Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.99 no.6 Madrid Jun. 2007
CARTAS AL DIRECTOR
Dysphagia aortica: A diagnostic challenge in the elderly
Disfagia aórtica: un reto diagnóstico en el paciente de edad avanzada
Palabras clave: Disfagia aórtica. Retos diagnósticos. Edad avanzada.
Key words: Dysphagia aortica. Diagnostic difficulties. Elderly.
To the Editor:
Dysphagia aortica is a difficulty in swallowing, caused by extrinsic compression of the esophagus due to an ectatic, tortuous, or aneurysmatic atherosclerotic thoracic aorta. This condition is very uncommon (1), and is usually associated with old age, women of short stature, hypertension, and kyphosis (2,3). Occasionally, diagnostic challenge may appear such as this report illustrates.
A 75-year-old woman presented with a seven month history of progressive dysphagia to solids and liquids with concomitant 5 kg weight loss. Her medical history included hypertension, hypertrophic non-obstructive cardiomyopathy, and an arteriosclerotic aneurysm of ascending aorta repaired fifteen months before.
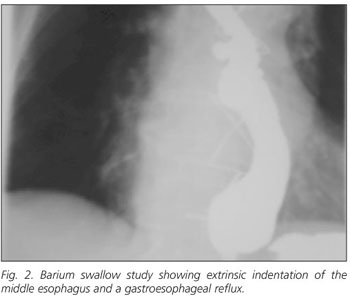
Physical examination showed a systolic ejection murmur at the right upper sternal border. Her height was 1.49 m. Her chest radiograph revealed an enlargement of the aortic arch and kyphosis (Fig. 1). An esophagogastroduodenoscopy showed an extrinsic compression at middle esophagus. An upper gastrointestinal barium study confirmed previous finding showing, also, a gastroesophageal reflux with no hiatal hernia (Fig. 2). Computed tomography (CT) scann of the chest showed an ectasic and enlarged thoracic aorta with following diameter in cm: ascending (3.8 x 3.6); arch (3.9 x 3.9); and descending (4 x 4) where an intramural thrombus and parietal fissure were seen (Fig. 3). These findings suggested a dysphagia aortica with an unstable aortic aneurysm. The patient was transferred to the department of Cardiovascular Surgery. An endovascular prosthesis from aortic arch to hiatus was placed. In addition, her diet was modified. Outcome: although the patient had a moderate symptomatic relief, dysphagia to solids was present 6 months later.
There is no a "gold standard" diagnostic procedure for dysphagia aortica. The association of suggestive symptoms, such as progressive intolerance to solids with concomitant weight loss, with the results of imaging and other diagnostic studies provide a high index of suspicion (4). The diagnostic work-up includes (usual findings) standard chest radiography (enlargement of aortic arch and tortuous dilated aorta); chest CT scann (dilated thoracic aorta); endoscopy (pulsatile extrinsic compression, stenosis of the lower esophagus with proximal dilatation); barium swallow test (partial esophageal obstruction, pulsatile movement synchronous with aortic pulsation), and manometry (localised high pressure band with superimposed pulsation synchronous with the cardiac cycle).
Differential diagnosis of dysphagia aortica includes various common structural and neuromuscular abnormalities. Dysphagia aortica is frequently seen with gastroesophageal reflux disease and motility disorders, both common causes of dysphagia (2). The coexistence of these conditions and the lack of sensitivity and specificity of usual diagnostic methods difficult to make the diagnosis of dysphagia aortica with certainty. So, the classical findings for dysphagia aortica are inconstant and subjective. Radiographic and, or endoscopic findings may be minimal or absent. False negative results are not rare in barium swallow study. Tortuosity of the thoracic aorta is a frequent radiological finding in older people with dysphagia. CT scann may occasionally be of no value in assessing compression of the esophagus by the aorta (2). Vascular pulsation appears commonly on endoscopy of the normal esophagus. Also manometric features suggestive of dysphagia aortica occur in normal patients with no dysphagia (5). Thus, to exclude a motility disorder as the cause of dysphagia in this clinical setting, a structural compression at the same level as manometric findings may be required (2).
In patients with dysphagia aortica and severe symptoms, surgery may be appropriate. However, symptoms are usually mild or moderate. This clinical setting associated with old age and frequent comorbidity require a conservative management, modifying diet to soft or liquid (2-4).
Presence of gastroesophageal reflux disease in this patient may explain her dysphagia better than compression by aneurysmatic aorta, and why the endovascular aortic repair did not resulted in resolution of the dysphagia. In addition, partial relief of dysphagia may be attributed to the modified diet.
In conclusion, the association between aortic aneurysm and dysphagia in the elderly is not ever synonymous of causal relationship.
E. Antón
Department of Internal Medicine. Zumárraga Hospital. Zumárraga. Guipúzcoa, Spain
References
1. Taylor CW, Sinha A, Nightingale JMD. Dysphagia and thoracoabdominal aneurysm. Postgrad Med J 2001; 77: 257-8.
2. Wilkinson JM, Euinton HA, Smith LF, Bull MJ, Thorpe JAC. Diagnostic dilemma in dysphagia aortica. Eur J Cardiothorac Surg 1997; 11: 222-7.
3. Ponce J, Gaspar E, Del Val A, Garrigues V, Sancho MJ, Carrasquer J. Vascular dysphagia. Rev Esp Enferm Dig 1991; 80: 53-6.
4. Hilliard AA, Murali N, Keller AS. Dysphagia aortica. Ann Intern Med 2005; 142: 230-1.
5. Mittal RK, Siskind BN, Hongo M, Flye MW, McCallum RW. Dysphagia aortica. Clinical, radiological and manometric findings. Dig Dis Sci 1986; 31: 379-84.