Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 no.3 Madrid mar. 2006
CLINICOPATHOLOGICAL CONFERENCE
A young woman with first-trimester metrorrhagia, fever and skin lesions
A. Lalueza Blanco, D. Rodríguez Alcalde1, C. González Gómez, G. López2, P. Martínez Montiel1, E. Sanz García3 and J. A. Solís Herruzo1
Departments of Internal Medicine, 1Gastroenterology, 2Pathology and 3Radiology. Hospital Universitario 12 de Octubre. Madrid, Spain
ABSTRACT
Inflammatory bowel disease commonly affects women with child-bearing potential, and clinical activity extent is most relevant at the time of conception. Below, we report on the case of a 19-year-old woman who was admitted for first-trimester metrorrhagia and fever, with various extraintestinal manifestations, mainly including erythema nodosum and episcleritis during the course of disease. The differential diagnosis of these manifestations led to the diagnosis of Crohn's disease, which involved the whole colon.
Key words: Inflammatory bowel disease. Erythema nodosum. Extraintestinal manifestations. Pregnancy.
Lalueza Blanco A, Rodríguez Alcalde D, González Gómez C, López G, Martínez Montiel P, Sanz García E, Solís Herruzo JA. A young woman with first-trimester metrorrhagia, fever and skin lesions. Rev Esp Enferm Dig 2006; 98: 204-215.
Case report presentation
Dr. C. González Gómez. Department of Internal Medicine: A 19-year-old gypsy woman presented in our Emergency Department with first-trimester metrorrhagia and fever.
Initially she had hypogastric pain and fever up to 39 ºC, which was clinically and hemodynamically well tolerated. A scraping procedure was performed, following which abdominal pain improved; however, high temperature persisted despite this procedure and the use of ampicillin, gentamycin, and metronidazole. Baseline laboratory workup revealed moderate leukocytosis, and microcytic anemia.
Given the patient status her admission to the internal medicine ward was decided upon. On new history taking the patient reported a previous pregnancy that yielded a healthy, currently 16-months-old child, and having lost 15 kg of weight in the absence of hyperorexia since then. She reported having taken no oral contraceptives, and no other medications or toxics. For 15 days before admission she had two or three soft stools daily with no pathologic products, but she had spontaneously recovered before visiting the emergency room.
During the review of systems she reported no other systemic symptoms, except a number of painful lesions in the oral mucosa that she had never consulted for.
During her stay at the Gynecology Department a number of erythematous, papulonodular lesions in various stages developed on her skin; these were widespread but predominated in the lower limbs, particularly in the pretibial area. Subsequently she had an episode of monoarthritis in her right knee with inflammatory, sterile synovial fluid.
Physical examination
Blood pressure: 93/50. Temperature 38 ºC. Severe thinness overall. Head and neck: normal venous pressure. No lesions in the oral mucosa. Conjunctival elevated white-yellowish lesion with hyperemia on the medial aspect of both eyes, with a foreign-body sensation (Fig. 1). Chest: cardiopulmonary auscultation, rhythmic at 130 beats per minute; rest, normal. Abdomen: moderate painful hepatomegaly; tenderness in right iliac fossa and hypogastrium, with no peritonism or palpable masses. Limbs: no osteoarticular symptoms. Skin: papulous, nodular, erythematous, hyperemic lesions in various stages, predominating in the lower limbs (Fig. 2).
