Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 no.8 Madrid ago. 2006
CLINICAL NOTE
Pancreatic pseudocyst located in the liver
Pseudoquiste pancreático de localización hepática
I. Les, J. Córdoba, V. Vargas, L. Guarner1,
R. Boyé2 and V. Pineda2
Services of Internal Medicine-Hepatology,
1Gastroenterology and
2Radiology.
Hospital Valle de Hebrón. Universidad Autónoma de Barcelona. Barcelona, Spain
ABSTRACT
Pancreatic pseudocyst is a common complication of acute and chronic pancreatitis. Extrapancreatic locations of pancreatic pseudocyst in the liver, pleura, mediastinum, or pelvis have been described. However, a pancreatic pseudocyst located in the liver is an infrequent condition. We present the case of a 46-year-old man with pancreatic pseudocyst located in the liver secondary to chronic alcoholic pancreatitis. During admission, the patient underwent an abdominal CT scan that showed a mass located in the head and body of the pancreas, as well as a thrombosis of the splenic vein. A percutaneous needle aspiration biopsy of the pancreas was obtained under CT guidance, which showed no tumoral involvement. Fourty-eight hours after the procedure the patient developed abdominal pain and elevated serum amylase levels. A pancreatic MRI exam showed two pancreatic pseudocysts, one of them located in the left hepatic lobe, the other in the pancreatic tail. Chronic pancreatitis signs also were found. Enteral nutrition via a nasojejunal tube was administered for two weeks. The disappearance of the pancreatic pseudocyst located in the pancreatic tail, and a subtotal resolution of the pancreatic pseudocyst located in the liver were observed. To date twenty-seven cases of pancreatic pseudocyst located in the liver have been published, most of them managed with percutaneous or surgical drainage.
Key words: Pancreatic pseudocyst. Acute pancreatitis. Chronic pancreatitis. Hepatic location.
Introduction
A pancreatic pseudocyst is a collection of pancreatic juice located in or around the pancreas. Pancreatic pseudocysts are encased by a non-epithelial lining of fibrous, necrotic and granulation tissue secondary to pancreatic injury. They develop at least four weeks after this damage has occurred. Pancreatic pseudocysts are a complication of both acute and chronic pancreatitis. Most pancreatic pseudocysts are located within the head and the body of the pancreas, but 20% of them are extrapancreatic (1). Several locations of pancreatic pseudocysts, like the pleura, mediastinum and pelvis, have been described (2). We present the case of a pancreatic pseudocyst located in the liver that developed during the reactivation of a chronic pancreatitis, and resolved without need of drainage.
Clinical description
A 46-year-old smoker and chronic alcoholic male who three years ago had suffered from an episode of acute pancreatitis secondary to alcoholic abuse was admitted to hospital for his coffee-ground vomiting and melena. He reported no abdominal pain. His blood pressure was 90/60 mmHg, and he was apyretic. The cardio-respiratory examination revealed tachycardia (120 bpm) without other alterations. No abdominal pain was elicited during exploration, but an enlarged spleen was detected. There were neither hepatomegaly nor peripheric adenopathies. Laboratory tests revealed the following findings: hemoglobin 10 g/dL, MCV 85 fL, leukocytes 4,4 x 109/L, platelets 64 x 109/L. Coagulation, hepatic, and renal tests showed no abnormalities. An electrocardiogram revealed sinusal tachycardia at 120 bpm, without other alterations. Chest and abdomen radiograms were normal. The patient underwent upper endoscopy, which showed a congestive area in the body and the antrum of the stomach. An abdominal ultrasonogram revealed a 18-cm splenomegaly, which was confirmed by an abdominal CT scan. Moreover, the abdominal CT scan revealed the existence of a heterogeneous mass in the retroperitoneum that included the head and body of the pancreas, and which caused thrombosis in the splenic vein (Fig. 1).
