My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO  Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.96 n.2 Madrid Feb. 2004
| CLINICAL NOTES |
Obscure gastrointestinal bleeding: a complication of radiation
enteritis diagnosed by wireless capsule endoscopy
D. Martínez Ares, B. González Conde, J. Souto Ruzo, M. A. Vázquez Millán, E. Estévez Prieto,
P. Alonso Aguirre and J. L. Vázquez Iglesias
Division of Gastroenterology. Complejo Hospitalario Universitario Juan Canalejo. A Coruña, Spain
ABSTRACT
Obscure gastrointestinal bleeding is a common disorder and may account for as many as 5% of all gastrointestinal hemorrhages. It is often caused by lesions in the small intestine, which were very complicated to examine prior to the advent of wireless capsule endoscopy.
Here we present the case of a 31-year-old woman with obscure gastrointestinal bleeding as a complication of radiation enteritis, which was diagnosed only after she underwent an examination with wireless capsule endoscopy.
This technique has proven to be far superior to other radiographic and endoscopic methods in diagnosing obscure gastrointestinal bleeding and pathologies of the small intestine in general.
Key words: Radiation enteritis. Gastrointestinal bleeding. Obscure gastrointestinal bleeding. Capsule endoscopy.
Martínez Ares D, González Conde B, Souto Ruzo J, Vázquez Millán MA, Estévez Prieto E, Alonso Aguirre P, Vázquez Iglesias JL. Obscure gastrointestinal bleeding: a complication of radiation enteritis diagnosed by wireless capsule endoscopy. Rev Esp Enferm Dig 2004; 96: 132-137.
Recibido: 21-04-03.
Aceptado: 28-04-03.
Correspondencia: David Martínez Ares. C/ Emilio González López, 11, 7º B. 15001 A Coruña. e-mail: dmartinez@sepd.es
INTRODUCTION
The concept of obscure gastrointestinal bleeding covers all causes of GI bleeding that fail to be clarified after performing conventional radiographic and endoscopic tests. In some series they account for as many as 5% of all cases of GI bleeding (1,2). These hemorrhages may be occult, their only manifestation being chronic anemia and a positive result on tests for occult blood in the feces, or they may be overt, appearing as melena or rectorrhage (3). In a large number of cases bleeding originates in the small intestine, a region that is difficult for conventional endoscopy to access. Moreover, radiological studies, which are currently the only procedures that permit the examination of the small intestine, are unable to show small bleeding lesions such as angiodysplasias, which are one of the most common causes of obscure gastrointestinal bleeding (4,5).
With the advent of wireless capsule endoscopy great progress has been made in the study of these portions of the intestine, which have remained unexplored until now. The capsule makes it possible to provide an etiological diagnosis of obscure origin bleeding in 33-100% (6) of cases. In a study compiling the 517 cases published to date, 343 patients (65%) could be diagnosed with wireless capsule endoscopy (7). Following is a case report of a patient with obscure gastrointestinal bleeding associated with a relatively common pathology, but whose diagnosis was only possible after she was examined with this novel endoscopic technique.CASE REPORT
A 31-year-old patient presented to our hospital on two occasions with symptoms of severe anemia. On her second hospital admission, she also exhibited melenic stools. A blood test done on admission showed a hemotocrit value of 24% (normal value is 36-45%) and a hemoglobin level of 8 g/dL (12-15.6 g/dL).
When questioned about her personal background, she reported that eight years earlier a neoplasm of the uterus had been diagnosed and treated with chemotherapy and pelvic radiotherapy. Since that time she had been asymptomatic, with no evidence of a recurrent tumor in follow-up controls.
