My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.98 n.11 Madrid Nov. 2006
ORIGINAL PAPERS
Complete rectal prolapse clinical and functional outcome with Delorme's procedure
Prolapso rectal completo. Resultados clínicos y funcionales con la operación de Delorme
J. A. Pascual Montero1,2, M. C. Martínez Puente2,
I. Pascual2, T. Butrón Vila1, F. J. García Borda1,2,
M. Lomas Espadas1 and M. Hidalgo Pascual1
1Service of Gastrointestinal Surgery. Hospital 12 de Octubre. 2Coloproctology Unit. Clínica Centro. Madrid, Spain
ABSTRACT
Introduction: many surgical techniques -both through the perineal and abdominal routes- have been described for the treatment of rectal prolapse. The aim of this work is to evaluate the clinical and functional outcome with Delorme's perineal procedure.
Patients and methods: twenty-one patients with complete rectal prolapse were studied from July 2000 to October 2005. Age, gender, anesthetic risk, and accompanying symptoms were all assessed. Diagnostic tests performed included: colonoscopy, anorectal manometry before and after surgery, and 360° endoanal ultrasonography. Delorme's procedures were carried out by only one surgical team.
Results: no mortality occurred, and morbidity was minimal. Prolapse relapse rate was 9.52% with a mean follow-up of 34 months. Anal continence improved in 87.5% of patients, and no surgery-associated constipation ensued. Mean hospital stay was 2 (range 1-4) days. During the postoperative period no pain developed in 17 patients, and 4 patients had mild pain. Satisfaction with surgery was high in 16 cases (76.19%), moderate in 3 (14.28%), and low in 2 (9.52%).
Conclusions: Delorme's procedure for the management of complete rectal prolapse is associated with low morbidity, improves anal continence, gives rise to no postsurgical constipation, and has an acceptable relapse rate. Patient satisfaction with this procedure is high because of its high comfortability (intradural anesthesia, short hospital stay, and little postoperative pain) and optimal results.
Key words: Rectal prolapse. Delorme's procedure. Fecal incontinence.
Introduction
Complete rectal prolapse is the rectum's protrusion with all its layers through the anal orifice. It has a higher incidence in advanced age, and is frequently associated with anal incontinence difficulties (in 50-70% of cases) and -on occasion- constipation (1,2). Many procedures for the management of this condition have been described, both through the abdominal and perineal routes. Most such surgical techniques are successful regarding the prolapse, but either do not solve or even worsen defecation obstruction and incontinence concerns (1,3,4).
Delorme's procedure for the surgical treatment of complete rectal prolapse was first described by the French military surgeon Edmond Delorme in 1900 (3). This is a procedure through the perineal route consisting of rectal muscle layer plication and mucosal layer resection. The technique has been recently revitalized despite the fact that its associated relapse rate (5-22%) is higher than that of abdominal procedures (0-10%) (1,3).
The aim of this work is to evaluate clinical and functional outcome with Delorme's procedure for the management of complete rectal prolapse.
Patients and method
A total of 21 patients (19 females, 2 males) with complete rectal prolapse were studied from July 2000 to October 2005. Mean age was 59 (range 24-84) years. Of all 21 patients, 18 (85.71%) had an ASA (American Society of Anesthesiologists) II or higher risk. Rectal prolapse was primary for 20 cases, and relapsing for 1 (the previous procedure had been an abdominal rectopexy using a polypropylene mesh).
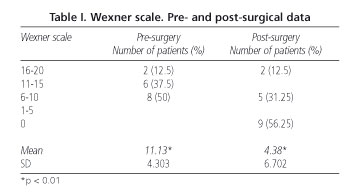
Prolapse-associated symptoms included (in order of frequency): mucous secretion from the anus in association with stinging and pruritus in all patients, anal incontinence in 16 patients (76.19%), rectorrhagia in 15 (71.42%), constipation in 5 (23.80%), and tenesmus in 1 (4.76%). Anal incontinence was evaluated using a Wexner scale (5) both before and 6 months after surgery.
