beginning of the intervention.
The early intervention program PIPE combines three therapeutic components: psychoeducation, individual and family cognitive-motivational therapy. The PIPE program is described elsewhere30.
Motivational Intervention (MI) was used to increase motivation for change, help patients solve their ambivalences, promote their adherence to both pharmacological and psychological treatment, change substance use habits (in the case of user patients), increase daily life activities, and maintain hygiene habits (in the case of patients with difficulties)31.
Individual CBT were used to treat delirious ideas and hallucinations32. Family intervention aimed to promote communication attitudes that ensure an optimal family climate for the patient's recovery and the family's own adaptation to the illness. As in individual therapy, work with the family aimed to promote healthy and functional changes in accordance with MI style. The intervention program began with four psychoeducational sessions to provide the patient and family with information about the nature of the disease. The aim is to help the patient understand the illness by promoting his/her active participation in reducing the risk for relapses and the levels of social maladjustment. With regards to the family, the aim is to enhance their commitment to the patient's therapeutic process by avoiding blaming tendencies and reinforcing their motivation to help.
The individual cognitive intervention with a motivational style started during the third week of the program and lasted for 20 weeks approximately. Family therapy was carried out for 10 sessions. In some of them, the whole family (parents, siblings and patient) took part, whereas others involved family members only at the therapist's judgment.
Intervention was carried out by one therapist trained in the MI style and early psychological interventions to treat psychosis. Regular supervisions were carried out, some of them with audiovisual support.
Routine Care (RC)
The usual treatment for the initial phase of schizophrenia in the context of the Spanish Mental Health Care is pharmacological treatment as prescribed by the regular psychiatrist.
Assessment procedures and instruments
Assessments were carried out by a qualified external assessor in order to guarantee single-blinding and objectivity of results (a psychologist). They were carried out at three time periods: at pre-treatment (right before being allocated to one of the experimental conditions), 3 months after, and 6 months after baseline assessment.
The social and demographic characteristics of the patients and families were collected through a short questionnaire during the first interview.
Symptoms and Global Functioning
- Baseline assessment
To assess symptoms and global functioning, the Positive and Negative Syndrome Scale for Schizophrenia (PANSS), the Brief Psychiatric Rating Scale (BPRS), the Clinical Global Impression Scale, and the Global Assessment of Functioning Scale (GAF) were used.
- Assessments during the intervention (3 and 6 months after)
Three months after the beginning of the intervention, the BPRS was used in order to observe the patients' progress. Six months after, patients were assessed again using the baseline outcome measures relapse rates were also recorded during the study.
Relapses
Two strategies were used to record relapses aiming to avoid overlapping bias in the treatment of data.: (a) individual relapses which comprised (I) number and duration of inpatients admissions; (II) number and duration of outpatients admissions; (III) number of visits to emergency services due to deterioration of symptoms; and (IV) number and duration of deterioration of symptoms that require intervention by professionals (increase in/change of medication or non-scheduled visits; since de beginning of intervention to the follow up. If increase in medication is prescribed in the emergency room, both variables will be recorded. On the contrary, if the increase in medication is prescribed by the regular psychiatrist with the aim of preventing relapse in relation to current changes liable to affect the patient's status, then it will not be considered as a relapse. (b) Global relapses: if, in the context of a relapse, there is involvement of more than one of health care services listed above within the same period of time, this will be recorded as one single relapse (called "global"). The differentiation between the two strategies for this variable serves the purpose of avoiding bias in the treatment of the number of relapses. In the case that the patient shows a period of stability between the use of one service and another, they would be considered as two independent relapses.
Data analysis
Before the descriptive analysis of baseline, an analysis of scores was carried out, with statistical differences observed concerning the normal distribution of variables. For this reason, all analyses were carried out using non-parametrical procedures, including the analysis of covariance and Mann-Whitney U test (U) to compare both groups. Two-tailed tests of significance were used in all analyses. Multivariate analysis of Variance (MANOVAs) was used to compare differences in symptoms change between the PIPE and CG at 6 months follow-up. In order to control for the effect of psychotic symptoms, the PANSS baseline scores were used as a covariate in the MANOVAs. Doses of pharmacological treatment were converted to Chlorpromazine-equivalents doses (mg/day) in both groups and were also treated as a covariate33.