Laboratory tests
Blood test: hemoglobin 8.2 g/dl; hematocrit 26%; MCV 70 fl; MCH 22 pg; platelets 551,000/mm3; leukocytes 8690/mm3 (N 60%; L 30%; M 6%); reticulocytes 0.55%; absolute reticulocyte count 20,800/mm3; ESR 100 mm/h. Coagulation: prothrombin activity 85%; INR 1.12; APTT 31.2 s; fibrinogen 504 mg/dl. Chemistry: glucose 87 mg/dl; LDH 107 IU/l; GOT 18 IU/l; GPT 16 IU/l; gamma-GT 118 IU/l; AP 344 IU/l; total bilirubin 0.31 mg/dl; total proteins 6.4 g/dl; albumin 2.85 g/dl; creatinine 0.62 mg/dl; calcium 8.7 mg/dl; phosphorus 3.9 mg/dl; uric acid 3.1 mg/dl; cholesterol 118 mg/dl; triglycerides 100 mg/dl; sodium 137 mEq/l; potassium 4.6 mEq/l. Thyroid hormones: free T4 1.3 ng/dL; TSH 1.8 µIU/mL. Iron profile: iron 25 µg/dl; ferritin 226 ng/ml; transferrin 153 mg/100; TIBC 216 mcg/100; SAT-transferrin 12%. Urinalysis: density 1020; pH 7; leukocytes +++; rest, negative; with some bacteria, 4 RBCs per field, 25 leukocytes per field and some amorphous phosphates; folic acid: 2.73 ng/ml. Vitamin B-12: 1.85 pg/ml. Clostridium difficile toxin: positive. Repeat coprocultures: negative. Repeat blood cultures: sterile. Mantoux: negative. HIV: negative. Chest x-rays on admission was normal, and abdomen x-rays showed an abnormal luminogram in the right iliac fosse with thickened submucosal structure.
Comments and clinical course
Dr. A. Lalueza Blanco. Department of Internal Medicine: In summary, this is a young woman who, since delivering her first child 16 months ago, had a constitutional syndrome with severe weight loss and clear protein-energy malnutrition signs. Fifteen days before admission she had a transient episode of scarce diarrhea with no abnormal products and in association with hypogastric pain that spontaneously subsided with no treatment. She presented to hospital with first-trimester metrorrhagia and fever up to 39 ºC, and thus underwent scraping, which managed to improve abdominal pain while fever persisted despite antibiotic therapy. A sole microbiologic evidence had been available that far, namely the presence of Clostridium difficile toxin in her stools, which was adequately managed. Severe hepatomegaly associated with bilateral episcleritis and elevated skin lesions predominating in the lower limbs, which suggested erythema nodosum, was seen during admission.
These findings suggest the presence of a systemic inflammatory process involving various organs, although the presence of infection -mainly subacute- accounting for the patient's illness cannot be excluded at the present time.
Before proceeding with differential diagnosis, I would like to know whether the histologic study of skin lesions confirmed a diagnosis of erythema nodosum.
Dr. G. López (Department of Pathology): The histologic study of skin lesions showed changes suggestive of suppurative septal panniculitis. There was an inflammatory infiltrate in the dermis and subcutaneous tissue made up by lymphocytes and histiocytes in association with edema (Fig. 3). This lesion may be found in infectious panniculitis, alpha-1 antitrypsin deficiency, and erythema nodosum.
Dr. A. Lalueza Blanco (Department of Internal Medicine): Given the patient's history, the most likely diagnosis is that of erythema nodosum, which forces to rule out causes most commonly associated therewith (1,2) (Table I).
While not very accurately, we may divide up erythema nodosum into those accompanied by mediastinal adenopathies (M. tuberculosis, sarcoidosis, lymphoma, fungi, Chlamydia and Yersinia), and those associated with gastrointestinal symptoms [inflammatory bowel disease (IBD), Behçet's disease, Whipple's disease, pancreatitis, and bacterial gastroenteritis by Shigella, Yersinia or Campylobacter]. However, before getting into the differential diagnosis for erythema nodosum as manifested by this patient, I would order an abdomino-pelvic computerized tomography (CT) scan to rule out gynecological complications and then attempt to anatomically document her hypogastric pain. In addition, we should have a chest-PA, Mantoux test, and ASLO titers available, as Streptococcus pyogenes is most commonly associated with erythema nodosum. Similarly I would request a serology for hepatotropic viruses and HIV, an intradermoreaction and cultures for Mycobacteria, genital, anal, and oropharyngeal exudates, reaginic and treponemic tests, a coproculture, a search for parasites and C. difficile toxin in stools, angiotensin-converting enzyme (ACE) titers, and 24-hour calciuria. I would also have an interest in cryoglobulins, C-reactive protein (CRP), anticardiolipin antibodies, antinuclear antibodies (ANA), anti-neutrophil cytoplasm antibodies (ANCA), rheumatoid factor, and blood-borne tumor markers. Finally, I would order a colonoscopy and gastrointestinal follow-through to exclude IBD.
