Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.28 no.3 Zaragoza jul./sep. 2014
https://dx.doi.org/10.4321/S0213-61632014000300003
Verbal fluency in chronic schizophrenia and severity of psychotic symptoms. Consideration of their relationship with errors in the tasks
Flavia S. Galaverna*; Carlos A. Morra** and Adrián M. Bueno*
* Laboratory of Experimental Psychology, Faculty of Psychology, National University of Córdoba, Córdoba, Argentina
** Prof. León S. Morra Sanitarium, Córdoba, Argentina
FSG was supported by the Doctoral Scholarship Type II 2013 of the Secretary of Science and Technology (SECyT), Universidad Nacional de Córdoba (UNC).
ABSTRACT
Background and Objectives: There are many associations between psychotic symptoms and performance in Verbal Fluency (VF) tasks. However, most of these are found are with negative symptoms. In this study we examined the relationship between the performance in four VF tasks and the severity of both positive and negative symptoms.
Methods: To compare performance in different VF tasks, two groups of participants were matched for age, sex and educational level, a Healthy Control Group (N = 83) and a Chronic Schizophrenia Group (N = 83). We examined the correlation between cognitive performance in these verbal tests and the severity of psychotic symptoms in the group of patients.
Results: The results show that the performance of patients with chronic schizophrenia in VF tests is significantly lower than for healthy individuals. The analysis of correlations between tasks showed a significant correlation between the severity of negative symptoms and poor performance in VF tasks. Another interesting result was the association between the severity of formal thought disorder and poor performance in semantic VF. A particularly striking result was the correlation between the severity of positive symptoms and the number of errors in VF tasks in the patient group.
Conclusions: These results have provided evidence for some of the proposed hypotheses and are in accordance with previous investigations. The correlations between the positive symptoms and the number of errors in the different VF tasks have not been previously reported. It is important to note that most of these correlations are between the severity of positive symptoms and intrusion errors.
Key words: Chronic Schizophrenia; Verbal Fluency; Negative Symptoms; Errors Task; Formal Thought Disorder.
Introduction
There are many associations between psychotic symptoms and the performance in verbal fluency (VF) tests1-7. However, most of these associations are with negative symptoms rather than positive ones. Only one study, carried out by Kerns, Berenbaum, Barch, Banich & Stolar5, found a relationship between the presence and severity of hallucinations and the production of contextually related words.
Studies conducted by Allen, Liddle & Frith8, Joyce, et al.4 and Docherty, et al.3 suggest that alogia and formal thought disorder (FTD) are associated with different patterns of VF task deficiencies. More specifically, the work by Docherty, Berenbaum & Kerns3 shows that alogia is associated with poor controlled retrieval, finding increased response latency between each word on the semantic verbal fluency (SVF). However, alogia was not found to be correlated with the performance in the VF task, showing a deficiency in semantic memory and contextual processing. This led the authors to conclude that decreased language generation and syntactic complexity in patients with schizophrenia are associated with problems in the use of controlled retrieval mechanisms, connected to access with intact representations of semantic memory.
On the other hand, FTD was associated with VF deficiency, showing poor contextual processing, as this symptom was associated with fewer semantically related words in the phonemic verbal fluency test (PVF)3. The same study showed that there is no relationship between FTD and other indices involving semantic memory deficiencies like response latency in the SVF, or a low performance in this task compared to the PVF test. Therefore the results would indicate that language disorder in schizophrenia appears to be associated with problems in the use of contextual processing to guide and monitor language3.
The aforementioned study by Kerns, et al.5 showed that FTD is related to the production of non related words (few contextual words), coinciding with the recent results of Docherty, et al3. However, Kerns interprets this data as a disturbance in the organization of semantic memory. Contextually related words would be a more sensitive indicator of semantic memory problems; in turn, categorical relationships would be less affected by semantic memory problems than contextual relations.
