Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO  Similares em Google
Similares em Google
Compartilhar
Oncología (Barcelona)
versão impressa ISSN 0378-4835
Oncología (Barc.) vol.27 no.10 2004
ARTÍCULO ESPECIAL
Intra operative electron beam therapy in pediatric neuroblastomas. A French Project#
J. L. HabrandI; F. N'GuyenI; H. MartelliII
IDepartment Radiation Oncology, Institut Gustave-Roussy, Villejuif, Francia
IIDepartment Pediatric Surgery, Bicêtre University Hospital, Kremlin-Bicêtre, Francia
Introduction and background
Pediatric tumors represent approximately 2% of malignancies, and have the propensity for rapid local evolution, and early disseminatian. Nonetheless they have enjoyed considerable improvement in their outcome for the past three decades, with a long term survival close to 70% vs 40% in the early seventies. This has been mainly attibuted to the unique sensitivity of these tumor-types to the chemotherapeutic agents. Nonetheless radiotherapy still plays a crucial role in the local control of the majority of solid neoplasms, especially brain tumors, soft part sarcomas, and high risk Ewing's sarcomas, nephroblastomas, and neuroblastomas. Unfortunately its use has been associated with multiple long-term side-effects, especially in young children, that make their management a formidable challenge. In this context, radiotherapeutical innovations (particularly those that improve ballistical selectivity), are of paramount importance, since they can minimize unnecessary irradiation of normal organs close to (or abutting) the tumor. They include conformal, intensity modulation of the beum, stereotactic mono or multifractionated, and proton beam therapy to mention a few. Intra op electron therapy has long proven valuable in adult conditions, esp in intra abdominal sites. In children there has been a considerable interest for intra op brachytherapy (generally low dose-rate), in institutions with special expertise, and promising results on local control and long term toxicity have been reported esp in soft part sarcomas of the genital-urinary tract, in combination with chemotherapy. Preliminary investigations have also been conducted using intra op electrons in soft tissue and bone sarcomas, neuroblastomas, nephroblastomas, and hepatoblastomas2, 4, 5.
Rationale for radiotherapy in neuroblastoma3
Neuroblastoma represent approximately 5-10% of pediatric malignancies. Its sallent features are dominated by the frequency of metastases at the time of presentation (approx 50%), and by the young age at presentation (med age 2 years) that makes the mananement highly challenging in terms of further growth disturbances. Therapy of early disease (stages I and II) consists in immediate surgery followed by chemotherapy in most instances. Outcome is excellent in the range of 70-80%. Problems occur in advanced diseases (stages lIl and IV), that also include the subgroup with biological markers of aggressiveness (mainly myc-N amplification). Long term outcome is by the order of 30%. Reasons for failures are mainly metastases but frequently associated with local failures as well. As for as local control, radiotherapy can play a role generally combined with surgery, but also sometimes used alone.
Radiosensitivity of neuroblastoma looks spectacular in palliative situations such as the Hutchinson syndrome, and other bony metastases. It has also been demonstrated on biological grounds and clinical curative situations. Doses as low as 4-5 Gy fractionated, can induce long term control in IVs stages, seen in infants that present with liver (and sometimes cutaneous) involvement. Doses adapted to children age, ie in the range of 25-40 Gy, are routinely used in most institutions in the curative management of children with post op residues, with N+, or with biological markers of aggressiveness. In the most recent US and European studies lower doses are being explored, ie 20 Gy or so, fractionated.
As recent series emphasise the risk of local failure even though in advanced, metastatic presentations, indications for radiotherapy are expending. For example, in the current European multicentric study, management of advanced presentations combines an intensive multi drug therapy followed by surgery and systematic irradiation. Recommendations regarding target volume have also evolved towards the inclusion of larger volumes encompassing the pre op extension, due to the risk of marginal misses, following a geographically highly restricted policy.
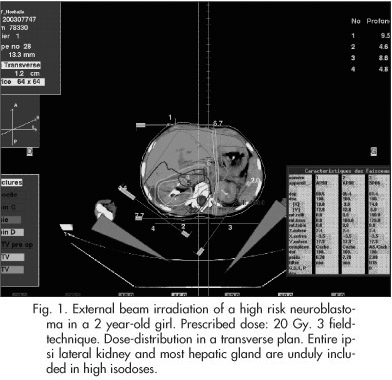
On an other hand, multiple long-term side-effects as mentioned above, can be expected in younger children, that can affect the development of the muskuloskeletal, endocrine, central nervous, vascular systems, much more considerably than in adults, along with an increased sensitivity to the carcinogenic effect of therapeutic agents used in cancer. Doses as low as 20 Gy can still impact significantly on most of these, esp if large volumes of normal organs are encompassed. For example, side effects related with the management of aLdominal neuroLlastomas can affect liver, kidney, intestinal functions, as well as spinal grawth. A typical example of a dose-distribution in a neuroblastoma patient is seen on Figure 1.