Computerized tomography (CT)
E. Sanz García. Department of Radiology: Abdominal CT scans showed hepatomegaly with left-lobe hypertrophy and splenomegaly, where a hypodense lesion suggestive of infarction could be seen. There were no septic thrombophlebitis signs. The presence of diffuse thickening in the colonic wall and a cystic 2-cm anexal lesion also stood out (Fig. 4).
This patient also underwent an intestinal follow-through where the stomach, duodenal bulb, and jejunal loops with no apparent abnormalities could be seen; in contrast, the distal ileum was severely involved and exhibited marked changes in its wall; margins appeared strongly irregular and folds were thickened (Fig. 5).
Dr. P. Martínez Montiel (Department of Gastroenterology): Regarding the studies you want to know, I inform you that this patient underwent the following laboratory tests: beta-2 microglobulin, 3.32 mg/L; tumor necrosis factor alpha, 30 ng/mL; ANA, negative; c-ANCA and p-ANCA, negative; anticardiolipin antibodies, IgG, 4.8 U/mL; IgM, lower than 0.07 U/mL; CRP, 11.5 mg/dL; rheumatoid factor, lower than 20 IU/mL; ASLO, lower than 200 IU/mL; cryoglobulins, negative; ACE, 37.5 IU/L; urine calcium, 7.5 mg/%. Serologies for rubella, toxoplasma, Epstein-Barr virus and cytomegalovirus with positive IgG and negative IgM. Serology for HIV, negative. Serology for hepatitis C, negative; serology for hepatitis B: negative HBsAg and anti-HBc. Endocervical, anal, and pharyngeal cultures were negative. Intradermoreaction, fluorescence staining, and sputum culture for Mycobacterium tuberculosis were all negative. Last, an abdominal scan using Tc99m-labelled leukocytes showed an abnormal leukocyte accumulation in the hypogastrium.
Dr. A. Lalueza Blanco (Department of Internal Medicine): As we just saw, CT ruled out any gynecological disorder accounting for the patient's manifestations; it rather showed colonic wall changes in the form of thickened wall areas. On the other hand, the intestinal follow-through demonstrated extensive involvement at the distal ileum, which was consistent with the findings of the abdominal scan using labelled leukocytes, which showed abnormal leukocyte accumulation in the hypogastrium. In our opinion, differential diagnosis should include those conditions where erythema nodosum associates with bowel manifestations, specifically with ileal and colonic involvement, and 1-year-standing systemic symptoms.
Among infectious causes Mycobacterium tuberculosis stands out, and might therefore account for both the patient's 1-year-long constitutional syndrome and terminal ileum involvement. Ileocecal involvement is found in 80-90% of patients with abdominal tuberculosis (3,4), and the most common symptom is diarrhea. Abdominal pain, fever, nocturnal sweating, distension, and weight loss are less common. Ileal involvement is commonly associated with local adenopathies -usually massive and with central low attenuation areas related to caseous necrosis; dual-contrast barium studies usually show ulcers longer than those seen in Crohn's disease (5). None of this was found in this patient; hence a diagnosis of intestinal tuberculosis was unlikely. While only 15% of patients with intestinal tuberculosis have evidence of associated pulmonary disease (4), the fact that chest x-rays, Mantoux tests, and sputum Ziehl stainings were consistently negative (subsequently confirmed by cultures) makes this diagnosis even more unlikely.
Bacterial gastroenteritis, mainly by Shigella spp., Yersinia spp. and Campylobacter spp., could be another potential cause of erythema nodosum, which would account for diarrhea. However, the progression of some symptoms (1-year-standing constitutional syndrome), the self-limited nature of diarrhea with no abnormal products in the stools, and stool culture negativity make it little likely. The search for Yersinia would lead to the identification of specific antibodies, since stool culture was negative for pathologic bacterial flora (6). Among the remaining bacterial causes for gastroenteritis, the only one that should be considered is Neisseria gonorrhoeae, even though the prolonged course, and the fact that antibiotics covering this pathogen had been received with no clinical improvement, as well as microbial culture negativity would rule it out.
