Introduction
Borderline personality disorder (BPD) is a severe mental health condition observed in clinical and non-clinical populations, with a percentage rate of 1.4 to 5.9% and 2 to 3% respectively (Chapman, 2019; Gunderson et al., 2018; Trull et al., 2018).
It is characterized by emotional dysregulation, psychological instability, impulsiveness and relational difficulties, among others (Chapman, 2019; Luyten et al., 2019). People with BPD tend to perceive distrust towards others, facing the possibility of an imminent abandonment or rejection (Perrotta, 2020). These attributions lead to disruptive behaviors against significant others through social conflicts and interpersonal violent behaviors like intimate partner violence (IPV) (Látalová & Praško, 2010).
Several studies have pointed out the association between BPD and intimate partner violence, whether in physical, sexual or psychological violence (e.g. Gonzalez et al., 2016; Jackson et al., 2015; Sijtsema et al., 2014; Stepp et al., 2012; Weinstein et al., 2012). In fact, BPD seems to be the more likely personality disorder to perpetrate partner-violence both in males and females, in a more frequent and several ways (Gonzalez et al., 2016).
Taking these findings into account, this review summarizes empirical studies published between 2017 and 2021 that relate borderline personality disorder with intimate partner violence. Increasing our knowledge in this field, may lead us to improve clinical practice and to promote future research.
Method
This systematic review was developed based on the Preferred Reporting Items for Systematic Review -PRISMA- (Page et al, 2021b). The databases Web of Science, Scopus and ProQuest was searched for the terms ("dating violence" OR "partner violence" OR "interpersonal violence" OR "intimate partner violence" OR battering OR "intimate violence" OR "domestic violence" OR "dating abuse" OR "partner abuse" OR "interpersonal abuse" OR "intimate partner abuse" OR "intimate abuse" OR "domestic abuse" OR "dating assault" OR "interpersonal assault" OR "intimate partner assault" OR "domestic assault") AND ("borderline personality" OR "borderline traits" OR "borderline features" OR "borderline symptoms" OR "borderline disorder") according with Jackson et al. (2015).
The research included studies made in English or Spanish between 2017 and December 1st, 2021. References of identified articles were searched for additional relevant articles. Studies with adult population with borderline disorder, traits of borderline personality symptoms who was in a violent relationship which was cross sectional, longitudinal, experimental, correlational, exploratory or systematic review was included, while Chapters book, Doctoral Thesis, studies with n = 1, communications in Congress, manuscripts without blind double review were excluded in order to reduce the risk of bias.
Elimination of duplicate articles was made using Rayyan, a specific digital application for systematic review (Ouzzani et al., 2016). Articles selected were reviewed for 2 authors and relevant information was extracted independently, with discrepancies resolved for discussion.
Results
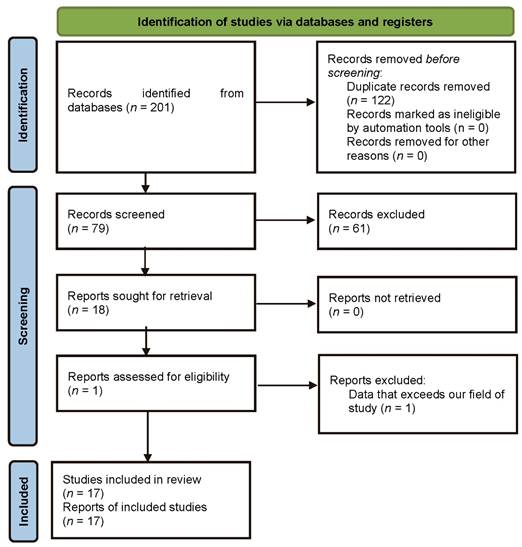
In the first instance, 201 studies were selected from databases according to inclusion and exclusion criteria. 122 duplicate articles were mechanically deleted through Rayyan (Ouzzani et al., 2016), remaining 79 studies. Subsequently, 61 articles were manually excluded due to deviating from the main aim of this systematic review, having 17 finally included for a more extensive analysis.
