My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
The European Journal of Psychiatry
Print version ISSN 0213-6163
Eur. J. Psychiat. vol.27 n.4 Zaragoza Oct./Dec. 2013
https://dx.doi.org/10.4321/S0213-61632013000400002
Incidence of psychoses among drug dependent patients in primary care with no psychiatric history: A retrospective observational matched-cohort study
Martin Frisher*; Orsolina I. Martino**; James Bashford*; Ilana Crome*** and Peter Croft****
*School of Pharmacy, Keele University, Staffordshire. United Kingdom
**Wallsall Healthcare NHS Trust, Walsall, West Midlands. United Kingdom
***Academic Psychiatry Unit, St George's Hospital, South Staffordshire and Shropshire Healthcare NHS Foundation Trust, Corporation Street, Stafford. United Kingdom
****Primary Care Sciences Research Centre, Keele University, Staffordshire. United Kingdom
The study was funded by the North Sta-ffordshire Health Care Consortium. The Consortium had no role in the study design; in the collection, analysis, and interpretation of the data; in the preparation of the manuscript; or in the decision to submit the article for publication.
ABSTRACT
Background and Objectives: While several studies have indicated a link between illicit drug use and the development of psychosis, the confounding role of pre-existing psychiatric illness is unclear. This study controls for this factor to a greater extent than has hitherto been possible, using a retrospective observational matched-cohort design controlling for age, gender, socioeconomic status and prior psychiatric illness.
Methods: 592 cases (diagnosed with drug misuse/dependence) and 592 controls (no recorded history of drug misuse/dependence) were drawn from all patients aged 16-44 in 183 practices within the General Practice Research Database (UK). On study entry, cases and controls had never had a psychiatric diagnosis since registering with their practice. The average look-back period was 17.7 years. The main outcome measure was diagnosis of psychosis (including schizophrenia) from study entry onwards.
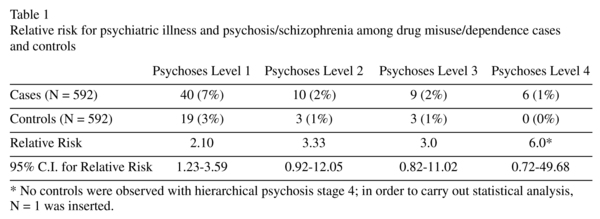
Results: Patients with a drug misuse/dependence diagnosis are significantly more likely to be diagnosed with psychosis than those with no drug misuse/dependence history (RR = 2.10, 95% C.I. = 1.23-3.59) with the relative risk increasing as the definition of psychosis gets narrower.
Conclusions: This study has established that, when the confounding presence of previous psychiatric illness is removed, the onset of problematic substance misuse severe enough to warrant primary care consultation is a risk factor for future onset of first-ever psychotic illness. Thus, there is a distinct sub-group of psychotic patients among whom drug misuse/dependence, with no prior psychiatric illness, is a risk factor for the development of psychoses.
Key words: Drug misuse; Epidemiology; General Practice; Mental Health; Primary Care.
Introduction
The role of drug misuse as a cause of psychiatric illness has been highlighted as a key consideration in policy concerning the classification of illegal drugs1. Much of the research on this topic focuses specifically on the risk of developing psychosis as a result of drug misuse, most notably cannabis. While there is still considerable debate on this issue2,3, a recent editorial cites several studies indicating that "regular use of cannabis is associated with an increased risk of psychotic symptoms and disorders in the general population"4. The editorial also casts doubt on the hypothesis that this could be due to uncontrolled confounding as a result of prior psychiatric illness and suggests that the onus is on those who advocate confounding to provide evidence to support this hypothesis.