Sarcoidosis may explain arthritis, uveitis, and skin involvement. While exceptional, ileal involvement has been described in 17 cases of intestinal sarcoidosis in the absence of respiratory symptoms (7), which greatly complicates differential diagnosis versus Crohn's disease. The fact that chest x-rays was strictly normal, together with calciuria and normal ACE titers, make the diagnosis of sarcoidosis difficult (8). In patients with sarcoidosis ACE sensitivity for this disease ranges from 58 to 86%, depending on disease activity; in contrast, this test's specificity reaches 90%. They may be present in tuberculosis, silicosis, primary biliary cirrhosis, and lymphoma, but not in Crohn's disease (7-11).
Among systemic causes Behçet's disease and systemic lupus erythematosus (SLE) should be ruled out. The former disease may account for erythema nodosum, for gastrointestinal symptoms, and potentially for oral aphthae as reported in the patient's history. Behçet's disease may affect any portion of the bowel, but the ileocecal region is most commonly compromised (12). Histologic lesions and similar extraintestinal manifestations may render the distinction between Behçet's disease and Crohn's disease a difficult task (13-15). Pain is the most commonly seen abdominal symptom, and is present in some series in up to 90% of patients, followed by diarrhea and gastrointestinal bleeding (12). However, this patient does not meet the criteria allowing a diagnosis of Behçet's disease, mainly the major criteria (recurrent oral ulers with at least 3 episodes in 12 months), and only has one of the minor criteria (skin lesions including erythema nodosum). She reported no recurrent genital ulcers, ocular lesions or pathergy (16). Colonoscopy usually demonstrates deep isolated ulcers in the ileocecal region (12). LSE, while a most uncommon cause of erythema nodosum (17), may explain skin lesions; however, the patient's immune profile and the absence of additional clinical or blood data make it little likely; in addition, diarrhea is not easily explained by this condition.
IBD may justify the constitutional syndrome's progression, as well as abdominal pain, radiographic bowel findings, and fever at admission; however, the fact that gastrointestinal symptoms were scarce is outstanding. In this disease, up to 35% of patients have extraintestinal manifestations. In our case report, the patient had erythema nodosum. This finding occurs in 15% of patients -it usually develops during flare-ups and is closely linked to peripheral joint disease. At admission the patient had type-1 peripheral arthritis symptoms involving the right knee. Episcleritis is the most commonly occurring ocular symptom in Crohn's disease, and affects 5% of patients (18); its severity is also parallel to that of bowel disease (19-23).
Among erythemas nodosa of tumoral origin Hodgkin and non-Hodgkin lymphomas stand out, as do leukemias; however, no laboratory parameters warrant such diagnoses. From a pathological standpoint, a cecal carcinoma or carcinoid tumor might also be considered.
To clear doubts I truly believe that colonoscopy -plus ileoscopy if possible- in association with the sampling of lesions encountered is essential.
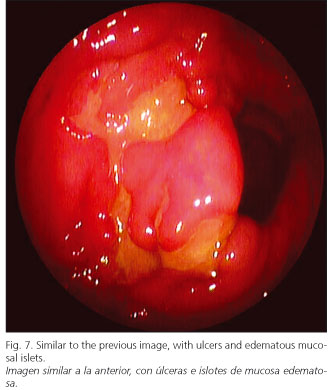
Dr. D. Rodríguez Alcalde (Department of Gastroenterology): Colonoscopy showed a patchy involvement of the whole colon with numerous fibrin-covered ulcers, some of them serpiginous, that bled on touch; the biggest ulcers were up to 3-3.5 cm in size, alternating with apparently normal mucosal areas (Figs. 6 and 7). In the vicinity of ulcers, and within some of them, there were millimetric pseudopolypoid formations consistent with damaged mucosal areas, whereas mucosal regions far removed from ulcers had a normal macroscopic appearance with a well preserved vascular pattern. Involvement was more severe in the descending colon and sigma, while only a few aphthae were found in the rectum. Ileoscopy only managed to show the most distal 5-7 cm, but no lesions were seen in that ileal portion. All of this was trongly suggestive of IBD, specifically Crohn's disease with pancolonic involvement in a moderate flare-up.
Dr. G. López (Department of Pathology): Colorectal biopsy showed a severely distorted glandular architecture and densely packed, mixed inflammatory infiltration reaching beyond the muscularis mucosae and into the submucosa. Microabscesses and cryptitis were apparent. It was all strongly suggestive of idiopathic inflammatory disease, most likely Crohn's disease with high inflammatory activity (Figs. 8 and 9).