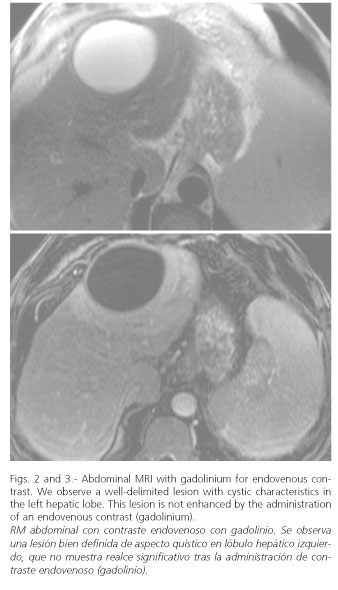
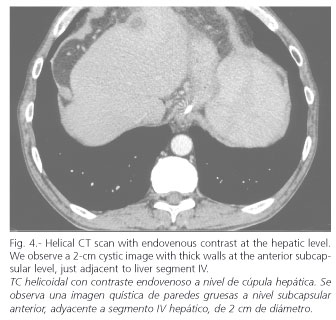
A fine-needle aspiration biopsy with CT guidance was obtained to rule out pancreatic adenocarcinoma. On anatomo-pathologic studies no atypical cells were observed. Fourty-eight hours after the procedure the patient reported continous abdominal pain located in the epigastrium, with nausea and vomiting. An urgent laboratory examination revealed serum amylase levels of 312 IU/L (normal < 53 IU/L). Hemoglobin showed no changes, and the rest of the biochemical work-up were normal, including transaminases. The abdominal CT scan was repeated without significant variations, except for a well-delimited lesion in the tail of the pancreas, 5 x 2 cm in size. This image was consistent with a pancreatic pseudocyst. Fasting and intravenous fluid therapy were initiated. After a few days, an abdominal MRI was performed to better define the features of this pancreatic lesion. The pancreas exhibited a dilated Wirsung's duct and other alterations consistent with chronic pancreatitis. Moreover, the abdominal MRI confirmed the existence of a pancreatic pseudocyst in the tail of the pancreas, and showed another cystic lesion in the left hepatic lobe, 6 x 6.5 cm in size (Fig. 2). We tend to believe that the previous mass detected by the CT scan was an edematous pancreas with peripancreatic exudates, which evolved to peripancreatic and intrahepatic pseudocysts. All of it was consistent with a reactivated chronic alcoholic pancreatitis. At this point, enteral nutrition therapy via a nasojejunal tube was administered. After fourteen days a repeat abdominal CT scan was obtained, which showed a subtotal resolution of the pancreatic pseudocyst located in the liver (Fig. 3) and the disappearance of the pseudocyst in the pancreatic tail. Enteral nutrition was interrupted, and oral ingestion was tolerated by the patient, who was discharged with no symptoms.
Discussion
Pancreatic pseudocyst located in the liver is an uncommon condition. In the literature, twenty-seven cases have been described, twenty-six of which were summarized in a review article (3,4). As in the present case, the majority of liver pancreatic pseudocysts are located in the left hepatic lobe. The proteolytic effect of pancreatic enzymes has been proposed as a pathogenic mechanism. These enzymes promote the formation of pseudocysts in multiple locations, including the liver, pleura, mediastinum, and retroperitoneum (5). The hepato-duodenal ligament has been proposed as a way for spreading between the pancreas and the liver (6). In our case, some days prior to the diagnosis of pancreatic pseudocyst, a fine-needle aspiration biopsy had been performed. A puncture through the liver may open a tract between these two organs. However, the procedure was not performed through the hepatic parenchyma, so we rule out this cause.
Pancreatic pseudocyst located in the liver must to be included in the differential diagnosis of liver cystic lesions (7,8), like neoplasms. A pancreatic pseudocyst located in the liver cause no specific symptoms, and is incidentally diagnosed by the identification of a liver cystic lesion during acute pancreatitis. Liver studies are usually normal, with no transaminase increase. Exceptionally, a pancreatic pseudocyst located in the liver can produce hepatomegaly, jaundice or an abdominal palpable mass (9). An easy confirmation may be obtained by amylase levels in the contents of the pseudocyst (10). In our case this was not necessary because clinical manifestations left no doubts, and the cyst had an early resolution.
Almost every pancreatic pseudocyst improves spontaneously and needs no specific treatment (11,12). Draining is mandatory when symptoms secondary to compression of adjacent organs are found. It is also necessary to act when the following complications develop: rupture, infection, or bleeding. Depending on the complexity of the pseudocyst, its communication with Wirsung's duct, and the existence of ductal injury, we may perform a percutaneous, endoscopic or surgical drainage. Only the last procedure is definitive.