Some studies have also estimated the population attributable risk (PAR), which is an estimate of the proportion of schizophrenia/psychosis that may be attributable to cannabis use. In reviewing these estimates, McLaren et al.5 conclude that 8-13% represents a conservative estimate for the PAR. In other words, 8-13% of psychosis could be prevented if no-one used cannabis. Another study states that 25% of incident schizophrenia cases in 2010 in the UK may be caused by cannabis use6. There are no precise estimates for the proportion of psychosis that may be attributable to other substances, although one review concluded that cocaine, amphetamines, and alcohol use are associated with an increased risk of psychosis7. However despite reports of a substantial rise in cannabis use in the 1980s and 1990s6, the incidence and prevalence of psychosis did not increase over the 1996-2005 study period in the UK8,9. Studies of psychotic outcomes relative to cannabis10,11 or other drug use, e.g. amphetamines, cocaine or heroin12,13 have tended to define drug use per se as the exposure, rather than problematic use or dependence. Research indicates that there is a dose effect for cannabis, i.e. regular or heavy cannabis use is more strongly associated with incident psychosis4. However, the risk of confounding is possibly more pronounced, as very often these cases present later in their drug using career when it is harder to establish whether there has been pre-existing psychiatric illness. A stronger test of the hypothesised link between drug misuse/dependence and psychotic illness could focus on consultation data in health care systems where precise dates of diagnosed drug misuse/dependence and psychiatric illness are available.
The present study is the first to utilise consultation data from primary care in a matched-cohort design to address this question. The study compares the incidence of psychiatric illness following first ever diagnosis of drug misuse/dependence with that in controls with no history of drug misuse. There are three main strengths to this design. First, matching cases and controls on age, gender and practice to control for socio-demographic effects. Second, ensuring that both cases and controls were registered for at least 5 years and had no psychiatric diagnoses prior to the point of study entry provides a more accurate measure of incidence, and avoids potential bias from cases already having a psychiatric illness before their incident drug misuse/dependence diagnosis. Thirdly, since almost all psychiatric illness in the UK, apart from emergency admissions for acute psychosis, are referred to psychiatrists from general practice, a past history of psychiatric illness, especially minor illness, is much more likely to be completely recorded in general practice records than in any other source of data. Although GP-diagnosed drug misuse/dependence is certainly an under-representation of illicit drug use in the general population as a whole, data from general practice provide a relatively clean epidemiological measure of drug misuse, "problematic" enough to be diagnosed by the GP14.
Methods
Sample
The data for this study come from the General Practice Research Database (GPRD). The GPRD is owned by the Medicines and Healthcare Products Regulatory Agency (MHRA). The data were obtained under a license from the Medical Research Council. The study cohort comprises all patients aged 16-44 in 183 GPRD practices. These practices continuously submitted data from 1996 to 2005. The practices are drawn from the 9 National Health Service (NHS) Regional Office areas for England, plus Scotland, Wales and Northern Ireland.
Cases were defined as patients with a diagnosis or treatment of drug misuse/dependence occurring anywhere in their records before 31/12/2005. The point of study entry was defined as the date of their first ever (i.e. incident) drug misuse/dependence diagnosis. Cases had to be free of any psychiatric event prior to the incident diagnosis. Thus at study entry, cases had never had a drug misuse/dependence or psychiatric diagnosis. Drug misuse/dependence events were taken from diagnostic and treatment (i.e. prescription) events; relevant prescriptions were those for opioid dependence (e.g. methadone). Psychiatric events were taken from diagnoses only.There are 241 diagnostic codes for drug misuse/dependence disorders and 12 codes for related prescriptions, and 1,693 codes for psychiatric disorders, of which 595 relate to psychoses or schizophrenia (hereafter referred to as psychoses). Eligible cases had to be registered with a recording practice on the database for at least 5 years prior to the point of study entry.
Controls were defined as having no diagnosis of drug misuse/dependence anywhere in their medical records. These were matched to cases by gender, year of birth and practice. For each control, the point of study entry was defined as the date of the incident drug event for their corresponding matched case. They had to be free of any psychiatric event prior to the point of study entry. Eligible controls had to be registered for at least 5 years prior to the point of study entry.