The relationship between FTD and VF seem more evident in SVF tasks than in PVF tasks. These results suggest that patients with FTD have semantic processing deficits5. Alterations in semantic memory organization and loss of semantic information appear to reflect anatomical changes in the left temporal lobe or problems in the modulation of this brain area by the frontal lobe.
Another line of investigation has been developed based on the study of the semantic structure of schizophrenic patients using VF tests, also been related with the psychotic symptoms. One study showed that patients with alogia lack a meaningful dimension in the organization of the semantic structure, suggesting that semantic disorganization underlies alogia in schizophrenic patients7. Semantic memory degradation might precede the emergence of psychotic symptoms7,9.
The present investigation studies a possible relation between the performance in four VF tasks and the severity of psychotic symptoms, both positive and negative. Unlike other studies, we applied VF tasks using a single given category determined by the examiner, and combined category tests in which the participant can change freely between categories, previously determined by the examiner, during the test. Furthermore, we analyze the relation between the performance in the different VF tasks and each of the psychotic symptoms included in the Scale for Assessment of Positive Symptoms (SAPS) and the Scale for Assessment of Negative Symptoms (SANS). Our main hypothesis is the existence of a relation between a low performance in PVF tasks and the severity of negative symptoms, due to the executive demands that these tasks entail and the well established connection between these functions and negative symptoms.
Materials and methods
Subjects
This study comprised two groups of participants: a Healthy Control Group and a Chronic Schizophrenia Group. The Healthy Control Group included 83 healthy participants (preserved cognitive functioning, no record of cognitive complaints and overall good physical health) of both sexes between 21 and 65 years old of the city of Córdoba, Argentina. Individuals with the following antecedents were excluded: cerebrovascular accident (CVA), encephalic cranial trauma, episodes of coma, epilepsy, loss of consciousness for more than 20 minutes, cardiomyopathy, nephropathy, hepatic encephalopathy, thyroid problems, diabetes, chronic headaches, hypertension, recurrent sleep alterations, diagnosed psychiatric alterations and drug use.
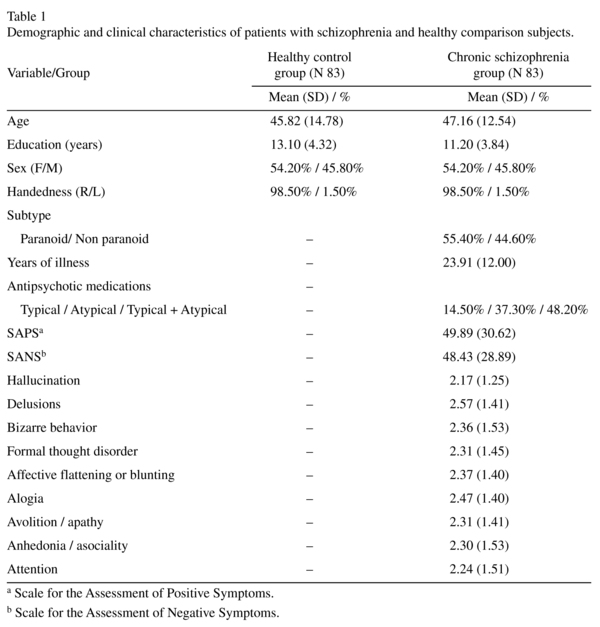
The Chronic Schizophrenia Group included 83 patients attending services for chronic and acute hospitalization and day hospital service at the following mental health institutions in the city of Córdoba, Argentina: Clínica Integral de Psiquiatría "San Nicolás" and Sanatorio "Profesor León Morra". All the participants in this group met the diagnostic criteria for schizophrenic disorder proposed by the DSM IV10. Patients participating in this study were stably medicated at the time of assessment for at least one month before the tests. Both groups were matched for age, sex and level of education. Table 1 shows the descriptive results of sociodemographic data for both groups and the clinical data for the Chronic Schizophrenia Group.
Verbal Fluency Test
Semantic Verbal Fluency Test: Two types of tests were selected: a single category test using the category "Animals" and a combined category test using "Fruits or Animals". In the first test, participants had to name as many animals as possible during a minute without repeating them. In the combined category fluency test, participants had to name as many fruits and animals as they could during a minute without repeating them.