Table 1 summarizes included studies with number of participants (see Figure 1), gender, if perpetrator of victim in the relationship, study design and quality, measures and questionnaires used and main results. The quality of the articles was assessed with Quality Rating Scheme for Studies and Other Evidence (Centre for Evidence Based Medicine, 2009).
Table 1. Study Characteristics
| Study | Sample | Design | Evidence Level | Main results |
|---|---|---|---|---|
|
USA |
135 adult couples. Mean age: 32.02 in males and 29.99 in females |
Cross-sectional correlational exploratory design | 4 | There is a negative correlation between borderline personality traits and psychopathic features. When predicting heart rate reactivity, there is a significant interaction between cognitive empathy and borderline personality traits, and between affective empathy and psychopathic features. Skin conductance does not seem to have any relevant interaction with these personality traits. |
|
USA |
218 university students (48.2% males, 51.8% females) in a relationship. Mean age: 22.98. |
Cross-sectional correlational exploratory design | 4 | BPD features are associated with rejection sensitivity and IPV. It has been seen that anger mediates the relationship between BPD traits and psychological aggression. There was a significant association between BPD features and later anger in ambiguous situations than in critical ones. |
|
USA |
135 adults. Mean age: 32 years in males, 29,9 in females. |
Cross-sectional correlational exploratory design | 4 |
Borderline personality traits and alcohol problems are associated in order to predict frequency of IPV. The same results are observed with antisocial personality features. However, drug problems are not associated with any of the mentioned traits when predicting frequency of IPV. |
|
USA |
79 adult couples with male-to-female IPV. Mean age: 29.9 |
Cross-sectional correlational exploratory design | 4 | BPD features are associated with more accuracy in recognizing fear and surprise, while psychopathic traits are related to a lower accuracy. Higher skin conductance when viewing facial expressions and BPD traits are associated. Perpetrators males with psychopathic traits present a lower skin conductance and a lower sensitivity towards emotional distress expressions by their partners. |
|
USA |
211 adult women IPV victims with PTSD symptoms. Mean age: 37.81 years |
Cross-sectional correlational exploratory design | 4 | Significant interaction between BPD traits and PTSD symptoms derived from victimization is observed. There are no significant associations between borderline features and childhood abuse. |
|
Australia |
Adults in a relationship (147 females and 53 males) with a mean age of 22,28 | Cross-sectional correlational exploratory design | 4 | Anxious and avoidant attachment, BPD traits and psychopathic features are positively associated with perpetration in psychological and online IPV. Anxious attachment is indirectly associated with perpetration via high BPD and psychopathic traits, while avoidance attachment presents a similar association but only with psychopathic traits. |
|
Spain |
1190 adult couples Mean age: 46.5 in males and 44.4 in females |
Cross-sectional correlational design | 4 |
Females tend to express both perpetration and victimization. In males, there is a significant association between IPV and BPD and psychopathic features. In the case of female perpetrators, alcohol consumption and quality relationship are associated with IPV. A significant correlation between male perpetration and female victimization is observed. |
|
Netherlands |
633 adult people (29.2% males, 70.8% females) | Cross-sectional correlational exploratory design | 4 | Child sexual abuse and adult sexual IPV are significantly associated. The severity of the child sexual abuse, BPD features, dissociative symptoms and emotional dysregulation are important predictors for adult sexual IPV.Dissociation and emotional dysregulation mediate the relationship between both child sexual abuse and adult sexual IPV. |
|
Netherlands |
703 adults (25% males, 75% females) with a mean age of 28.49 | Cross-sectional correlational exploratory design | 4 | There is a significant association between childhood maltreatment and a subsequent IPV perpetration or victimization during adulthood. This interaction is mediated by borderline personality traits, which are predicted by the childhood maltreatment itself. Coping strategies are related to BPD features, influencing in both perpetration and victimization. |
|
USA |
127 adult men in a community-based IPV intervention program Mean age: 35.7 Two separated cohorts (1999-2001 and 2009-2011) |
Cross-sectional design | 4 |