Results
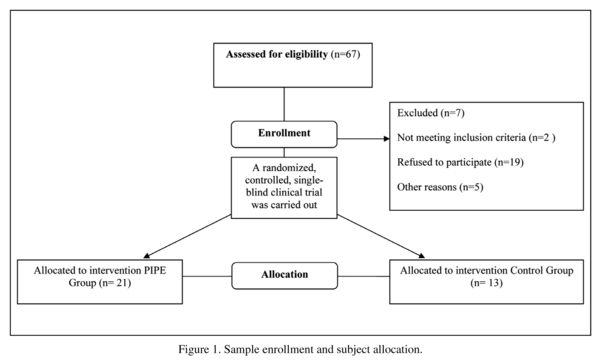
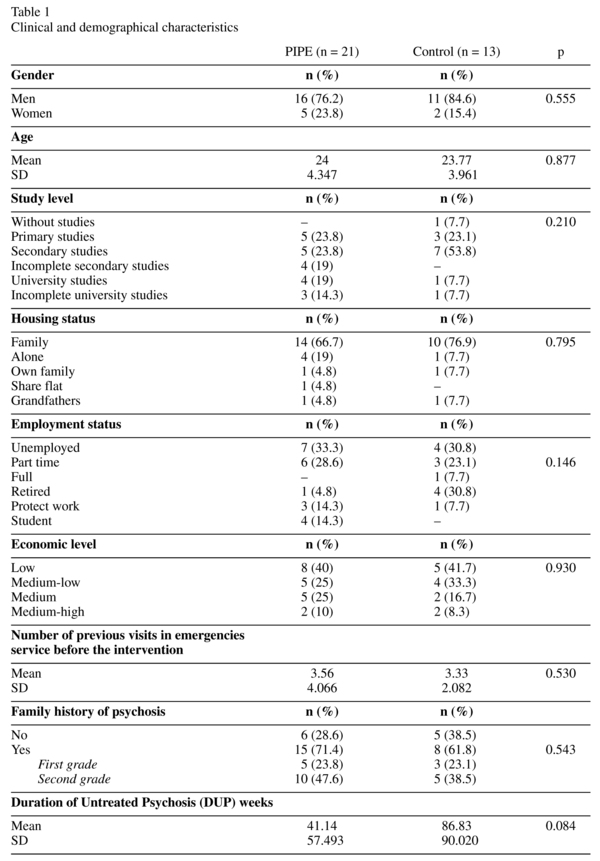
A total of 67 cases diagnosed with schizophrenic disorder meeting the inclusion criteria of this study were detected. During the enrollment process, 5 subjects moved out of area; 7 people could not be contacted; 19 did not agree to participate in the study because they did not think they had any mental illness; and 2 of them were false positives. The final sample of the study included by 34 patients allocated to the two experimental conditions: PIPE group (n = 21) and control group (n = 13) (see Figure 1). During the intervention, no patient dropped out. Data collection for the current results was completed two years after the first patient was included, because the sample inclusion was progressive during the program. The social, demographical and clinical characteristics were distributed homogeneously between groups (see Table 1).
Symptoms and functioning
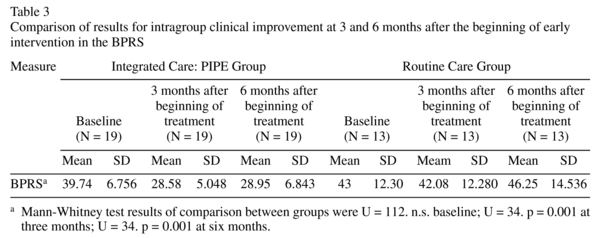
Table 2 shows scores in the clinical measures, global functioning and global clinical impression. An analysis of covariance was carried out with the scores of baseline assessment as covariables in order to compare two analyses: a) the effects between baseline assessments, 3 and 6 months after treatment; b) the effects between the groups of results with respect to baseline scores (see table 2 and 3).
Significant improvement was observed in all PANSS scales between baseline and 6 months in the PIPE group.