Phonological Verbal Fluency Test: The letter "P" was chosen for the phonetic verbal fluency test, where participants had to name as many words as possible beginning with the letter "P" in one minute, but could not repeat words or use their own name. The other phonetic test was similar using letters "A" or "F", the participants could switch freely between letters but could not repeat words or use names, places nor countries.
Assessment of symptoms
Spanish version (available on demand from Dr. Nancy Andreasen) for the Scale for the Assessment of Positive Symptoms -SAPS-11. The SAPS was used to assess the state of positive psychotic symptoms of the participants as it is specifically designed for symptoms present in schizophrenia11. This assessment scale evaluates symptoms over a period of time, generally considering the state of the patient a month prior to the time of evaluation. A standard interview was used in this evaluation.
Spanish version (available on demand from Dr. Nancy Andreasen) for the Scale for the Assessment of Negative Symptoms -SANS-12. The SANS was used for evaluating the negative psychotic symptoms due to its specificity in assessing psychotic symptoms present in schizophrenia12. This scale uses the same aforementioned specifications.
Procedure and selection of participants
The study was carried out in two stages. The first stage consisted in the selection and evaluation of participants with chronic schizophrenia, and the second stage was the selection and evaluation of the healthy control group. This approach was used to match the participants by age, sex and level of education. The study involved two sessions for the control group and three sessions for the group of patients. This difference was due to the particular requirements that the group of patients demanded in their selection and evaluation.
The group of healthy individuals were interviewed in the first session to learn about their sociodemographic and clinical background to select and possible participants. After this interview they were explained the objectives of the study and the scientific use of the results of the study, making clear that their identity would be kept secret and that all the data collected would be referred to a number and a letter. They were also informed that their participation in this study involved a brief clinical and cognitive evaluation regarding their cognitive function, that the tests were destined for people of their age and condition and entailed no risk or discomfort. The cognitive evaluation was then performed in a subsequent session of 45 minutes, where two professionals specialized in neuropsychology applied to psychiatric disorders carried out the four tests of VF with a 10 minute interval between each test. The VF performance was recorded with the consent of the participants for a better assessment.
The patient group had a similar procedure. Followed by a preselecting conducted cooperatively with professionals who care for patients was performed the Structured Clinical Interview for DSM- IV Disorders. A meeting was held with the participants to inform them of the objectives of the study and the scientific use of the results of the study, making clear that their identity would be kept secret and that all the data collected would be referred to a number and a letter. They were also informed that their participation in this study involved a brief clinical and cognitive evaluation regarding their cognitive function, that the tests were destined for people of their age and condition and entailed no risk or discomfort. The participants that accepted to take part in the study were then evaluated to determine the severity of their symptoms using the Positive and Negative Syndrome Scale11,12. The cognitive tests were carried out in a later session using the same procedure described for the healthy group. At the same time, and with due authorisation, the clinical histories of the patients were examined to gather and corroborate their socio-demographic (i.e. level of education) and clinical data (beginning of the illness, years of illness, current medication).
Statistical Analyses
Descriptive statistics were calculated. A two-tailed t-test was used to compare patients and controls. A Pearson correlation analysis was used to analyze relationships between the severity of psychotic symptoms and performance in verbal fluency tasks and to examine possible relationships between doses of medication administered and the performance in verbal fluency tests. Results were considered significant at p < 0.05. All statistical tests were carried out using PAWS statistics 18.