The following diagnostic tests were performed: preoperative colonoscopy in all cases, anorectal manometry before and after surgery in 16 patients with incontinence, and 360º endoanal ultrasonography in 8. The anorectal manometry device used was a pressure system including a graduated polyvinyl probe with a latex microballoon on one end, coupled with an external transducer connected to a recording device (GAELTEC, Dunvegan, Isle of Skye. Scotland). Maximum pressure at rest (MPR), maximum pressure at voluntary contraction (MPVC), and sphincter length were all measured using a station pull-through technique. The presence of rectoanal inhibitory reflex (RAIR), and maximum tolerated volume were also assessed.
The procedure was in all patients performed by the same surgical team, which was mainly devoted to colorectal surgery. The bowel was cleaned using a balanced polyethylenglycol solution, and antimicrobial prophylaxis with metronidazole and gentamycin -without antithrombotic prophylaxis- was applied. Intradural anesthesia (saddle block) plus sedation was used for all patients. A lithotomy position was adopted in 19 cases, and prone jack-knife decubitus in the remainder patients. Surgical technique was as follows: with a completely prolapsed rectum (Fig. 1) 1: 200,000 epinephrine was injected into the submucosal plane above the dentate line. A circular incision was performed using an electric scalpel through the mucosal and submucosal layers 1 cm above the dentate line, and a sleeve was dissected -which revealed the rectum's circular muscular layer- to the prolapse's vertex (Fig. 2). A 6 to 8-stitch (polyglactyn 00) longitudinal suture was applied to plicate the rectal musculature in order to reduce and invaginate it (Fig. 3). Once the dissected mucosa was excised the procedure was ended with a loose-stitch (polyglactyn 00) from the proximal to the distal mucosa just above the dentate line. After surgery, oral metamizole and diclofenac were used in standard doses for analgesia during the first 3 preoperative days, and pain extent was measured using a numeric scale from 0 (no pain) to 10 (the worst pain possible).
Follow up was carried out by means of outpatient visits at months 1, 2, 3, 6 and 12, and the once a year. Patients were asked for their extent of satisfaction with surgery -high, moderate, or low.
A statistical analysis was performed to compare Wexner scale values to manometric parameters both before and after surgery. A repeat measurement ANOVA was carried out using the SPSS software package. Statistical significance was considered for p < 0.05.
Results
The results from the preoperative study were as follows: colonoscopy ruled out associated organ pathology for all cases. In 14 of 16 cases with incontinence undergoing anorectal manometry, sphincter hypotonia was found regarding both pressure at rest and pressure at voluntary contraction, and 6 of 8 patients with endoanal ultrasonography showed open puborectal bundles and substitution signs in the internal anal sphincter. Ultrasonography revealed no significant disturbances in the remaining two patients.
Mean surgery duration was 71 (range 60-100) minutes. Mean excised sleeve size (as measured following phormol fixation) was 7.18 (range 5-11) cm.
After surgery oral ingestion was restored at 15 hours on average (range 6-24), and using the aforementioned analgesia 17 patients developed no pain, and 4 had mild pain (1-3 in the pain scale). No deaths occurred, and the only complication encountered was a case of preoperative bleeding at day 10 after surgery, which subsided spontaneously. Mean hospital stay was 2 days (range 1-4).
Mean patient follow-up was 34 months (range 7-63). Two patients had a relapsing prolapse during follow-up (9.52%). In both cases relapse occurred early postoperatively (within 3 months of surgery), and these patients were reoperated using the same Delorme's technique, with satisfatory results in one patient and partial improvement in the other subject at 24 months after reintervention. A patient developed suture stenosis, which was resolved with digital rectal maneuvers.
Anal continence improved in 14 of 16 patients with previous incontinence. Data regarding improvement as measured by a Wexner scale are listed in table I. Differences were statistically significant (p < 0.01). Following surgery, the maximum pressure at rest and maximum pressure at voluntary contraction significantly improved (p = 0.03 and p < 0.01, respectively). Maximum tolerated volume significantly decreased (p < 0.01). Anorectal manometry data before and after surgery are listed in table II. Reactoanal inhibitory reflex (RAIR) was normal in 12 patients, and absent in 4. No RAIR changes occurred after surgery.