Dr. C. González Gómez (Department of Internal Medicine): Indeed, with a presumed diagnosis of Crohn's disease involving the whole colon and terminal ileum treatment was empirically started with mesalazine 800 mg and intravenous methylprednisolone 1 mg/kg/day. Fever regressed within 48 hours, and both extraintestinal manifestations and laboratory changes gradually improved to the point that the patient could be discharged.
Dr. A. Lalueza Blanco (Department of Internal Medicine): Chronologically, a fact to point out in this patient is the development of insidious manifestations including weight loss in the wake of her first pregnancy, with a subsequent episode of severe extraintestinal manifestations during the second pregnancy. These are the two most interesting aspects of this case: extraintestinal manifestations and then the association of pregnancy with IBD.
During pregnancy, there is seemingly no higher risk for spontaneous abortion, and pregnancy is no risk factor for IBD relapse. Also, fertility has not been seen to decrease except in patients with proctocolectomy or ileoanal anastomosis. In this respect it must be stressed that sulfasalazine induces reversible hypomotility and oligospermia in 80% of males receiving this drug (24,25).
We may pose a couple of questions here -on the one hand whether pregnancy affects IBD activity; on the other hand how may this disease impact on pregnancy. Regarding the former question, there is a clear association with activity extent during pregnancy: if the condition is stable at pregnancy onset, it will probably remain like that until the end of pregnancy. Inflammatory disease relapses during pregnancy in one third of patients, but this percentage does not differ from that of relapse risk among non-pregnant women (26). On the contrary, if IBD is active when pregnancy starts, this flare-up will probably remain for the rest of pregnancy (70% of patients). IBD complications that may occur during pregnancy do not differ from those seen in non-pregnant patients. No differences exist during the postpartum period either (27). In the presence of perineal involvement a Caesarean section is often advised; when IBD is inactive or during mild-to-moderate flare-ups vaginal delivery is possible, but episiotomy is advised against given the subsequent fistulization risk (28,29).
Crohn's disease has a greater impact on fetal development when compared to ulcerative colitis; in fact, ulcerative colitis is thought not to influence pregnancy outcome, except for a risk of preterm delivery for women first hospitalized during pregnancy. Crohn's disease is considered a risk factor for preterm delivery and low birth weight. This risk is similar to that seen in smoking mothers (30). In no case is there a higher risk of congenital abnormalities (31).
References
1. Brodell RT, Mehrabi D. Underlying causes of erythema nodosum. Postgrad Med 2000; 108: 147-9. [ Links ]
2. Requena L, Requena C. Erythema nodosum. Dermatol Online J 2002; 8: 4. [ Links ]
3. Engin G, Acunas B, Acunas G, Tunaci M. Imaging of extrapulmonary tuberculosis. Radiographics 2000; 20: 471-88. [ Links ]
4. Vanhoenacker FM, De Backer AI, Op de Beeck B, Maes M, Van Altena R, Van Beckevoort D, et al. Imaging of gastrointestinal and abdominal tuberculosis. Eur Radiol 2004; 14: 103-15. [ Links ]
5. Boudiaf M, Zidi SH, Soyer P, et al. Tuberculous colitis mimicking Crohns disease: utility of computed tomography in the differentiation. Eur Radiol 1998; 8: 1221-3. [ Links ]
6. Baert F, Knockaert D, Bobbaers H. Bilateral hilar lymphadenopathy associated with Yersinia enterocolitica infection. Clin Infect Dis 1994; 19: 197-8. [ Links ]
7. Storch I, Rosoff L, Katz S. Sarcoidosis and inflammatory bowel disease. J Clin Gastroenterol 2001; 4: 345. [ Links ]