Results
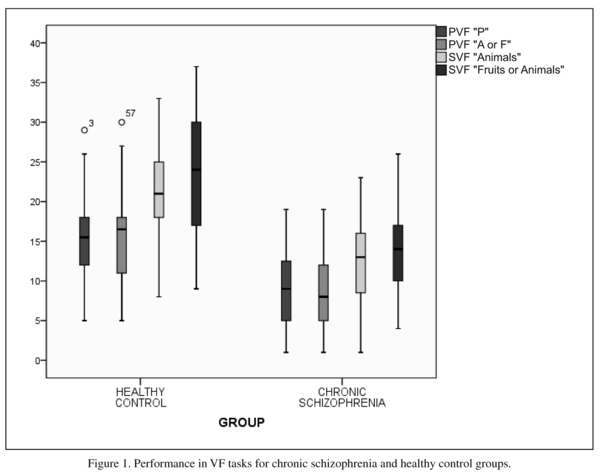
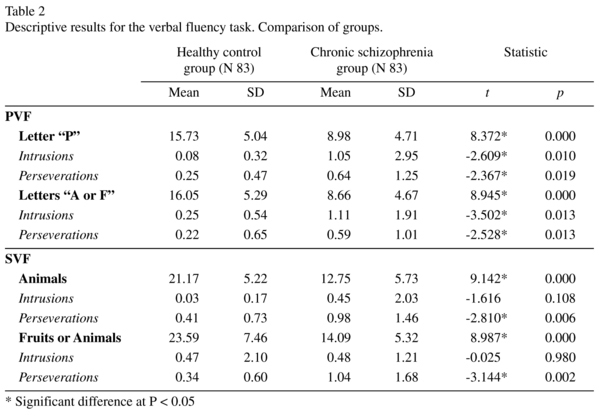
The descriptive results show that schizophrenic patients group produces significantly fewer words in the four VF tasks compared to the healthy control group (Figure 1 and Table 2). As shown in Table 2, independent sample t-tests revealed that the control healthy and chronic schizophrenia groups differ significantly in the performance in VF task. The performance of both groups was more limited in the PVF task. Statistically significant differences for the number of errors in VF tasks were also evident, except for intrusions in both SVF task (Table 2).
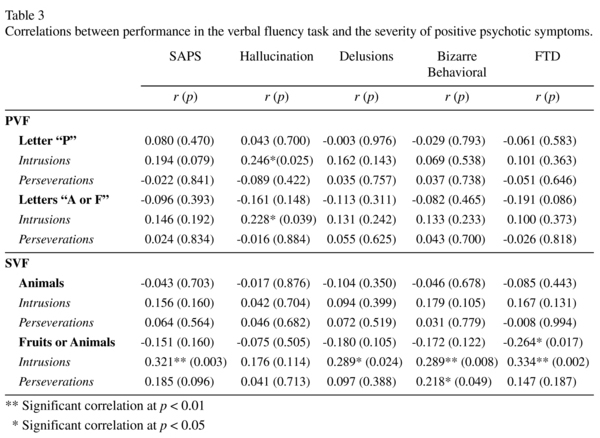
One of the clinical psychiatric variables considered in this study was both positive and negative symptoms. Correlation analysis evidenced different associations between symptoms and performance in VF (Tables 3 and 4). Overall the results show a correlation between low performance in VF and the severity of negative symptoms. Correlation analyses between the different negative symptoms and performance in the VF tasks show that the severity of affective flattening or blunting is significantly correlated with reduced production of words in two of the PVF tests and with SVF "Animals". The abulia-apathy symptomatic pair is correlated with low performance in the four verbal fluency tests. Other negatives symptoms were significantly correlated with the performance in the tests, such as attention impairment during the interviews and PVF task, and anhedonia-unsociability with the SVF "Animals" (see coefficients in Table 4). Among the positive symptoms, the only one that correlated significantly with performance in VF is FTD, the severity of which is related to low performance in alternating SVF task (r = -0.264; p = 0.017).
Positive symptoms are correlated with the generation of errors in the tasks. For example, the general assessment of the severity of positive symptoms is strongly correlated with the production of words that do not belong to the "Fruit or Animal" categories assigned in the SVF task. Also, the severity of hallucinations is significantly correlated with the generation of intrusive words in the two PVF. Delusions and bizarre behavior were found correlated with the presence of intrusions in alternating SVF "Fruits or Animals" (r = 0.249, p = 0.024 and r = 0.289, p = 0.008 respectively). The latter also was related with the amount of perseverations produced in the same task (r = 0.218; p = 0.049). The number of perseverations in the alternating PVF task was correlated with the global assessment of the severity of negative symptoms and with the acuteness of affective flattening or blunting.