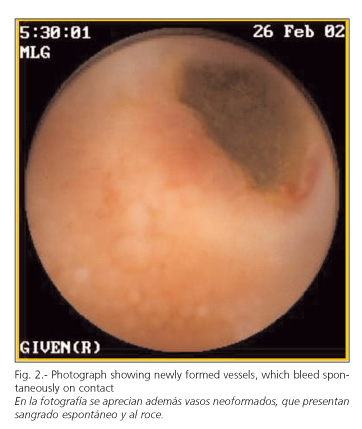
It was decided to perform a gastroscopy, which did not reveal any lesions that could explain her symptoms. Afterward the patient underwent a colonoscopy with ileoscopy, push enteroscopy, and barium examination of the small bowel, all of which had negative results. For this reason we recommended that the patient be examined with wireless capsule endoscopy, since she presented no apparent contraindications. A study of the images revealed the presence of granular, edematous areas in the mucosa, with ulcerated zones producing a slight stenosis at the level of the ileum (Fig. 1) and telangiectasias that bled spontaneously on contact (Fig. 2). Considering the patient's history of pelvic radiotherapy and an unlikely diagnosis of Crohn's disease, our findings strongly suggested radiation enteritis. The ingestion of non-steroid anti-inflammatory medication had also been previously ruled out.
Our recommendation to the patient was surgical treatment. She rejected this possibility, at least for the time being, so we started her on treatment with corticosteroids and 5-ASA. Barring the persistence of a certain degree of anemia, the patient's condition has improved somewhat, and she has not required any more transfusions.
DISCUSSION
Radiation enteritis generally affects the distal ileum, sigmoid colon and rectum (8) owing to their proximity to or their location in the pelvic region, since gynecological neoplasias and prostate cancer are the diseases most frequently treated with radiotherapy.
The damage induced by radiation may be acute, subacute or chronic. Acute lesions are usually due to damage to the epithelium (9), motor disorders from neural irritation, and other anomalies caused by radiation (10,11). Symptoms usually occur a few days or weeks after exposure. Chronic lesions, however, are due to an ischemia in the wall of the intestine caused by a collagenous-vascular lesion. They may appear as strictures, chronic ulcerations, lower gastrointestinal bleeding (occult or overt), perforations of the intestine, formation of fistulous passages or intra-abdominal abscesses, etc. (12). The latency period of these manifestations may range from 6 months to 25 years (13). Our patient presented no evidence of previous symptoms, and eight years had passed since she was last treated with radiation.
In the chronic form of the disease medical treatment is often ineffective, with surgery being required to treat complications (14,15). Our efforts should therefore focus on prevention, either with medication that protects against radiation or anti-inflammatory treatment (16). Also helpful would be the use of absorbable mesh slings which separate the intestine from the field of radiation (17). Our patient rejected surgical treatment after she was given the diagnosis. However, when an evaluation with wireless capsule endoscopy was suggested, she was willing to accept the fact that it might be necessary. If she had refused, the test would have been ruled out, since, as we will discuss below, it is absolutely essential for the patient to be comfortable with this possibility.
Images provided by the capsule were evaluated as highly suggestive of radiation enteritis, particularly in view of the patient's history. The ulcerated areas, the dull appearance of the mucosa, and the constricted areas might be attributed to lesions caused by non-steroid anti-inflammatory medication or even resemble lesions from Crohn's disease, which has been referred to as a cause in as many as 10-20% of the cases of obscure gastrointestinal bleeding (18). The patient professed not to have taken non-steroid anti-inflammatories, and Crohn's disease was ruled out owing to the undamaged state of the terminal ileum and the absence of lesions in other areas. More-over, the presence of the characteristic telangiectasias in the mucosa of the intestine would strongly suggest a possible diagnosis of radiation enteritis, although we could not back it up with histological confirmation.
There is little doubt that the main application of wireless capsule endoscopy today is the study of obscure gastrointestinal bleeding. This technique has also proved to be far superior to push enteroscopy in diagnosing these hemorrhages. Several other studies also corroborate these findings, although only three reported statistically significant results (7). Two have been published as ABSTRACTs (19,20), while only one has been published as a full-length article (21). In this study, Ell et al. reported that push enteroscopy resulted in a diagnosis in 28% of cases, whereas the percentage with wireless capsule endoscopy rose to 66% (p < 0.001).
