Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 no.7 Madrid jul. 2006
PICTURES IN DIGESTIVE PATHOLOGY
Massive hepatic amyloidosis with fatal hepatic failure
Amiloidosis hepática masiva con fallo hepático fulminante
E. Ubiña Aznar, N. Fernández Moreno, R. Rivera Irigoin, P. Moreno Mejías, F. Fernández Pérez,
F. Vera Rivero, J. M. Navarro Jarabo, G. García Fernández, C. de Sola Earle,
A. Pérez Aisa and A. Sánchez Cantos
Servicio de Aparato Digestivo y Anatomía Patológica. Hospital Costa del Sol. Marbella. Málaga, Spain
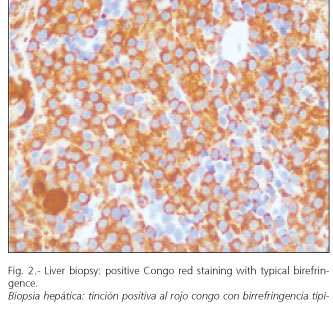
A 55-year-old woman diagnosed with high blood pressure, hypothyroidism, and various vertebral fractures attributed to severe osteopenia was admitted to the hospital with a gastrointestinal bleeding secondary to a benign gastric ulcer. During the examination, attention was drawn to an indolent smooth-surface, hard hepatomegaly associated with severely tender spinous processes in lumbar vertebrae. Laboratory parameters showed normocytic anemia (Hb 8.7 g/dl, VCM 84 fl) with a prothrombin activity of 35% and changes in the liver tests (GGT 588 U/L, AP 231 U/L, normal transaminases and bilirubin). In view of these findings an abdominal ultrasound was obtained, which showed liver enlargement without signs of portal hypertension, but evidences of chronic liver disease with no definite findings. Because of the presence of severe coagulation problems, a transjugular liver biopsy was carried out, and the diagnosis of amyloidosis was reached; later, a bone marrow puncture was performed before the advent of vertebral fractures in the lumbar region. After the diagnosis of primary amyloidosis and plasmocytoma, treatment was begun with high-dose of dexamethasone; however, liver and renal function impaired progressively, the patient developed jaundice and died.
Liver involvement is frequent in systemic amyloidosis, and varies according to different series from 56 to 90% if we exclude familial amyloidosis (1,2). The onset of the disease usually involves a presentation with symptoms secondary to liver dysfunction, including abdominal distension and hepatomegaly. Liver function tests may be abnormal and usually include elevated alkaline phosphatase and GGT. The presence of jaundice and particularly serum bilirubin levels above 5 mg/dl is exceptional and commonly associated with a poor outcome (2). The presence of severe intrahepatic cholestasis at onset is exceptional; thus, Goenka et al. (2) described the existence of only 27 cases, of which 22 died before the sixth month after development of jaundice. The presence of high alkaline phosphatase levels up to 4 times the normal value results in poor prognosis, with a mean survival of 3.3 months since jaundice development (3). Treatment with melphalan and prednisone, together with the assessment of potential liver transplantation are the only therapeutic options.
References
1. Bruguera M. Amiloidosis e hígado. Actualidades en gastroenterología y hepatología. Prous Editores; 1994.
2. Goenka MK, Bhasin DK, Vasisth RK, Dhawan S. Hepatic amyloidosis presenting with severe intrahepatic cholestasis. J Clin Gastroenterol 1996; 23: 134-6.
3. Gertz MA, Kyle Ra. Hepatic amylodidosis [primary (AL), immunoglobulin light chain]: the natural history in 80 patients. Am J Med 1998; 85: 73-80.











 texto en
texto en