These selection criteria resulted in a final number of 592 cases of GP-recorded drug misuse/dependence, who had at least 5 years free of GP-recorded psychiatric illness and drug misuse/dependence prior to the incident drug misuse/dependence diagnosis. These were matched by age, gender and practice to 592 controls. Controls were registered for at least 5 years with no record of drug misuse/dependence at any point, and no recorded psychiatric illness prior to the date of the incident substance misuse event in their matched case.
Hierarchical psychosis analysis
Coding of psychoses diagnoses
39 codes were used within the sample of 592 cases and their matched controls to record psychoses. The 39 codes were shown to a panel of five clinicians and general practitioners, with the following statements (to be marked "yes" or "no" for each code): statement A "You might use this code for psychosis" and statement B "Most patients with this code will have had psychosis". Based on the responses, and following discussion with additional expert and GP opinion, three codes were removed and the remaining 36 codes grouped into the following hierarchy for analysis:
1. Symptoms/diagnoses which may be applied to individuals with psychosis, excluding those specific to senile/presenile dementia (36 codes);
2. Excludes all depression-related diagnoses without mention of a psychotic element (24 codes);
3. Further excludes depression-related diagnoses with a psychotic element (21 codes);
4. Further excludes all remaining ambiguous codes, i.e. those representing symptoms/diagnoses which can on occasion indicate psychosis but where majority opinion was that on most occasions they will not do so. This final list therefore comprised symptoms/diagnoses that would, in most cases, definitely correspond to a diagnosis of psychosis (15 codes).
Analysis
The relative risk for developing psychoses among cases and controls was computed using SPSS 17. Population Attributable Risk (PAR) was calculated using the formula developed by Levin for cohort studies15. PAR may be thought of as the decrease in GP recorded psychoses if GP recorded drug misuse/dependence were eliminated from the whole population15.
Results
At study entry, cases and controls had been registered for an average of 17.0 and 18.5 years respectively. During this period cases and controls were free from drug misuse/dependence & psychiatric diagnoses. The average age of cases and controls at the point of study entry was 29 years.
Cases were significantly more likely to progress to psychoses (level 1) than controls (see table 1). The relative risk was higher for psychoses levels 2/3 compared to level 1 and for level 4 compared to the other levels. However, these results did not attain statistical significance for psychoses levels 2-4 (see table 1).
Based on the relative risk of psychoses and the rate of diagnosed drug misuse/dependence observed in a previous study using the same database14, the Population Attributable Risk (PAR) is shown in table 2. Model 1, is based on a diagnosis rate of drug/misuse dependence without prior psychiatric illness of 0.15%. Model 2 is based on the diagnosis rate for all patients diagnosed with drug/misuse dependence (irrespective of whether they have had previous psychiatric illness). Model 3 is based on self-reported class A drug use in the last month in the general population, while Model 4 is based on self-reported cannabis use in the last month in the general population.
According to model 1 (where the proportion of the population that has the risk characteristic is 0.15%), the PAR is 0.16%. In other words, less than 1% of psychosis would be prevented if there was no exposure to this form of risk (i.e. GP-recorded drug/misuse dependence without prior psychiatric illness). In fact, the majority of incident cases of drug/misuse dependence in this UK GP database have prior psychiatric illness. Table 2 shows this result alongside other drug use scenarios including any cannabis use in the last month.
Discussion
Our study has clearly established that, when the confounding presence of previous psychiatric illness is removed, the onset of problematic substance misuse severe enough to warrant primary care consultation is a risk factor for future onset of first-ever psychotic illness. However, this relationship would only explain a small proportion of all psychosis that occurs in persons who have substance misuse, and more research is needed to disentangle the pathways of risk in persons who constitute the majority of those developing psychosis in the presence of substance misuse who have a previous history of psychiatric illness and have not consulted health care about their substance misuse.