The 89.8% of participants experienced negative reactions following IPV, while 32,7 experienced positive reactions and the 67.5 had conciliatory behaviors. Positive reactions following IPV were associated with positive result expectancies of violence, higher frequency of abuse and antisocial traits. Negative reactions following IPV were associated with higher motivation to change, higher frequency of abuse perpetration and borderline traits, and were inversely linked to psychopathic traits. Conciliatory behaviors were associated with motivation to change, borderline traits and lower levels of psychopathic traits. |
|
USA, UK, New Zealand, Poland and Finland |
Systematic Review | 1 | Risk factors of IPV perpetration in women were not found. However, there were an association between perpetrate IPV and child abuse, borderline traits, substance use (specially alcohol), experiencing trauma and attachment issues. | |
|
Portugal |
19 battered women at a special protection shelter house for IPV victims | Experimental, longitudinal design | 3 | Compared to the placebo group, the intervention group presented a positive effect size in depression, borderline and PTSD (Post Traumatic Stress Disorder), as well as in some CPTSD (Complex Post Traumatic Stress Disorder) dimensions when analyzing baseline-follow-up. There was also a negative effect size in the CPTSD total. |
|
New Zealand |
250 adults with a mean age of 30.25 | Cross-sectional correlational design | 4 |
Both the “traditional” and the AMPD (DSM 5 Alternative Model of Personality Disorders) operationalization of BPD were equally associated with IPV perpetration. The AMPD traits of hostility, suspiciousness and risk taking were robustly associated with IPV perpetration for the total sample; negative affectivity trait facets were related to IPV perpetration for men. |
|
New Zealand |
531 male domestic violence offenders who were court-mandated to undergo treatment. Mean age: 33.62 |
Experimental, longitudinal design | 3 |
The IPV perpetrators with BPD symptomatology were more likely to fail to complete the intervention program and were at higher risk to re-offend during one-year follow-up. On the other hand, both traditional BPD and AMPD BPD relevant traits had a similar association with IPV self-reported variables, IPV intervention results and recidivism. |
|
Iran and Germany |
45 women victims of IPV with a PTSD diagnosis | Experimental, longitudinal design | 3 | Compared to TAU (Treatment-as usual) group, NET (Narrative Exposure Therapy) participants present a significantly greater symptoms reduction in depression, PTSD and perceived stress at both, three and six months’ follow-ups. Enhancement of daily functioning and reduction of borderline symptoms and IPV experiences at both follow-ups were greatly but not significantly different between the two treatment groups. |
|
United States |
193 males with a mean age of 19.69 | Cross-sectional correlational design | 4 |
BPD was associated with violent behaviors and IPV; and negative urgency (impulsive behavior in response to intense, negative emotions) was only associated with IPV. No indirect paths from BPD outcome were demonstrated via any other factors of impulsivity; despite this, sensation seeking was an independent predictor of general violence. |
|
United States |
139 partner violent men | Cross-sectional design | 3 |
Compared to antisocial personality disorder (ASPD), men with BPD present longer periods of anger and lower skin conductance reactivity. In contrast to men with no diagnosis, those with BPD present less frequent distress and longer periods of anger, while those with ASPD exhibit greater heart rate reactivity and shorter periods of anger. In men with ASPD, psychological aggression used to be preceded by partner positive or neutral affect. |
Perpetration
Borderline traits are broadly associated to all forms of IPV, physical, psychological and sexual perpetration and also with its frequency (Armenti et al., 2018; Armenti & Babcock, 2021; Munro & Shellbom, 2020; Mackay et al., 2018; Jose et al., 2021), being a risk factor especially for women perpetration (Mackay et al., 2018).
Empathy can play an important role in this relationship. IPV perpetration in people with BPD has been associated with a higher cognitive empathy compared with controls, maybe due to hypermentalizing (over-attributing intentions and ideas to other people) which can lead to interpersonal confusions (Armenti & Babcock, 2018). Similarly, Babcock and Michonski (2019) point out that sensitivity to facial affect in other people can mediate the relation between BPD and IPV perpetration, presenting higher physiological reactivity than controls before facial expressions of different emotions and precisely identifying the emotions of surprise and fear.