In virtue of the AGA recommendations on the management of obscure gastrointestinal bleeding (22), routine endoscopic examinations must first be performed before resorting to the capsule. Following this pattern, our patient underwent a gastroscopy, colonoscopy, enteroscopy, and barium examination of the small bowel, all of which had a negative outcome. Not only did the wireless capsule endoscopy reveal lesions prone to bleeding in the small intestine, it also located active bleeding in some of these lesions.Wireless capsule endoscopy might also prove useful in the study of other pathologies of the small intestine besides obscure gastrointestinal bleeding, where other endoscopic techniques have failed to result in a diagnosis (23). Under these circumstances it clearly outranks barium radiology (24).
In addition, an examination using wireless capsule endoscopy is an extremely safe, non-invasive and painless procedure that may be performed on an out-patient basis (23), provided that the patients have been properly screened. The test is not recommended in patients suspected of suffering from stenosis or intestinal obstruction, or in patients having difficulty swallowing or with severe motor disorders of the gastrointestinal tract. It should not be administered if the patient is unable to understand the explanation of the test, and hence, will not be able to collaborate, and in cases where the patient wears an electronic device such as a pacemaker, etc. (25). There are no studies on the use of this test in children under the age of 10. The only absolute contraindication, however, is when the patient clearly exhibits a negative attitude towards surgery or if a surgical procedure would entail an unacceptable risk (26), as surgery may be required to disimpact the device.
In summary, wireless capsule endoscopy has remedied, in part, the grave deficiencies in the techniques that were available to carry out the examination of the small intestine, although roughly 35% of patients with obscure gastrointestinal bleeding will still remain undiagnosed. This technique is safe, with practically no complications at all when performed on patients who have been correctly screened. This non-invasive test has been widely accepted by patients.
REFERENCES
1. Szold A, Katz L, Lewis B. Surgical approach to occult gastrointestinal bleeding. Am J Surg 1992; 163: 90-3. [ Links ]
2. Adrain AL, Krevsky B. Enteroscopy in patiens with gastrointestinal bleeding of obscure origin. Dig Dis Sci 1996; 14: 345-55. [ Links ]
3. Zuckerman GR, Prakash C, Askim MP, et al. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology 2000; 118: 201-21. [ Links ]
4. Douard R, Wind P, Panis Y, et al. Intraoperative enteroscopy for diagnosis and management of unexplained gastrointestinal bleeding. Am J Surg 2000; 180: 181-4. [ Links ]
5. Nolan DJ, Traill ZC. The current role of the barium examination of the small intestine. Clin Radiol 1997; 52: 809-20. [ Links ]
6. Appleyard M, Glukhovsky A, Swain P. Wireless-capsule diagnostic endoscopy for recurrent small-bowel bleeding. N Engl J Med 2001; 344 (3): 232-3. [ Links ]
7. Caunedo Álvarez A, Rodríguez Téllez M, Barroso Relinque N, García Montes JM, Pellicer Bautista FJ, Herrerías Gutiérrez JM. Role of capsule endoscopy in the management of patients with obscure gastrointestinal bleeding. Rev Esp Enferm Dig 2002; 94: 482-7. [ Links ]
8. Yoshimura K, Hirata I, Maemura K, Sugi K, Tahara T. Radiation enteritis: a rare complication of the transverse colon in uterine cancer. Intern Med 2000; 39 (12): 1060-3. [ Links ]