The matched-cohort design controls for the effects of age, gender and socioeconomic status, and the exclusion of patients with prior psychiatric diagnoses means that we have a relatively clean measure of the incidence of psychiatric illness within the study sample. While other studies have attempted to control for prior psychoses, this study controlled for any prior psychiatric diagnoses. At study entry, cases had been registered for an average of 17 years and during this time had never been diagnosed with any form of psychiatric illness or drug misuse/dependence.
It is nevertheless necessary to address limitations of general practice data in estimating risks in relation to drug misuse, and emphasise the point that these findings relate to a specific population, i.e. patients with GP-diagnosed drug misuse. In other words, only those with a problem severe enough to be consulting their GP (e.g. addiction, or receiving methadone) will be recorded. Similarly, controls are defined only as those without a diagnosis of drug misuse; this does not necessarily mean that they have never used drugs. Thus the findings only provide a measure of the risk for psychiatric illness with drug misuse/dependence on a level problematic enough to consult the GP; they cannot be used to draw conclusions concerning the risk among the general population, or with more "casual" drug use. Most of the drug misuse/dependence diagnoses on the GPRD are not for specific drugs, but for "drug abuse" or "drug addiction", therefore it is not possible to stratify our analysis by the type of drug involved (e.g. cannabis or amphetamines). In addition, the database contains no information about the precise nature and extent of problematic drug use. Another issue is the dropout rate from the study. By the end of 2005, 15.2% of cases and 4.3% of controls left the database before the end of 2005 without a psychiatric diagnosis. 37% of censored cases occurred within the first two years, compared to 15% of censored controls. This indicates that early departure was more frequent and more rapid among the cases. This could introduce bias if these cases are more likely to have psychoses. Thus the relative risk estimates may be conservative.
The key aspect of these findings relates to the long period where cases and controls were free of psychiatric illness. This lends a high degree of confidence to the elevated risk of psychiatric illness free from confounding by prior psychiatric illness. However this risk must be seen in the context of the risk exposure captured in this study. This risk is diagnosed drug misuse/dependence, the vast majority of which relates to opiate use rather than cannabis use. The 5 year rate of diagnosed drug misuse/dependence in GPRD is 0.4%. It should be emphasised that the results of this study relate solely to a group of cases with no recorded previous diagnosis of psychiatric illness. An earlier analysis using the same database found that where patients have both psychosis and substance abuse diagnosis, the former occurs first in 60% of cases17.
This study found indications that the more "severe" the classification of psychosis, the greater the relative risk among drug misusers, and the greater the proportion of psychosis cases that can be potentially attributed to drug misuse/dependence. However, as noted above, these findings did not attain statistical significance and future work could focus on this issue. In conclusion, the main strength of this study lies in its methodological rigour. All participants were free from diagnosed psychiatric illness for a long period of time at the point of study entry. Thus the results indicating elevated risk of psychoses are likely to be robust with regard to the confounding influence of earlier psychiatric illness. 7% of patients presenting with proble-matic drug use, and no prior psychiatric illness, are likely to progress to psychoses-level 1 and 1% to psychoses-level 4. This study has clarified the role of drug misuse/dependence in psychoses/schizophrenia by confirming that there is a relationship, independent of prior psychiatric illness. While the majority of psychoses are predated by psychiatric illness, there is a distinct group among whom drug misuse/dependence, with no prior psychiatric illness, is a risk factor for the development of psychoses.
These findings have clinical implications for the treatment of drug misusers. The data support the view that mental health issues are a key factor in assessing drug-related harm18 and the specific needs of this particular population need to be taken into account in the planning of treatment services. Moreover, the fact that these individuals are also more likely to leave their practice after short periods possibly reflects the chaotic nature of their condition; given that this may make them more difficult to engage in and subsequently retain in treatment, it is likely to impact upon the effectiveness of such services.
Acknowledgements
We are extremely grateful to Efrosis Setakis, Tim Williams and Jon Ford at the Medicines & Healthcare Products Regulatory Agency (MHRA). The MHRA team provided the data for the study under an MRC license (protocol 786) granted to the authors. The authors would also like to thank all contributing general practitioners and their patients.