Four of 5 previously constipated patients had still constipation after surgery.
Satisfaction with surgery was high in 16 cases (76.19%), moderate in 3 cases (14.28%), and low in 2 cases (9.52%).
DISCUSSION
Many procedures have been described for complete rectal prolapse both through the abdominal and perineal routes. The primary advantages of Delorme's procedure versus abdominal techniques for the management of rectal prolapse include low morbidity and mortality (1,6-8). Using a perineal route no risk of impotence is run, in contrast with abdominal rectopexy where pelvic nerves (erection problems) or hypogastric nerves (ejaculation problems) may be damaged (1,3). Because of this, this procedure is -according to some authors- of choice for young and adult males (only two males were included in our series, though). Furthermore, a perineal approach may be attempted with intradural anesthesia, and is also most indicated for patients at high surgical risk. In our series most patients were ASA II or higher. This aspect is of utmost importance since -as previously discussed- prolapse is a condition with a high incidence in older women. This technique is also associated with short hospital stay, early oral feeding resumption (relevant for patients with associated conditions), and patient comfort, with little or no postoperative pain. Thus, Delorme's procedure may be recommended both for young and adult males to prevent potential impotence (3) and weakened or elderly patients. The literature also describes that Delorme's procedure may be indicated as emergency surgery for strangulated rectal prolapse with satisfactory results (9).
However, the procedure most commonly performed in the management of rectal prolapse is abdominal rectopexy according to the literature, with a relapse rate of 0-10% (1). This is its greater advantage over Delorme's procedure, which in most recent series shows a relapse rate of 5-22% (1,6,7). Our series falls within this range (9.52%). A possible explanation of rectal prolapse relapse when a perineal route is used is technical in nature, as mucosectomy all along the prolapse's length is very important. At least in our series, this could be the cause for our two relapsing cases, as these were the first patients operated on and we believe that mucosectomy did not ultimately reach the prolapse's apex. Some authors extend resection to both mucosal cylinders -inner and outer- in the prolapse (8,10). Most authors believe that Delorme's procedure may be repeated for failed first attempts (2,11). We reoperated our two patients with early relapse using the same Delorme's technique with satisfactory results in one case.
Several aspects are of utmost importance for relapsed prolapse prevention and incontinence improvement. First is an initial incision at one centimeter above the dentate line, to preserve anorectal sensory area. Also a mucosal and submucosal dissection along the whole prolapse, which allows a subsequent plication of the underlying circular muscle layer (2). Another relevant technical detail, a modification of Delorme's original procedure, is submucosal infiltration with epinephrine, which facilitates dissection and reduces blood loss (10).
Voiding difficulties and constipation following abdominal procedures occur in 27-47% of patients (1). Rectal denervation is probably an important factor in the etiology of defecatory problems. The sectioning of lateral ligaments as in abdominal procedures entails a high incidence of constipation. However, these ligaments are not sectioned with Delorme's perineal technique, and this prevents constipation from developing; constipation may even improve after surgery according to a number of series (1,6). In our series no constipation developed postoperatively, and previously constipated patients did not get worse. For other authors constipation improvement may result from reduced rectal compliance after surgery, which explains the increase in defecatory frequency. Also rectal mucosectomy may exert a significant effect on proximal colonic motility, with a higher frequency of rectal filling and hence improved constipation (3). It is for these reasons that Delorme's procedure -or a previous modification- has been recommended for the management of constipation associated with internal rectal intussusception (12-14).
Continence often improves after prolapse repair regardless of the technique used: 38-100% of patients improve after rectopexy, and more than 83% improve after Delorme's operation (1). In our series continence improved in 87.5% of cases. A case where continence remained unchanged was a female patient of advanced age who had suffered from severe incontinence before prolapse development, and had a previous postanal repair with no satisfactory functional results. Continence improvement after prolapse surgery may also result from increased pressure at rest, as this parameter is previously reduced in most patients with rectal prolapse (15). Results regarding increased anal pressures (both at rest and at voluntary contraction) are inconsistent across series (1). In some series -as in ours- both parameters increase (1), but sphincter pressures remain unchanged in other series (3,4). Some authors suggest that improved rectal sensation may be the cause of improved continence despite decreased rectal compliance (4).