9. MacNaughton WK. Review article: new insights into the pathogenesis of radiation-induced intestinal dysfunction. Aliment Pharmacol Ther 2000; 14 (5): 523-8. [ Links ] 10. Classen J, Belka C, Paulsen F, Budach W, Hoffmann W, Bamberg M. Radiation-induced gastrointestinal toxicity. Pathophysiology, approaches to treatment and prophylaxis. Strahlenther Onkol 1998; 174 (Supl. 3): 82-4. [ Links ]
11. Fraser R, Frisby C, Schirmer M, Blackshaw A, Langman J, Yeoh E, et al. Effects of fractionated abdominal irradiation on small intestinal motility: studies in a novel in vitro animal model. Acta Oncol 1997; 36 (7): 705-10. [ Links ]
12. Nguyen NP, Antoine JE. Radiation enteritis. In: Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger and Fordtran's, Gastrointestinal and Liver Disease. Philadelphia: Saunders, 2002. p. 1996-7. [ Links ]
13. Nguyen NP, Antoine JE. Radiation enteritis. In: Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger and Fordtran's, Gastrointestinal and Liver Disease. Philadelphia: Saunders, 2002. p. 1998. [ Links ]
14. Regimbeau JM, Panis Y, Gouzi JL, Fagniez PL. Operative and long term results after surgery for chronic radiation enteritis. Am J Surg 2001; 182 (3): 237-42. [ Links ]
15. Pagano A, Vaccaro F, Romano G, Romano G Surgical treatment of radiation enteritis. Minerva Chir 1996; 51 (3): 93-6. [ Links ]
16. Kilic D, Eeghan I, Ozenirler S, Dursun A. Double-blinded, randomized, placebo-controlled study to evaluate the effectiveness of sulphasalazine in preventing acute gastrointestinal complications due to radiotherapy. Radiother Oncol 2000; 57 (2): 125-9. [ Links ]
17. Rodier JF, Janser JC, Rodier D, Dauplat J, Kauffmann P, Le Bouedec G, Giraud B, Lorimier G. Prevention of radiation enteritis by an absorbable polyglycolic acid mesh sling. A 60-case multicentric study. Cancer 1991; 68 (12): 2545-9. [ Links ]
18. Hahne M, Adamek HE, Schilling D, Riemann JF. Wireless capsule endoscopy in a patient with obscure occult bleeding. Endoscopy 2002; 34 (7): 588-90. [ Links ]
19. Gay G, Saurin JC, Gaudin JL, et al. Comparison of wireless endoscopic capsule and push-enteroscopy in patients with obscure ocult/overt digestive bleeding: results of a prospective, blinded, multicenter trial. First Given conference on capsule endoscopy. Rome, 2002. p. 17-9. [ Links ]
20. Pennazio M, Santucci R, Rondonotti E, et al. Wireless capsule endoscopy in patients with obscure gastrointestinal bleeding: results of the italian multicentre experience. First Given conference on capsule endoscopy. Rome, 2002. p. 17-9. [ Links ]
21. Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy 2002; 34 (9): 685-9. [ Links ]
22. American Gastroenterological Association medical position statement. Evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology 2000; 118: 197-200. [ Links ]
23. Scapa E, Jacob H, Lewkowicz S, Migdal M, Gat D, Gluckhovski A, et al. Initial experience of wireless-capsule endoscopy for evaluating occult gastrointestinal bleeding and suspected small bowel pathology. Am J Gastroenterol 2002; 97 (11): 2776-9. [ Links ]
24. Costamagna G, Shah SK, Riccioni ME, Foschia F, Mutignani M, Perri V, et al. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology 2002; 123 (4): 999-1005. [ Links ]
25. Barroso Relinque N, Caunedo Álvarez A, Rodríguez Téllez M, Herrerías Estéban JM, Pellicer Bautista F, Herrerías Gutiérrez JM. Wireless endoscopy. Rev Esp Enferm Dig 2001; 93: 598-601. [ Links ]
26. Cave DR. Wireless Video Capsule Endoscopy. Clinical Perspectives in Gastroenterolgy 2002: 203-7. [ Links ]











 text in
text in