References
1. HM Government, 2008. Government response to the recommendations made by the Advisory Council on the Misuse of Drugs in its report Cannabis: Classification and Public Health. Produced by COI on behalf of HM Government. October 2008. Ref: 291042. [ Links ]
2. Minozzi S, Davoli M, Bargagli AM, Amato L, Vecchi S, Perucci CA. An overview of systematic reviews on cannabis and psychosis: discussing apparently conflicting results. Drug Alcohol Rev 2010; 29: 304-317. [ Links ]
3. Ben Amar M., Potvin S. Cannabis and psychosis: what is the link? J Psychoactive Drugs 2007; 39: 131-142. [ Links ]
4. Hall W, Degenhardt L. Cannabis and the increased incidence and persistence of psychosis. BMJ 2011; 342: d719. [ Links ]
5. McLaren J, Silins E, Hutchinson D. Assessing evidence for a causal link between cannabis and psychosis: A review of cohort studies. Int J Drug Policy 2010; 21: 10-19. [ Links ]
6. Hickman M, Vickerman P, Macleod J, Kirkbride J, Jones PB. Cannabis and schizophrenia: model projections of the impact of the rise in cannabis use on historical and future trends in schizophrenia in England and Wales. Addiction 2007; 102: 597-606. [ Links ]
7. Thirthalli J, Benegal V. Psychosis among substance users. Curr Opin Psychiatry 2006; 19: 239-245. [ Links ]
8. Frisher M, Crome I, Martino O, Croft P. Assessing the impact of cannabis use on trends in diagnosed schizophrenia in the United Kingdom from 1996 to 2005. Schizophrenia Res 2009; 113: 123-128. [ Links ]
9. Nutt D. Government vs science over drug and alcohol policy. Lancet 2009; 374: 1731-1733. [ Links ]
10. Fergusson DM, Horwood LJ, Ridder EM. Tests of causal linkages between cannabis use and psychotic symptoms. Addiction 2005; 100: 354-366. [ Links ]
11. Andreasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet 1987; 2: 1483-1486. [ Links ]
12. Coulston CM, Perdices M, Tennant CC. The neuropsychology of cannabis and other substance use in schizophrenia: Review of the literature and critical evaluation of the methodological issues. Aust N Z J Psychiatry 2007; 41: 869-884. [ Links ]
13. Holtmann M, Becker K, Hartmann M. Gibt es einen zeitlichen zusammenhang von substanzmissbrauch und psychose bei jugendlichen? (Is there a temporal correlation between substance abuse and psychosis in adolescents?) Z Kinder Jugendpsychiatrie 2002; 30: 97-103. [ Links ]
14. Frisher M, Crome I, Macleod J. Substance misuse and psychiatric illness: prospective observational study using the general practice research database. J Epidemiol Community Health 2005; 59: 847-850. [ Links ]
15. Lilienfeld A, Lilienfeld D. Foundations of Epidemiology. New York: Oxford University Press; 1980. [ Links ]
16. Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 2002; 325: 1212-1213. [ Links ]
17. Frisher M, Crome I, Millson D, Collins J, Conolly A. A national epidemiological study of comorbid substance abuse and psychiatric illness in primary care between 1993-1998 using the General Practice Research Database. 2003. Home Office, London (dmri.lshtm.ac.uk/docs/frisher_summary.pdf). [ Links ]
18. Best D, Gross S, Vingoe L, Witton J, Strang J. Dangerousness of drugs: A guide to the risks and harms associated with substance misuse. London: National Addiction Centre, Department of Health; 2003. [ Links ]
![]() Correspondence:
Correspondence:
Martin Frisher
School of Pharmacy
Keele University
Staffordshire, ST5 5BG
United Kingdom
Tel: 01782 733 568
Fax: 01782 713 586
E-mail: m.frisher@keele.ac.uk
Received: 16 August 2012Revised: 21 January 2013
Accepted: 15 April 2013