To conclude, Delorme's procedure is a perineal technique that solves rectal prolapse with a low surgical risk and little morbidity. The procedure is associated with a marked improvement in anal continence, relapse rates are relatively low, and patient satisfaction is high.
References
1. Tsunoda A, Yasuda N, Yokoyama N, Kamiyana G, Kusano M. Delorme's procedure for rectal prolapse. Clinical and physiological analysis. Dis Colon Rectum 2003; 46: 1260-5. [ Links ]
2. Tobin SA, Scott IHK. Delorme procedure for rectal prolapse. Br J Surg 1994; 81: 1681-4. [ Links ]
3. Watts AMI, Thompson MR. Evaluation of Delorme's procedure as a treatment for full-thickness rectal prolapse. Br J Surg 2000; 87: 218-22. [ Links ]
4. Plusa SM, Charig JA, Balaji A, Watts A, Thompson MR. Physiological changes after Delorme's procedure for full-thickness rectal prolapse. Br J Surg 1995; 82: 1475-8. [ Links ]
5. Jorge M, Wexner S. Etiology and management of fecal incontinence. Dis Colon Rectum 1993; 36 (1): 77-97. [ Links ]
6. Senapati A, Nicholls RJ, Thomson JP, Phillips RK. Results of Delorme's procedure for rectal prolpase. Dis Colon Rectum 1994; 37 (5): 456-60. [ Links ]
7. Watkins BP, Landercasper J, Blezer GE, Rechner P, Knudson R, Bintz M, et al. Long-term follow-up of the modified Delorme procedure for rectal prolapse. Arch Surg 2003; 138 (5): 498-502; discusión 502-3. [ Links ]
8. Palma F. Nobleza de la operación de Delorme en el tratamiento del prolapso rectal. Indicaciones y resultados. Rev Esp Enferm Dig 1989; 76 (6-I): 585-8. [ Links ]
9. Jordán JC, Fernández C, Díaz F, Alós R, Buch E, Roig JV. Operación de Delorme en un caso de prolapso rectal estrangulado. Cir Esp 1999; 66: 339-40. [ Links ]
10. Oliver GC, Vachon D, Eisenstat TE, Rubin RJ, Salvati EP. Delorme's procedure for complete rectal prolapse in severely debilitated patients. An analysis of 41 cases. Dis Colon Rectum 1994; 37: 461-7. [ Links ]
11. Pikarsky AJ, Joo AS, Wexner SD, Weiss EG, Nogueras JJ, Agachan F, et al. Recurrent rectal prolapse. What is the next good option? Dis Colon Rectum 2000; 43: 1273-6. [ Links ]
12. Sielezneff I, Malouf A, Cesari J, Brunet C, Sarles JC, Sastre B. Selection criteria for internal retal prolapse repair by Delorme's transrectal escisión. Dis Colon Rectum 1999; 42 (3): 367-73. [ Links ]
13. Dippolito A, Esser A, Reed J. Anterior modification of Delorme procedure provides equivalent results to Delorme procedure in treatment of rectal outlet obstruction. Curr Surg 2005; 62 (6): 609-12. [ Links ]
14. Velasco FJ, López R, Pujol J, Sancho F, Llaurado JM, Lluis F, et al. The use of anorectal manometry and dynamic proctography in patients for diagnosis of solitary rectal ulcer syndrome. Rev Esp Enferm Dig 1998; 90 (6): 454-8. [ Links ]
15. Roig JV, Buch E, Alos R, Solana A, Fernández C, Villoslada C, et al. Anorectal function in patients with complete rectal prolapse. Differences between continent and incontinent individuals. Rev Esp Enferm Dig 1998; 90 (11): 794-805. [ Links ]
![]() Correspondence to:
Correspondence to:
José Antonio Pascual Montero.
C/Ventisqiero de la Condesa, 42.
28035 Madrid.
Tele-Fax: 917 340 011
E-mail: pepasmon@hotmail.com
Recibido: 09-06-06
Aceptado: 07-09-06.