My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO  Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.96 n.3 Madrid Mar. 2004
| CLINICAL NOTE |
Hemobilia secondary to chronic cholecystitis
R. de Quinta Frutos, L. Moles Morenilla, F. Docobo Durantez1, J. A. Soto Pradas2, J. Iriarte Calvo3
and A. Vázquez Medina
Departments of General Surgery, 2Gastroenterology and 3Pathology. Hospital Militar Vigil de Quiñones.
1Unit of Clinical Administration. C.M.A. Hospital Universitario Virgen del Rocío. Sevilla, Spain
ABSTRACT
The term hemobilia is used to describe the presence of blood in the biliary tract. We report a case of symptomatic hemobilia associated with chronic cholecystitis in a 57-year-old man with jaundice, gastrointestinal hemorrhage, and epigastric pain.
We review the etiology of this condition and highlight the role of abdominal ultrasonography in its diagnosis. In our case, abdominal ultrasonography revealed the presence of clots inside the gallbladder.
The clinical condition was resolved by means of a cholecystectomy. The patient had an uneventful recovery.
Key words: Hemobilia. Ultrasound imaging. Cholecystitis.
de Quinta Frutos R, Moles Morenilla L, Docobo Durantes F, Soto Pradas JA, Iriarte Calvo J, Vázquez Medina A. Hemobilia secondary to chronic cholecystitis. Rev Esp Enferm Dig 2004; 96: 221-225.
Recibido: 13-05-03.
Aceptado: 25-06-03.
Correspondencia: Luis Moles Morenilla. Avda. S. Francisco Javier, 20-A, 3º-2. 41018 Sevilla. Tel. +34 954662445.
INTRODUCTION
The term hemobilia was introduced in 1948 by Sandblom to describe a hemorrhage into the biliary tree caused by a pathologic communication between the blood vessels and the bile ducts (1). In the 17th century, Glisson described this condition for the first time (2). It is mainly characterized by the typical clinical triad of colic pain in the right hypochondrium, jaundice, and digestive hemorrhage (3).
Hemobilia is a rare syndrome, and although its detection is increasing in frequency, its treatment continues to be a controversial matter. Ultrasound imaging represents an efficient and safe technique for the diagnosis of the condition and the control of its progress, as it allows the detection of clots in the biliary tree and inside the gallbladder, as well as the presence of aneurysms or intrahepatic hematomas (4).
We report a case of symptomatic hemobilia in the gallbladder. Abdominal ultrasounds allowed the potential source of hemorrhage to be detected. We carry out a brief review of the etiopathogenesis of the disease, and highlight the significance of ultrasonography in its diagnosis.
CASE REPORT
Our patient was a 57-year-old male with a history of high blood pressure, hiatal hernia, chronic alcohol abuse, and heavy smoking who had undergone surgery for left renal lithiasis. His regular treatment consisted of: acamprosate; clomethiazol; hydroxicobalamin, pyridoxine, thiamin; tiapride, and nifedipine.
The patient was examined at the emergency department for a temperature of 39 ºC -which had lasted for two days- anorexia, and asthenia. He reported having lost 15 kg in the preceding months and occasionally suffering space and time disorientation.
Physical examination demonstrated a heart rate of 129 bpm, blood pressure 131/64 mmHg, and axillary temperature of 39 ºC. The patient was conscious and coopera-tive, and had the following clinical manifestations: bradypsychia, lack of nuchal rigidity, slight conjunctival jaundice, decreased vesicular murmur on the right base, occasional wheezing in both pulmonary fields, rhythmical cardiac tones, soft, depressible abdomen with hepatomegaly measuring four finger widths, tender mass in right hypochondrium, and preserved peristaltic movements. There were no edemas in his lower limbs, although some trophic disorders were noted.
An initial analysis revealed leukocytosis (14.700) with 82% neutrophilia, 10.3% lymphocytes, and 14.0-g/dl hemoglobin. The coagulation study was normal. The findings of the biochemical study were: total bilirubin 1.9 mg/dl, direct bilirubin 1.4 mg/dl, indirect bilirubin 0.4 mg/dl, GOT 133 U/L, GPT 109 U/L, AP 247 U/L, total proteins 6.3 g/dl, cholesterol 130 mg/dl, and glucemia 158 mg/dl.
Chest and plain abdominal radiographs revealed no significant findings.
The patient was hospitalized for examination and treatment. In the following days, he had dark stools and nausea.Ultrasonographic findings included a distended gallbladder with heterogeneous echogenic content and no sound contrasts, irregular thickening of the wall, successive images suggesting clots in the gallbladder, thick bile consistent with bleeding inside the gallbladder or with an advanced inflammatory process; liver with no pathological signs or cholestasis. The common bile duct measured 6 mm near the head of the pancreas; the spleen was normal, and no adenopathies were observed in the hepatic ileus or the retroperitoneal area.