Discussion
This study analyzed and compared the performance of four VF tasks, phonological and semantic (the only option and alternating). Our results are consistent with investigations suggesting that a severe impairment in word production in patients with chronic schizophrenia. The variables that provided most data in this study were the clinical psychiatric variables. These results have provided evidence for some of the proposed hypotheses and are in accordance with previous investigations. Such is the case of the associations found between performance in the four VF tests, semantic and phonemic, and the severity of negative symptoms5,13,14.
The theoretical discussions regarding this repeated finding regard the great demand this type of cognitive task has on the executive function of the prefrontal brain, evidencing a specific relation between executive dysfunction and negative symptoms. Or are cognitive deficits correlated in general with negative symptoms more that positive symptoms?15. Our results may contribute to the hypothesis of a specific executive dysfunction, specifically in the PVF that have higher coefficients of correlation more than the SVF.
This discussion between executive specificity or a general cognitive deterioration regarding negative symptoms strongly disputes the negative symptom concept and to what degree they don't include the widely established cognitive alterations of schizophrenia. Are the significant correlations found between the severity of different negative symptoms (blunted affect, abulia and apathy, anhedonia and unsociability, and attention deficits) and low performance in VF evidence of the relations between a specific executive dysfunction in schizophrenia and its behavioral expression through negative symptoms? Is it possible to build an explanatory model based on levels of executive dysfunction that are translated to the behavioral level in observable behavioral variables affecting different social and functional outcomes of the patient?
The evidence established by most of the current studies supports this conceptual controversy regarding psychotic symptoms, showing that neurocognitive functioning predicts the daily performance of patients more strongly than psychotic symptoms16-18. Authors like Brazo, et al.19 or Villalta Gil, et al.20 argue that patients with greater neurocognitive alterations have more severe negative symptoms, generating a strong interaction between neurocognition and schizophrenia symptoms21.
A noticeable fact is that in this association between performance in VF and most negative symptoms, there is no relation regarding the negative symptom which in itself would imply a specific language alteration, namely alogia. These results are consistent with the evidence reported by Docherty, et al.3 showing that alogia was not related with performance in the VF they used. In agreement with previous reports, the severity of FTD was correlated with low performance in one of the semantic tests. As established by Kerns et al.5 these results allow to infer that patients with formal thought disorder will have difficulties with semantic processing.
Another interesting result was the correlations found between the positive symptoms assessed and the large number of errors in the different VF tasks. To our knowledge this result has not been previously reported. It is important to note that most of these correlations are between the severity of positive symptoms and intrusion errors, where patients produce words that do not abide with the rules established by the examiner. For example, in the SVF patients retrieved items belonging to other semantic categories. Future studies should further examine these results, paying specific attention to the effect of hallucinations on the production of errors in phonetic tests, which apparently demand intense executive function.
Role of funding source
SECyT and UNC have not participated in study design, collection, analysis and interpretation of data, writing of the report, or the decision to submit the paper for publication.