1. Positive scale: there were remarkable differences between the intervention and control group with the former scoring lower compared to the latter (adjusted mean = 7.28, SE = 1.103, versus adjusted mean = 36.94, SE = 8.427) (F = 7.436, df = 1, p < 0.011).
2. Negative scale: adjusted mean = 19.5, SE = 2.578, versus adjusted mean = 37.69, SE = 6.811; (F = 79.341, df = 1, p < 0.000).
3. General psychopathology scale: adjusted mean = 5.74, SE = 1.15, versus adjusted mean = 43.52, SE = 9.551; (F = 22.8, df = 1, p < 0.000).
The main results of MANOVA analysis are shown in the Table 4. We included baseline assessments, pharmacological treatment and DUP into the variance model.
We observed heterogeneous values for DUP in both groups (PIPE mean = 41.14 weeks; RC mean = 86.83). No significant differences were found in bivariate analysis, but the clinical difference was evident and it was indicated to include the DUP values into de variance model to observe the effect in groups' evolution.
The multivariate test showed a differential effect on the independent variable values in to design model (Lamda = 0.467; F = 3; p = 0.000; η = 0.603). The observed potency was 0.989. The effect size showed a 60% of the variance is explained by the group effect.
Global Functioning
High scores were detected by GAF scale in PIPE group, indicating an increase in activity, compared with the control group. Differences were significant at 6 months (adjusted mean = 66.43, SE = 2.456, versus adjusted mean = 45, SE = 5) (F = 22.813, df = 1, p < 0.000). Moreover, in the global clinical impression assessments, the PIPE group scored significantly lower compared to the control group (adjusted mean = 3.47, SE = 0.118, versus adjusted mean = 4.72, SE = 0.351) (F = 30.856, df = 1, p < 0.000). Lower scores in that scale mean a better global clinical impression assessed by external rates.
Brief Psychiatric Rating Scale
Another interesting result is shown by the BPRS scores, as this scale allows us to obtain clinical improvement scores at 3 months (Table 3). Results are similar to those of PANSS scores, but their specific contribution is that they allow us to observe this significant improvement just 3 months after the beginning of intervention (adjusted mean = 28.39, SE = 1.57, versus adjusted mean = 46.11, SE = 4.196) (F = 6.772, df = 1, p < 0.015).
Relapses
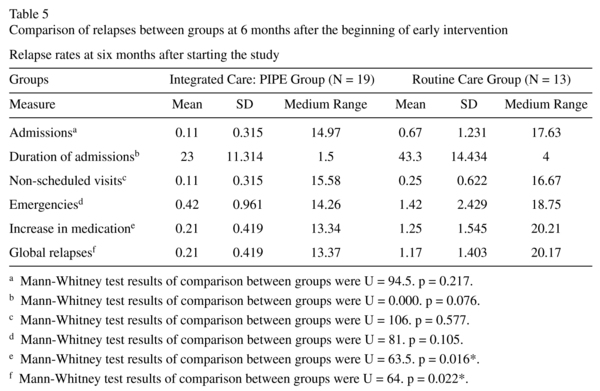
After 6 months of treatment, 24% of patients in the control group were admitted into hospital in comparison to 10.5% of the group receiving early intervention; however this difference is not statistically significant (χ2 = 0.922; p = 0.337) (see Table 5).
There were no significant differences in the frequency of day hospital stays between the PIPE group and the CG. The same was observed when assessing frequency of non-scheduled visits to other services. The same frequency is observed for patients (n = 2) that go to the mental health centre in a non-scheduled manner. No significant differences (χ2 = 2.264; p = 0.132) were also observed in the frequency of visits to emergency services at 6 months between the PIPE group (21.1%) and the CG (46.2%).
However, significantly less participants in the PIPE group (21.1%) compared to the CG (53.8%) required increase in medication. This difference in frequencies is statistically significant (χ2 = 3.680; p = 0.05). In the PIPE group a 72% of the prescriptions were done by their regular psychiatrist and the 28% in emergency unit. On the other hand, we observed a 64% of the increase prescriptions in CG by emergency unit (the 36% was prescribed by their regular psychiatrist).
With regards to global relapses, there are highly significant differences between two groups (χ2 = 5.398; p = 0.02). 21.1% of patients in the PIPE group were recorded as having global relapses in contrast to the 61.5% in the control group. These data imply the presence of two or more of the outcome measures used in the register of relapses in the same period of time.