The day after admission the patient had a fever peak of 39 ºC, and the serial blood culture obtained was positive for Escherichia coli. During the following days, temperature dropped when an antibiotic treatment was started.
Between days seven and ten after hospitalization, the patient suffered from recurring episodes of intense epigastric pain while jaundice increased progressively. By the tenth day his total bilirubin was 3.5 mg/dl; direct bilirubin 2.9 mg/dl. Hematocrit count fell to 24.2% and hemoglobin to 7.8 g/dl. A test for detecting the presence of occult blood in stools was positive. Three units of packed red cells were transfused. Tumor markers were normal, except for CA 19.9: 127.6 U/ml.
An abdominal computed tomography scan showed a solid shape in the gallbladder, which was compatible with vesicular neoplasm; the size and shape of the liver were normal.
Having diagnosed hemobilia, it was indicated that the patient underwent an explorative laparotomy. After a right sub-costal incision, it was found that the patient's gallbladder had a normal appearance but was moderately dilated. The liver was slightly enlarged but had a normal appea-rance; pancreatic palpation was normal. A transcystic cholangiography revealed no pathological findings and a cholecystectomy was subsequently performed. When the gallbladder was opened, a large clot was found inside.
The results in the report by the pathologist were: cholecystectomy piece measuring 9 x 4 cm with a rigid and shiny outer surface; the surface of mucosa was eroded and destructured; gallbladder demonstrates a site of recent bleeding.
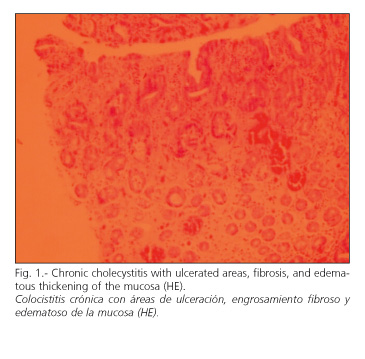
Diagnosis: chronic cholecystitis with areas of ulceration in the mucosa; fibrous and edematous thickening of the mucosa, lack of neoformative process (Fig. 1).
The postoperative course was good, with clinical and analytical improvement, and normalization of both the hemogram and hepatic function tests. The patient was discharged from hospital ten days after surgery. After two years, he has not presented with further episodes of digestive hemorrhage or any other symptomatology.
DISCUSSION
According to Sandblom, the main causes of hemobilia are: accidental or surgical trauma, inflammatory lesion, biliary lithiasis, hepatic tumors, and aneurysms (2). Nowadays 40% of hemobilia cases occur after diagnostic and therapeutic tests (5,6) are performed on the bile ducts or the liver (7,8). The term "hemocholecystitis" refers to hemorrhage inside the gallbladder. It may be caused by stones, tumors, and acute or chronic cholecystitis, which produce ulcerations and necrosis in the mucosa (9) or direct erosion in a vessel. Bile has a lithic action which increases the duration of the lesion. In our case the hemobilia was caused by chronic cholecystitis with ulceration in the mucosa. A site of recent bleeding was also detected.
Typical symptoms include jaundice, colic pain in the right upper quadrant followed by digestive hemorrhage. The pain usually improves after the hematic loss. The degree of jaundice varies depending on the extent to which the choledochus is obstructed by clots (3). Hepatomegaly or a palpable mass in the right hypochondrium are commonly found (9).
Episodes of pain and digestive bleeding are recurrent until an etiologic treatment is started. Our patient presented with jaundice, epigastric pain, anemia, melena, hepatomegaly and a mass in the right hypochondrium. When a gastrointestinal hemorrhage is associated with biliary disorders, a diagnosis of hemobilia should be considered (10). Another aspect that should be born in mind is that the rates of morbidity and mortality are proportional to the delay in inhibiting the hemorrhage. Therefore, hemobilia should be included in the dif-ferential diagnosis of obstructive jaundice, gastrointestinal hemorrhage, anemia, and upper abdominal pain (1).
Upper digestive endoscopy can rule out other more frequent causes of hemorrhage; in 30% of hemobilia cases, clots exiting through the papilla are observed (5,11). In our case, an endoscopy could have contributed to pro-duce a more comprehensive study of the patient. Abdominal ultrasounds are a useful technique for reaching a diagnosis of hemobilia, as it can detect the presence of clots inside the gallbladder or bile duct (4,12). It also allows the detection of other lesions, such as hepatic hematoma, aneurysms in the hepatic artery, as well as neoplasms in the bile ducts, liver and pancreas, which could originate the hemorrhage (5,13). In addition to the gallbladder blood clots, biliary sludge, pus, and the exophytic growth of a cancer have all a similar echographic appearance (14). In our patient ultrasound imaging showed the presence of a large clot inside the gallbladder, with no subsequent sound contrast.
Other complementary studies used to determine the source of hemobilia include: abdominal CT scans, cholangio MRI, scintiscans using erythrocytes marked with technetium, endoscopic retrograde cholangio-pancreatography, and percutaneous transhepatic cholangiography.