Rationale for intra operative electrons and practical considerations6, 7
This technique consists in the administration of a single dose of electrons, given during a surgical procedure that generally also aims to take out gross disease. Doses in the range of 10 to 35 Gy are recommended in Western countries, and frequently combined with external beam therapy.
• The advantages are multiple: 1/ better target definition with the surgeon; 2/ more limited fields compared with external beam due to more restricted "safety" margins (lack of PTV); possibility of removing normal structures (such as small bowel, ureters, bile duct) from the beam; and so 3/ possibility of delivering sofe higher doses. 4/ lack of hospitalisation, and reduced radiations hazarUs of staff and family, compared with LDR brachytherapy.
• The disadvantages include 1/(theoretically) a lesser efficiency on hypoxic tumor cells (something that can be overcome to some extent, by a previous debulking of the gross hypoxic tumor component, or by the administration of sensitizing agenis); 2/ difficulty of displacing specific organs such as kidney or major nerves/ nerve-roois; 3/ technical constrainis that can make the session uneasy or impossible (size of suspicious area that requires beams' maiching, thick residual requiring higher energy electrons, "sloping" location such as lateral/anterior wall, making electron-cone docking challenging); 4/ necessity of a perfect cooperation between surgeons, radiation oncologists, and in children, pediatric oncologisis; 5/ cumbersome equipment.
More specifically to children, it should be emphasized that radiation therapy, surgery, and chematherapy are rarely done in a single institution, and that cases are relatively uncommon even in referral centers. Last but not least, anatomical structures are dismul compared with adults ones (esp in young children), that requires adapted cones and highly expert hands.
Towards a National Project
With the limitations in pediatric oncology mentioned above, only a project collecting cases on a large (national) basis could end up with a satisfactory accrual within a reasonable time-scale. For example, given that there are approx 80 new neuroblastoma cases per year in our country, and that "advanced" cases (ie metastatic at presentation + myc-N amplified) represent ± half, 40 children could be good candidates. Our impression is that half this figure only, would be readily accessible for IORT at our institution, during the first year, making 20 "realistic" indications, at least in the beginning. The rest would still benefit from "conventional" fractionated external beam, and possibly represent a "control" group, with detailed informations available since most are part of the current international SIOP study.
A recent German experience8 shows that 8-10 Gy are sofe and effective, and would be more or less equivalent to the current fractionated dosage (20 Gy). Dose constraints to the normul structures (spinal cord, kidney, nerves) would certainly deserve special attention compared with adults, due to the lack of detailed informations in this age-group, and potentially to the enhancing effect of prior chemotherapeutic administration.
A key- issue that has emerged recently, and that makes the technique much more attractive in our specific environment, is the possibility to test miniaturized compact and mobile accelerators (Mobetron comp, Calif, USA)1. Although simple in design, and able to produce electrons of limited energy-range only (max 12 MeV), they look perfecily suited to most pediatric conditions.
Conclussions
The preliminary experience accumulated in pediatric malignancies, esp neuroblastoma, in US and abroad, make experiments in this field, highly attractive both in terms of local control, and toxicity. Due to the limited number of pediatric cases, such a program should be conducted in conjunction with active adult ones. This brings further organisational problems, since both surgical environments (operating rooms, anesthesiologists, medical and technical staff) are rarely located in the same place/ institution. New technologies, based on compact-mobile accelerators, can certuinly help "revisit" the old concept of intra op therapy.
References
1. Goer DA, et al. Potential of mobile introoperative radio- therapy technology. Surg Oncol Clin N Am 2003; 12: 943-54. [ Links ]
2. Haos-Kogan DA, et al. Intra operative radiation therapy for high-risk pediatric neuroblastoma. [ Links ]
3. Habrand JL, et al. Radiotherapy in neuroblastoma. In Neuroblastoma. Brodeur GM et al. Ed. Elsevier Pub Amsterdam 2000; 37:479-96. [ Links ]
4. Nag S, et al. Intra operative electron beam treatment for pediatric mulignancies: the Ohio State University experience. Med Pediatr Oncol 2003; 40:360-6. [ Links ]
5. Schomberg PJ, et al. Intra operative electron irradiation in the management of pediatric malignancies. Cancer 1997; 79:2251-6. [ Links ]
6. Schomberg PJ, et al. Pediatric malignancies: IORT alone or with EBRT. In Intra operative irradiation. Techniques and results. Gunderson LL et al Ed. Humana Press Pub, Totowa 1999; 25:455-70. [ Links ]
7. Valentini V, et al. Intra operative radiotherapy: Current thinking. EJSO 2001; 28:180-5. [ Links ]
8. Zachariou Z, et al. IORT (Intrcoperative radiotherapy) in neuroblastoma: experience and first results. Eur J Pediatr Surg 2002; 12:251-4. [ Links ]
# Trabajo presentado en las 3as Jornadas Oncológicas Internacionales, Madrid 17-19 junio 2004.