8. Dumot JA, Karim A, Petras RE, Lashner BA. Sarcoidosis presenting as granulomatous colitis. Am J Gastroenterol 1998; 10: 1949-51. [ Links ]
9. Bulger K, O'Riordan M, Purdy S, et al. Gastrointestinal sarcoidosis resembling Crohn's disease. Am J Gastroenterol 1988; 83: 1415-7. [ Links ]
10. Adenis A, Wallaert B, Colombel JF, Cortor A, Marchandise X, Janin A, et al. Intestinal involvement in sarcoidosis. Gastroenterology 1993; 104: 355-6. [ Links ]
11. Clague RB. Sarcoidosis or Crohn's disease? Br Med J 1972; 3: 804. [ Links ]
12. Lee CR, Kim WH, Cho YS, Kim MH, Kim JH, Park IS, Bang D. Colonoscopic findings in intestinal Behçet's disease. Inflamm Bowel Dis 2001; 7: 243-9. [ Links ]
13. Terrin G, Borrelli O, Di Nardo G, Pacchiarotti C, Cucchiara S. A child with aptthae and diarrhoea. Lancet 2002; 359: 316. [ Links ]
14. Kallinowski B, Noldge G, Stiehi A. Crohn's disease with Behçet's syndrome appearance. A case report. Z Gastroenterol 1994; 32: 642-4. [ Links ]
15. Yazici H, Yurdakul S, Hamurydan V. Behçet syndrome. Curr Opin Rheumatol 1999; 11: 53-7. [ Links ]
16. Internacional study group for Behçet's disease. Lancet 1990; 335: 1078-80. [ Links ]
17. Ajubi N, Nossent JC. Panniculitis as the first manifestation of systemic lupus erythematosus: description of two cases. Neth J Med 1993; 42: 25-9. [ Links ]
18. Petrelli EA, Mc Kinley M, Troncale FJ. Ocular manifestations of inflammatory bowel disease. Ann Ophthalmol 1982; 14: 356-60. [ Links ]
19. Levine JB, Lukawski-Trubish D. Extraintestinal considerations in inflammatory bowel disease. Gastroenterol Clin North Am 1995; 24: 633-46. [ Links ]
20. Veloso FT, Carvalho J, Magro F. Immune-related systemic manifestations of inflammatory bowel disease. A prospective study of 792 patients. J Clin Gastroenterol 1996; 23: 29-34. [ Links ]
21. Greenstein AJ, Janowitz HD, Sachar DB. The extraintestinal complications of Crohn's disease and ulcerative colitis. A study of 700 patients. Medicine 1976; 55: 401. [ Links ]
22. Orchard TR, Wordsworth BP, Jewell DP. Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut 1998; 42: 387-91. [ Links ]
23. Juillerat P, Mottet C, Froehlich F, Felley C, Vader JP, Burnand B, et al. Extraintestinal manifestations of Crohn's disease. Digestion 2005; 71: 31-6. [ Links ]
24. Birnie GG, McLeod TI, Watkinson G. Incidence of sulphasalazine-induced male infertility. Gut 1981; 22: 452-5. [ Links ]
25. Toovey S, Hudson E, Hendry WF, Levi AJ. Sulphasalazine and male infertility: reversibility and possible mechanism. Gut 1981; 22: 445-51. [ Links ]
26. Nielsen OH, Andreasson B, Bondesen S, Jarnum S. Pregnancy in ulcerative colitis. Scand J Gastroenterol 1983; 18: 735-42. [ Links ]
27. Rogers RG, Katz VL. Course of Crohn's disease during the pregnancy and its effect on pregnancy outcome: a retrosprective review. Am J Perinatol 1995; 12: 262-4. [ Links ]
28. Fonager K, Sorensen HT, Olsen J. Pregnancy outcome for women with Crohn's disease: a follow-up study based on linkage between national registries. Am J Gastroenterol 1998; 93: 2426-30. [ Links ]
29. Norgard B, Fonager K, Sorensen HT, Olsen J. Birth outcomes of women with ulcerative colitis: a nationwide Danish cohort study. Am J Gastroenterol 2000; 95: 3165-70. [ Links ]
30. Katz J. Pregnancy and inflammatory bowel disease. Curr Opin Gastroenterol 2004; 20: 328-32. [ Links ]
31. Mottet C, Juillerat P, Gonvers J, Froehlich F, Burnand B, Vader J, et al. Pregnancy and Crohn's disease. Digestion 2005; 71: 54-61. [ Links ]
![]() Correspondence:
Correspondence:
Antonio Lalueza Blanco.
Servicio de Medicina Interna.
Hospital Universitario 12 de Octubre.
Avda. de Córdoba, s/n.
28041 Madrid.
e-mail: lalueza@hotmail.com
Recibido: 10-10-05.
Aceptado: 19-10-05.











 texto en
texto en