Regarding antecedents and consequences, it is usual to feel anger before aggression and this is preceded by their partner´s distress 43% of the times (Trahan & Babcock, 2019); as consequence, in contrast with psychopathic traits, BP features are associated with more frequent abuse perpetration, negative reactions (e.g. feeling ashamed), greater motivation to change and conciliatory behaviors (such as buying flowers to the partner).
In this line, trait anger is an important mediator between BPD and aggression, being activated by environmental factors as an ambiguous rejection. A possible explanation could be that those who have perceived rejection during childhood tend to expect malicious rejection when ambiguous behaviors of their intimate partner, and those with BPD traits present higher levels of rejection sensitivity (Armenti & Babcock, 2021). In this regard, people with an anxious attachment may tend to act aggressively toward their partners in conflict situations, being a link between BPD and psychological abuse (Bui & Pasalich, 2021).
Some BPD traits such as interpersonal disturbances and affective instability have a crucial role in IPV perpetration (Krause-Utz et al., 2021b). An indirect effect of childhood trauma severity via BPD features on IPV perpetration has been identified, and also a link between maladaptive coping and BPD features. Thereby, interpersonal disturbances, affective instability with or without self-harming, impulsivity and identity disturbance are relevant factors for IPV perpetration (Krause-Utz et al., 2021b). Peters et al. (2017) suggest that negative urgency (impulsive behavior in response to negative and intense emotions) has also an indirect effect in the relationship between BPD and IPV.
IPV perpetration is also related to some borderline facets such as risk taking and suspiciousness, which are associated with sexual IPV perpetration in both genders; while anxiousness, separation insecurity, emotional lability, impulsivity and depression are associated only for men. Also, higher scores in BPD for men are related to sexual coercion, psychological aggression and IPV variety during the last year (Peters et al., 2017).
Noteworthy, hostility and anger are strongly associated with physical and psychological IPV and predicts its frequency (Armenti & Babcock, 2021; Munro & Sellbom, 2020). In fact, compared with no diagnosis and antisocial personality, BPD men who perpetrate IPV exhibit longer periods of anger and lower levels of distress and psychophysiological reactivity. BPD and antisocial present the same IPV injuries severity, which is higher than in those with no diagnosis (Trahan & Babcock, 2019).
Regarding gender differences, females IPV perpetrators are more likely to be assessed for BPD than any other disorder (Mackay et al., 2018). Besides, there are no differences between male and female perpetrators treatment or hospitalization, despite females are more likely to attempt suicide and been prescribed psychopharmacological medication.
Also, female perpetrators scored higher than controls in borderline and other cluster B personality disorders, and perpetration is associated with alcohol consumption and relationship quality. BP features are associated with IPV perpetration in males, while women tend to take both perpetration and victimization roles (Jose et al., 2021).
Regarding substance abuse, it has been found a strong association between alcohol consumption and IPV in individuals with BP traits (Armenti et al., 2018; Jose et al., 2021; Mackay et al., 2018) increasing physical violence frequency in comparison to people with a lower consumption (Armenti et al., 2018), although there is no consensus about if this occurs with other substances consumption too (Armenti et al., 2018; Mackay et al., 2018).
Referred to intervention, people with borderline features have an increased risk of not complete IPV treatment, due to a lower participation rating, lower confidence in violence inhibition, and higher blame externalization, being also more likely to reoffend in one year follow up. IPV recidivism, blame externalization, new arrest after treatment, IPV control tactics and program dismissal can be predicted according to some dimensions of the BPD such as negative affectivity; for this reason, it´s important to take borderline features into account for a better design of intervention programs (Munro & Sellbom, 2021).
Along the same lines, it is important to reduce alcohol consumption for reducing IPV in individuals with borderline features (Armenti & Babcock, 2018). In order to predict adherence and treatment outcome, some variables such as conciliatory behaviors and negative reactions after IPV perpetration must be considered, since they are associated with higher readiness to change in people with borderline features (LaMotte et al., 2019).