The majority of published pancreatic pseudocysts located in the liver were treated with percutaneous or surgical drainage. Only in two of the nineteen described treatments the pseudocyst resolved spontaneously with no need for drainage or surgery (3). Criteria to drain a pancreatic pseudocyst located in the liver have not been established. Almost all surgical patients were treated in times when radiology had a lower accuracy, and when percutaneous drainages were not available. Percutaneous drainage was promoted because it allows diagnosis confirmation and treatment (10). Nevertheless, in agreement with the new trends, we propose an initial expectant attitude if the diagnosis is clear, thus restricting percutaneous drainage for symptomatic and complicated cases.
In conclusion, we present the case of a patient with reactivated chronic alcoholic pancreatitis, complicated with thrombosis of the splenic vein. In his evolution, he first developed multiple peripancreatic exudates, and then two pancreatic pseudocysts located in the tail of the pancreas and liver. These lesions disappeared after conservative management and enteral nutrition via a nasojejunal tube.
References
1. Hamm VB, Franzen N. Atypically located pancreatic pseudocyst in liver, spleen, stomach wall and mediastinum: their CT diagnosis. Rofo 1993; 159 (6): 522-7. [ Links ]
2. Vitas GJ, Sarr MG. Selected management of pancreatic pseudocyst: Operative versus expectant management. Surgery 1992; 111 (2): 123-30. [ Links ]
3. Mofredj A, Cadranel JF, Dautreaux M, Kazerouni F, Hadj-Nacer K, Deplaix P, et al. Pancreatic pseudocyst located in the liver: a case report and literature review. J Clin Gastroenterol 2000; 30 (1): 81-3. [ Links ]
4. Balzan S, Kianmanesh R, Farges O, Sauvanet A, O'toole D, Levy P, et al. Right intrahepatic pseudocyst following acute pancreatitis: an unusual location after acute pancreatitis. J Hepatobiliary Pancreat Surg 2005; 12 (2): 135-7. [ Links ]
5. Baranyai Z, Jakab F. Pancreatic pseudocyst propagating into retroperitoneum and mediastinum. Acta Chir Hung 1997; 36 (1-4): 16-7. [ Links ]
6. Shibasaki M, Bandai Y, Ukai T. Pancreatic pseudocyst extending into the liver via hepatoduodenal ligament: a case report. Hepatogastroenetrology 2002; 49 (48): 1719-21. [ Links ]
7. Pelletier G. Diagnosis of cystic lesions of the liver. Ann Chir 1997; 51 (3): 267-71. [ Links ]
8. Mortele KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics 2001; 21 (4): 895-910. [ Links ]
9. Aguilera V, Mora J, Sala T, Martínez F, Palau A, Bastida G, et al. Endoscopic treatment of pancreatitis and its complications. Gastroenterol Hepatol 2003; 26 (1): 13-8. [ Links ]
10. Polakow J, Serwatka W, Dobrzycki S, Ladny JR, Janica J, Puchalski Z. A new diagnostic approach to pancreatic pseudocyst fine-needle puncture: three dimensional sonography. J Hepatobiliary Pancreat Surg 2004; 11 (3): 159-63. [ Links ]
11. Cheruvu CV, Clarke MG, Prentice M, Eyre-Brook IA. Conservative treatment as an option in the management of pancreatic pseudocyst. Ann R Coll Surg Engl 2003; 85 (5): 313-6. [ Links ]
12. Andren-Sandberg A, Ansorge C, Eiriksson K, Glomsaker T, Maleckas A. Treatment of pancreatic pseudocyts. Scand J Surg 2005; 94 (2): 165-75. [ Links ]
![]() Correspondence:
Correspondence:
Íñigo Les.
Servicio de Medicina Interna-Hepatología.
Hospital Valle de Hebrón.
Paseo Valle Hebrón, 119.
08035 Barcelona.
Fax: 932 746 068.
E-mail: iles@arrakis.es
Recibido: 06-03-06
Aceptado: 09-03-06











 texto en
texto en