Discussion
Many studies conducting CBT at the initial phase of schizophrenia present similar results when comparing the experimental and control groups and their separate evolution with regards to positive symptoms and lower drop-out rates9,15,34,35. However, other studies do not find these significant differences in the improvement of positive symptoms14,17 probably because their comparison groups are receiving, along with the regular treatment, problem-solving training or counseling interventions. Nevertheless, the three studies have pointed at the clinical improvement of the group receiving cognitive therapy in relation to other modalities.
In the present study, there are very favorable results just three months after the beginning confirming previous studies9.
Findings showed an increase in global activity and global clinical impression in the PIPE group compared to the control group which supports the findings of previous clinical trials1,8,36.
Remarkably, it is difficult to find studies conducting an intervention similar to the one presented here of a cognitive-motivational nature. In fact, we carried out a literature review to assess current opinions in this field. These issues make it clear that it is difficult to reach solid conclusions in this field due to the heterogeneity of the concept and the difficulty in writing manuals on this kind of intervention.
Nevertheless in Barrowclough's study1 the MI proposed shares similar characteristics to the one presented here. However, the study design is different as her sample is not in the initial phase of the disease, and they have dual diagnoses.
The work carried out by Tarrier's group10 shows assessments after 9 and 12 months of intervention with highly significant results also in all PANSS and global clinical impression scales. When assessing relapses in a short period of time such as 6 months, no significant differences are likely to be found in most of the measures explored. The results of our study show higher means in the control group in all the assessed measures. With regards to the number of hospital admissions, number of non-scheduled visits, visits to the emergency service, and duration of hospital stays. However, the frequency of global relapses and of the number of times when an increase in medication is needed shows statistically significant difference in the PIPE group in comparison to the control group; these results are similar to those of previous studies14.
Something similar happens, as there is a lower number and less duration of hospital stays in the group receiving CBT, although the levels of statistical significance do not reach such values as to reach more conclusive statements. Most studies applying CBT find this statistical significance in the longer term1,37.
With regards to the limitations of this study, we have to state that the trial is carried out using a cognitive-motivational intervention, one of the most important ingredients of which is the therapist's style. This factor makes this study hardly comparable; in fact, there are few studies with such an intervention. Dr. Barrowclough and her team in Manchester show the effect of their psychological intervention in a very similar trial1. Nevertheless, the difficulty of both studies lies in being able to discern whether the improvement is due to the fact that adherence to treatment is enhanced or to the intervention as a whole.
On the other hand, the reduced size of the sample forces us to interpret results with some caution. Applying strict inclusion criteria in combination with the lack of insight reported by a significant number of potential participants resulted in loss of participants.
Furthermore, the reduced size of the sample has not allowed the dependent variables to meet normality criteria in a regular manner, and for this reason in the phase of statistical analysis some decisions were made in this respect, such as the use of non-parametrical tests.
In short, our study shows that the Early Intervention Program for Schizophrenia (PIPE) has a high impact on the clinical improvement and a mild impact on relapses after 6 months of intervention. In future studies, we will assess the impact of the intervention in the long term and during follow-up, as well as explore the relative efficiency of every component in the integrated interventions.
Conclusions
Results obtained in all outcome measures in our study show the positive impact that early intervention has at the initial stage of schizophrenia concerning clinical improvement, global impression, and global activity after three and six months of treatment. The findings of this study in relation to the rest of published works encourage us to wait. The assessment of relapses seems to require time sensitivity. Presenting results after six months of intervention limits this possibility and, therefore, this will be an aspect to be assessed in a later period.
Acknowledgements
We would like to particularly thank the patients that took part in this study for their patience in attending the sessions, developing all the assessment tests and making this work possible.
This work was carried out thanks to the pre-doctoral grant for the Training of Research Personnel (FI) 2003FI-0932 awarded by the Departament d'Universitats, Recerca i Societat de la Informació (DURSI, Generalitat of Catalonia). Thanks too to Seny Foundation for Schizophrenia for the economic support.
Abbreviations:
PIPE: (it) refers to integrated program with cognitive-motivational therapy plus routine care.