References
1. Basso MR, Nasrallah HA, Olson SC, Bornstein RA. Neuropsychological correlates of negative, disorganized and psychotic symptoms in schizophrenia. Schizophr Res. 1998; 31 (2-3): 99-111. [ Links ]
2. Brébion G, Villalta-Gil V, Autonell J, Cervilla J, Dolz M, Foix A, et al. Cognitive correlates of verbal memory and verbal fluency in schizophrenia, and differential effects of various clinical symptoms between male and female patients. Schizophr Res. 2013; 147(1): 81-85. [ Links ]
3. Docherty AR, Berenbaum H, Kerns JG. Alogia and formal thought disorder: Differential patterns of verbal fluency task performance. J Psychiatr Res. 2011; 45: 1352-1357. [ Links ]
4. Joyce EM, Collinson SL, Crichton P. Verbal fluency in schizophrenia: Relationship with executive function, semantic memory and clinical alogia. Psychol Med. 1996; 26: 39-49. [ Links ]
5. Kerns JG, Berenbaum H, Barch DM, Banich MT, Stolar N. Word production in schizophrenia and its relationship to positive symptoms. Psychiatry Res. 1999; 87: 29-37. [ Links ]
6. O'Leary DS, Flaum M, Kesler ML, Flashman LA, Arndt S, Andreasen NC. Cognitive Correlates of the Negative, Disorganized, and Psychotic Symptom Dimensions of Schizophrenia. J Neuropsychiatry Clin Neurosci. 2000; 12: 4-15. [ Links ]
7. Sumiyoshi C, Sumiyoshi T, Nohara S, Yamashita I, Matsui M, Karachi M, et al. Disorganization of semantic memory underlies alogia in schizophrenia: An analysis of verbal fluency performance in Japanese subjects. Schizophr Res. 2005; 74 (1): 91-100. [ Links ]
8. Allen HA, Liddle PF, Frith CD. Negative features, retrieval processes, and verbal fluency inschizophrenia. Br J Psychiatry. 1993; 163: 769-775. [ Links ]
9. Phillips T, James A, Crow T, Collinson S. Semantic fluency is impaired but phonemic and design fluency are preserved in early - onset schizophrenia. Schizophr Res. 2004; 70, 215-222. [ Links ]
10. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association; 1994. [ Links ]
11. Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA: The University of Iowa; 1984. [ Links ]
12. Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS). Iowa City, Iowa: The University of Iowa; 1983. [ Links ]
13. Nuechterlein KH, Edell WS, Norris M, Dawson ME. Attentional vulnerability indicators, thought disorder, and negative symptoms. Schizophr Bull. 1986; 12: 408-426. [ Links ]
14. Howanitz E, Cicalese C, Harvey PD. Verbal fluency and psychiatric symptoms in geriatric schizophrenia. Schizophr Res. 2000; 42 (3): 167-169. [ Links ]
15. Henry JD, Crawford JR. A met-analytic review of verbal fluency deficits in schizophrenia relative to other neurocognitive deficits. Cogn Neuropsychiatry. 2005; 10: 1-33. [ Links ]
16. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996; 153: 321-330. [ Links ]
17. Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the "right stuff"? Schizophr Bull. 2000; 26 (1): 119-136. [ Links ]
18. Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: A meta-analysis. Schizophr Res. 2009; 113 (2-3): 189-199. [ Links ]
19. Brazo P, Delamillieure P, Morello R, Halbecq I, Marié RM, Dollfus S. Impairments of executive/attentional functions in schizophrenia with primary and secondary negative symptoms. Psychiatry Res. 2005; 133 (1): 45-55. [ Links ]
20. Villalta Gil V, Vilaplana M, Ochoa S, Haro JM, Dolz M, Usall J, et al. Neurocognitive performance and negative symptoms: are they equal in explaining disability in schizophrenia outpatients? Schizophr Res. 2006; 87 (1-3): 246-253. [ Links ]
21. Harvey PD, Green MF, Bowie C, Loebel A. The dimensions of clinical and cognitive change in schizophrenia: Evidence for independence of improvements. Psychopharmacology. 2006; 187 (3): 356-363. [ Links ]
![]() Correspondence:
Correspondence:
Flavia S. Galaverna
Laboratory of Experimental Psychology
Faculty of Psychology
National University of Córdoba
Enfermera Gordillo esquina Enrique Barros
Ciudad Universitaria, CP X5000GYA
Córdoba, Argentina
Tel.:+ 54 351 4344984
Fax: + 54 351 4334064
E-mail: fgalaverna@psyche.unc.edu.ar
Received: 24 January 2014
Revised: 1 July 2014
Accepted: 7 July 2014