The diagnosis of hemobilia can also be reached by performing an arteriogram of the celiac artery, as it has the greatest sensitivity for localizing the bleeding site, provided that there is sufficient bleeding (1).
In the initial treatment of hemobilia, selective arterial embolization is recommended, as it is an effective procedure and has a low rate of complications (15,16). Surgery should be reserved for cases of embolization failure or complication, resectable tumor, or, as was the case with our patient, cholecystitis (17), when after cholecystectomy hemorrhage, pain, and jaundice disappeared.
In conclusion, hemobilia is a rare condition which is presently mainly associated with procedures performed on the liver and bile ducts. It should be included in the differential diagnosis of patients with jaundice and digestive hemorrhage. Abdominal ultrasounds is a rapid, painless, and efficient diagnostic technique for the detection of various lesions which may cause hemobilia; therefore it is, together with endoscopy, the recommended initial diagnostic procedure.
REFERENCES
1. Goodnight JE Jr, Blaisdell FW. Hemobilia. Surg Clin North Am 1981; 61: 973-9. [ Links ]
2. Sandblom P. Hemobilia. Surg Clin North Am 1973; 53: 1191-201. [ Links ]
3. Whelan TJ Jr. Hemobilia. En: Davis-Christopher (eds). Textbook of Surgery. Sabiston DC. 11ª ed. Philadelphia: WB Saunders Co, 1977. p. 1230-5. [ Links ]
4. Escolano CM, Lozano C, Cuesta A, Bonilla F, Blázquez JC, Vigueras I, et al. Hemobilia sintomática tras biopsia hepática. Valor de la ecografía en el diagnóstico y control de esta complicación. Rev Esp Enferm Dig 1995; 87 (2): 169-73. [ Links ]
5. Defarges V, Loscos JM, Meroño E, Fernández Madrid J, Carda P. Dolor e ictericia secundario a hemobilia resuelto mediante CPRE y esfinterectomía endoscópica. Rev Esp Enferm Dig 1996; 88 (6): 443-5. [ Links ]
6. Cetta F, Montalto G, Zuckermann M, Cetta D. Hemobilia, infection, bile stasis and intrahepatic stones in liver transplant recipients. Surgery 1998; 123 (1): 115-7. [ Links ]
7. Hayashi N, Sakai T, Kitagawa M, Kimoto T, Inagaki R, Ishii Y. US-guided Left-sided Biliary Drainage: Nine-year experience. Radiology 1997; 204 (1): 119-22. [ Links ]
8. Livraghi T, Goldgerg SN, Lazzaroni S, Meloni F, Solbiati L, Gazzelle GS. Small hepatocellular Carcinoma: Treatment with Radio-frequency Ablation versus Ethanol Injection. Radiology 1999; 210(3): 655-61. [ Links ]
9. Sáinz B, Sueiras A, Buera M, Sola M, López Cano M, Vicens C, et al. Colecistitis como causa rara de hemobilia. Cir Esp 1995; 58 (2): 165-7. [ Links ]
10. Sandblom P, Mirkovitch V. Hemobilia: Some salient features and their causes. Surg Clin North Am 1977; 57: 397-408. [ Links ]
11. Sánchez-Pernaute A, Pérez Aguirre E, Ochagavía S, González López O, Díez L, Roca V, et al. Hemobilia en un paciente VIH positivo con trombocitopenia. Resolución mediante esplenectomía. Cir Esp 1998; 64: 486-8. [ Links ]
12. Obi S, Shiratori Y, Shiina S, Hamamura K, Kato N, Imamura M, et al. Early detection of haemobilia associated with percutaneous ethanol injection for hepatocellular carcinoma. Eur J Gastroenterol Hepatol 2000; 12 (3): 285-90. [ Links ]
13. Birth M, Ortlepp J, Bontikous S, Amthor M, Weiser HF, Bruch HP. Intermittent activity- induced hemobilia caused by liver hemangioma. Dig Surg 2000; 17 (3): 292-6. [ Links ]
14. Bruguera CA. Hemobilia. En: Ecografía abdominal. Barcelona: Salvat (eds), 1982. p. 87. [ Links ]
15. Alcindor K, Hernández M, Moles L, Moles JC, Marcos F. Hemobilia masiva postoperatoria tratada con éxito mediante la embolización arterial selectiva. Rev Quir Esp 1984; 11(3): 157-61. [ Links ]
16. Van Os EC, Petersen BT. Pancreatitis secondary to percutaneous liver biopsy-associated hemobilia. Am J Gastroenterol 1996; 91 (3): 577-80. [ Links ]
17. Dousset B, Sauvanet A, Bardou M, Legmann P, Vilgrain V, Belghiti J. Selective surgical indications for iatrogenic hemobilia. Surgery 1997; 121 (1): 37-41. [ Links ]











 text in
text in