CG: (it) refers to control group.
References
1. Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O'Brien, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry 2001; 158(10): 173-179. [ Links ]
2. Bechdolf A, Knost B, Kuntermann C, Schiller S, Klosterkotter J, Hambrecht M. A randomized comparison of group cognitive-behavioural therapy and group psychoeducation in patients with schizophrenia. Acta Psychiatr Scand 2004; 110(1): 21-28. [ Links ]
3. Drury V, Birchwood M, Cochrane R, Macmillan F. Cognitive therapy and recovery from acute psychosis: a controlled trial. I. Impact on psychotic symptoms. Br J Psychiatry 1996; 169(5): 593-601. [ Links ]
4. Drury V, Birchwood M, Cochrane R, Macmillan F. Cognitive therapy and recovery from acute psychosis: a controlled trial. III. Five-year follow-up. Br J Psychiatry 2000; 177: 8-14. [ Links ]
5. Drury V, Birchwood M, Cochrane R, Macmillan F. Cognitive therapy and recovery from acute psychosis: a controlled trial. II. Impact on recovery time. Br J Psychiatry 1996; 169(5): 602-607. [ Links ]
6. Freeman D, Garety P, Fowler D, Kuipers E, Dunn G, Bebbington P, et al. The London-East Anglia randomized controlled trial of cognitive-behaviour therapy for psychosis. IV: Self-esteem and persecutory delusions. Br J Clin Psychol 1998; 37(Pt 4): 415-430. [ Links ]
7. Gumley A, O'Grady M, McNay L, Reilly J, Power K, Norrie J. Early intervention for relapse in schizophrenia: results of a 12-month randomized controlled trial of cognitive behavioural therapy. Psychol Med 2003; 33(3): 419-431. [ Links ]
8. Haddock G, Barrowclough C, Tarrier N, Moring J. Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18-month outcomes of a randomised controlled trial. Br J Psychiatry 2003; 183: 418-426. [ Links ]
9. Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P, Kingdon D, et al. Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes. Br J Psychiatry Suppl 2002; 43: 91-97. [ Links ]
10. Tarrier N, Lewis S, Haddock G, Bentall R, Drake R, Kinderman P, et al. Cognitive-behavioural therapy in first-episode and early schizophrenia. 18-month follow-up of a randomised controlled trial. Br J Psychiatry 2004; 184: 231-239. [ Links ]
11. Trower P, Birchwood M, Meaden A, Byrne S, Nelson A, Ross K. Cognitive therapy for command hallucinations: randomized controlled trial. Br J Psychiatry 2004; 184: 312-320. [ Links ]
12. Birchwood M, Todd P, Jackson C. Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl 1998; 172(33): 53-59. [ Links ]
13. Garety P, Fowler D, Kuipers E, Freeman D, Dunn G, Bebbington P, et al. London-East Anglia randomized controlled trial of cognitive-behavioural therapy for psychosis. II: Predictors of outcome. Br J Psychiatry 1997; 171: 420-426. [ Links ]
14. Haddock G, Tarrier N, Morrison AP, Hopkins R, Drake R, Lewis S. A pilot study evaluating the effectiveness of individual inpatient cognitive-behavioural therapy in early psychosis. Soc Psychiatry Psychiatr Epidemiol 1999; 34(5): 254-258. [ Links ]
15. Kuipers E, Garety P, Fowler D, Dunn G, Bebbington GDP, Freeman D, et al. London-East Anglia randomized controlled trial of cognitive-behavioural therapy for psychosis. I: effects of the treatment phase. Br J Psychiatry 1997; 171: 319-327. [ Links ]
16. Tarrier N, Beckett R, Harwood S, Baker A, Yusupoff L, Ugarteburu I. A trial of two cognitive-behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients: I. Outcome. Br J Psychiatry 1993; 162: 524-532. [ Links ]
17. Tarrier N, Sharpe L, Beckett R, Harwood S, Baker A, Yusopoff L. A trial of two cognitive behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients. II. Treatment-specific changes in coping and problem-solving skills. Soc Psychiatry Psychiatr Epidemiol 1993; 28(1): 5-10. [ Links ]