Victimization
According to Beck et al. (2019), significant associations between BP traits and IPV-related post-traumatic stress disorder (PTSD) symptoms have been observed, especially in re-experiencing, avoidance and hyperarousal symptoms. For these authors, a history of childhood abuse (CA) does not modulate the association between borderline traits and IPV-related PTSD symptoms.
Nevertheless, according to Krause-Utz et al. (2021b) childhood maltreatment is associated with IPV and borderline traits during adulthood. Childhood maltreatment predicts victimization as perpetration of IPV, and borderline traits mediates the effect of this relation. So, having those personality traits correlates with childhood maltreatment and is considered a risk factor for been victim or perpetrator of IPV. Specifically, identity and interpersonal disturbances mediate the effect of childhood maltreatment in IPV adult victims. In this way, fear of abandonment or loneliness, as well as an unstable self-image are considered significant risk factors of victimization.
Considering Krause-Utz et al. (2021b) sample, females were more likely to have a clinical diagnosis and a history of psychotherapy, as well as higher BPD traits, anxious attachment, maladaptive coping strategies and less perceived social support than men. Besides, a history of moderate to extreme abuse and severe childhood trauma was more frequent in females too. 82.5% of males and females reported reciprocal IPV violence, experiencing and perpetrating it, and there were no gender differences about IPV perpetration or victimization associated with borderline features.
Child sexual abuse (CSA), as well as dissociation, maladaptive emotional regulation and BPD features are significant risk factors for sexual IPV, which is a form of revictimization. Maladaptive emotional regulation and dissociation mediates the association between CSA and sexual IPV, while dissociation explained the effect of CSA through BPD features, being a risk factor of sexual IPV (Krause-Utz et al., 2021a).
Finally, psychological interventions could be beneficial in this field for the aftermath in victims of IPV daily functioning. A reduction of depression, complex posttraumatic stress disorder (CPTSD), posttraumatic stress disorder (PTSD) and borderline dimensions has been seen after a cognitive-narrative intervention in IPV victims (Moreira et al., 2020). Orang et al. (2018) compared group narrative exposure therapy and counseling (treatment as usual, TAU) in a sample of IPV female victims. PTSD symptoms, perceived stress and depression decreased after 3 to 6 months in those participants of the group narrative exposure therapy. In contrast, enhancement of daily functioning and a reduction of borderline features and IPV experiences were observed in both groups, pointing out the importance of being in treatment even during the situation of violence so it can prevent it.
Discussion
The aim of this systematic review was to analyze empirical studies published between 2017 and 2021 that relate BPD with IPV. No previous systematic reviews about this relation including both perpetrators and victims was found, therefore this topic deserves special interest due to its implications for clinical guidelines.
BP traits are associated with both IPV perpetration and victimization (Jose et al., 2021; Krause-Utz et al., 2021b). Nevertheless, there are more studies that relate BPD with IPV perpetration (e.g. Armenti & Babcock, 2018; Jose et al., 2021; Mackay et al., 2018) than those that associate BPD with IPV victimization (Beck et al., 2019; Krause-Utz et al., 2021a).
It is important to take into account that almost a half (N=7) of the selected studies are about borderline personality males and their tendency to perpetrate IPV (e.g. LaMotte et al., 2019; Peters et al., 2017). These findings are relevant considering the higher existing prevalence of BPD among women. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), females represent 75% of individuals with BPD diagnosis (APA, 2013).
In the general population, 85% of IPV perpetration is caused by male to female partners (Roark, 2010), although it can be seen in both genders (Gonzalez et al., 2016; Jackson et al., 2015). As Jose et al. (2021) pointed out, females with BP traits could present both perpetration and victimization roles, although there is a tendency to perpetrate in males and to suffer IPV in females. In contrast with this, we found that almost a third of the studies (N=5) presented an equal or major percentage of women compared to men who perpetrated violence. Besides, the only systematic review included was focused on women with BPD diagnosis who perpetrated violence. In this line, the systematic review of Jackson et al. (2015) found that females with borderline traits were more likely to perpetrate IPV, as well as men with the same personality features. On the other hand, Maneta et al. (2013) found that BP traits are associated only with victimization in females, while in the case of males those features are associated with both perpetration and victimization.