18. Kavanagh DJ, Young R, White A, Saunders JB, Wallis J, Shockley N, et al. A brief motivational intervention for substance misuse in recent-onset psychosis. Drug Alcohol Rev 2004; 23(2): 151-155. [ Links ]
19. Rusch N, Corrigan PW. Motivational interviewing to improve insight and treatment adherence in schizophrenia. Psychiatr Rehabil J 2002; 26(1): 23-32. [ Links ]
20. Medalia A, Choi J. Cognitive remediation in schizophrenia. Neuropsychol Rev 2009; 19(3): 353-364. [ Links ]
21. Medalia A, Choi J. The role of motivation and engagement in successful cognitive training with schizophrenia patients. Schizoph Bull 2009; 35(Suppl 1): 355. [ Links ]
22. Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizoph Res 2008; 105(1-3): 95-104. [ Links ]
23. Barch DM. The relationship among cognition, motivation, and emotion in schizophrenia: how much and how little we know. Schizoph Bull 2005; 31(4): 875-881 [ Links ]
24. Perona S, Cuevas C, Vallina O, Lemos S. Terapia cognitivo-conductual de la esquizofrenia. Madrid: Minerva Ediciones; 2003. [ Links ]
25. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders-Administration Booklet. Washington DC: American Psychiatric Association; 1997. [ Links ]
26. Peralta V, Cuesta MJ. Validación de la escala de los síndromes positivo y negativo (PANSS) en una muestra de esquizofrénicos españoles. Actas Luso Esp Neurol Psiquiatr Cienc Afines 1994; 22(4): 171-177. [ Links ]
27. Overall JE, Gorham DR. Escala breve de Evaluación Psiquiátrica (Brief Psychiatric Rating Scale, BPRS). Psychological Reports 1962; 10: 799-812. [ Links ]
28. National Institute of Mental Health. 028 CGI. Clinical Global Impressions. In: Guy W, ed. ECDEU Assesment Manual for Psychopharmacology, rev ed. Rockville, Maryland; 1976; p. 217-222. [ Links ]
29. American Psychiatric Association. Escala de Evaluación de la Actividad Global EEAG. Manual diagnostico y estadístico de los trastornos mentales (4 ed.). Barcelona: Masson; 1995. [ Links ]
30. Palma C. Efectividad de un programa de intervención precoz en la fase inicial de la esquizofrenia: una evaluación a los 6 meses. Blanquerrna Faculty of Psychology and Educational and Sports Sciences, Ramon Llull University. Barcelona; 2005. [ Links ]
31. Palma C, Cebrià J, Farriols N, Cañete J, Muñoz E. La entrevista motivacional con el paciente esquizofrénico. Psiquis 2005; 26(3): 109-120. [ Links ]
32. Birchwood M, Tarrier N. El tratamiento psicológico en la esquizofrenia. Barcelona: Ariel; 1995. [ Links ]
33. Beers MH, Berkow R. El Manual Merck de diagnóstico y tratamiento. 10a ed. Madrid: Harcourt; 1999. [ Links ]
34. Garety PA, Kuipers L, Fowler D, Chamberlain F, Dunn G. Cognitive behavioural therapy for drug-resistant psychosis. Br J Med Psychol 1994; 67 (Pt 3): 259-271. [ Links ]
35. Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry. 2000; 57(2): 165-172. [ Links ]
36. Hayward P, Chan N, Kemp R, Youle S. Medication self-management: A preliminary report on an intervention to improve medication compliance. J Ment Health 1995; 4(5): 511-517. [ Links ]
37. Buchkremer G, Klingberg S, Holle R, Schulze MH, Hornung WP. Psychoeducational psychotherapy for schizophrenic patients and their key relatives or care-givers: results of a 2-year follow-up. Acta Psychiatr Scand 1997; 96(6): 483-491. [ Links ]
![]() Correspondence:
Correspondence:
Carol Palma Sevillano
Blanquerna Faculty of Psychology and Educational
and Sport Sciences. Ramon Llull University
C/ Císter, 34. 08022 Barcelona (Spain)
Tel: (+0034) 616818808
Fax: 93.253.30.31
E-mail: carolinaps@blanquerna.url.es
Received: 13 January 2010
Revised: 13 October 2010
Accepted: 18 October 2010