Substance abuse is associated with BPD and IPV perpetration, especially alcohol consumption (Armenti et al., 2018; Jose et al., 2021; Mackay et al., 2018). This consumption has frequently been associated with BPD traits (Chapman, 2019) as well as with IPV perpetration (Jackson et al., 2015; Stewart & Vigod, 2017). The results obtained in this review are in line with those by Stuart et al. (2006) that relate female IPV perpetrators with BPD and substance abuse, among others.
Hostility and anger have been strongly associated with BPD and IPV perpetration in its physical and psychological form (Peters et al., 2017). Otherwise, fear of rejection and loneliness, as well as identity instability, are borderline traits considered risk factors for IPV victimization (Krause-Utz et al., 2021b). All these characteristics could be related with an insecure attachment, which is also associated with violent behaviors and more frequent IPV perpetration (Dutton et al., 1994; Jackson et al., 2015).
A history of childhood maltreatment has also been related to both IPV perpetration and victimization in this population (Krause-Utz et al., 2021b). Childhood maltreatment can lead to an insecure attachment during infancy but also adulthood. According to Dutton et al. (1994) anger, jealousy, BP organization and trauma symptoms significantly correlate with IPV verbal and physical perpetration frequency, and also with insecure attachment. These researchers even suggest that fearful attachment could be also considered anger-attachment, leading to aggressive behaviors such as IPV. In this line, Liu et al. (2011) have found a relationship between childhood maltreatment and IPV perpetration, mediated by BP traits. This disparity in both our results and in the previous literature may indicate the existing relationship between childhood maltreatment and both IPV perpetration and victimization in individuals with BPD features, as Stewart and Vigod (2017) suggest.
Regarding the field of intervention, the benefits that psychotherapy provides in IPV victims with BP traits are shown. Cognitive-narrative therapy, group narrative exposure therapy and counseling contribute to a reduction of those personality features in victims, as well as PTSD and depressive symptoms (Moreira et al., 2020; Orang et al., 2018). It is remarkable the lack of research about this topic, being these two the only ones that approach psychotherapeutic interventions in IPV victims with borderline features.
There are some limitations that have to be taken into account. Firstly, the studies used in this review follow a correlational method, so we cannot establish any causal relationship between BPD and IPV. Secondly, the vast majority of papers use a cross-sectional design, while only three make use of a longitudinal one (Moreira et al., 2020; Munro & Sellbom, 2021; Orang et al., 2018). It would be convenient a greater amount of longitudinal research in order to know implications of this relation throughout the lifecycle. Thirdly, it is important to consider the heterogeneity of criteria used when talking to borderline condition. There are articles that include individuals with BPD while others include those who present BP features. Finally, intimate partner violence is a very broad concept. Differences when measuring this construct are observed, having studies that use subjective impressions, and others using individuals immerse in court proceedings (LaMotte et al., 2019; Mackay et al., 2018; Moreira et al., 2020; Munro & Shellbom, 2020).
Increasing our knowledge about the relationship between BPD and IPV becomes necessary. Longitudinal research would be helpful for this purpose, in order to understand how this association behaves throughout human development. It would also be important to increase knowledge about the relation between BPD and IPV victimization. Besides, implementing interventions in this specific population would be necessary in victims when reducing associated symptoms, as well as in perpetrators in order to prevent the continuation of violence.
Conclusions
Borderline personality features and intimate partner violence are strongly associated, but research for now is centered about perpetrators. This work makes possible a greater understanding about the relation between borderline personality features and being victim or perpetrator of IPV in both males and females. This knowledge allows the use of more specific and effective therapeutic strategies, achieving an intervention focused on the needs of patients with these features.