Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.99 no.9 Madrid sep. 2007
IMÁGENES EN PATOLOGÍA DIGESTIVA
Intrahepatic arteriovenous fistula resulting from needle biopsy
Fístula arteriovenosa intrahepática a consecuencia de una biopsia con aguja
I. M. Méndez Sánchez, J. M. Navarro Jarabo, E. Ubiña Aznar, F. M. Vera Rivero, R. Rivera Irigoin, N. Fernández Moreno, F. Fernández Pérez, G. García Fernández, A. Pérez Aisa, C. Albandea Moreno and V. M. Aguilar Urbano
Service of Gastroenterolgy. Hospital Costa de Sol. Marbella. Malaga, Spain
Clinical case
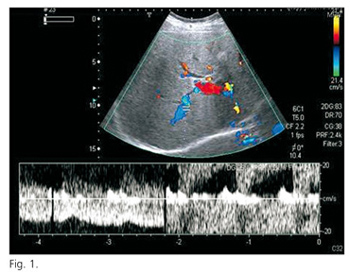
A 38-year-old male patient with HVC-related chronic liver disease refered to our Unit for percutaneous liver biopsy. Physical exam, hemogram and coagulation tests were unremarkable. Two hours after the procedure he refered an intense epigastric pain irradiated to right upper quadrant with nausea. Abdominal palpation revealed deep pain in right upper quadrant without peritoneal signs. Chest and plain abdominal X-ray did not show pneumothorax neither pneumoperitoneum, and blood tests evidenced no changes in hemoglobine concentration. Abdominal ultrasound showed an intravesicular clot without bile duct dilation or intraperitoneal free liquid. Pain killer were given to the patient with a significative improvement. Before hospital discharge the patient developed slight scleral jaundice but no other complications. On follow-up there were no new complications and jaundice solved spontaneously. Two years after the complication, an abdominal ultrasound revealed a right hepatic lobe tubular vascular image with a turbulent flow by doppler with no abnormalities in hepatic veins neither portal vein blood flow (Fig. 1). A trifasic-CT scan evidenced a prompt arterial filling of such vascular tract that depended upon the right branch of the hepatic artery with a contrast-media captation in the surrounding parenchyma (Fig. 2).
Discussion
Liver biopsy is safe when performed by experienced operators. The mortality rate following percutaneous liver biopsy is approximately 1 in 10.000 to 12.000 (1). Sixty percent of complications occur within two hours of the procedure and 96% within 24 hours. Complications after percutaneous liver biopsy can be classified as minor or mayor. Minor complications include transient localized discomfort at the biopsy site, pain sufficient to require analgesia, and mild transient hypotension. Significant intraperitoneal hemorrhage is the most serious bleeding complication of liver biopsy (2).
Postbiopsy arterioportal fistula was first described by Preger in 1967 (3). In the portal tract, the three vessel systems exist in close proximity (4). An arterioportal fistula occurs when liver biopsy produces an abnormal comunication between the hepatic artery an the portal vein (5). Okuda et al. demonstrated on celiac angiograms in 5.4% fistula arteriovenous intrahepatic in 93 patients having had needle biopsy previously but no other transhepatic procedure.
There are different degrees of arterioportal fistula, with most cases being transient and asyntomatic probability attributable to the peripheral formation of the fistula. An extrahepatic arterioportal fistula shunt produces portal hypertension wich may cause severe complications. A communication between a larga intrahepatic artery and porta branch can similarly cause portal hypertension (4).
Systemic arteriovenous fistula seldom close spontaneously, a small intrahepatic fistula may sea itself (4,5) and persistent arterioportal fistulas are considered to be relatively rare.
Angiography has been the gold standard for the diagnosis, but the color Doppler sonography is more suitable for the detection of an arterioportal fistula.
Asyntomatic fistula need not be treated, but the presence of an arterioportal fistula provokes other problems, should be repaired (5). Although hepatic artery ligation has been utilized, the results are not always satisfactory. For fistula deep within the liver, hepatic resection is the best procedure. Large intrahepatic fistula are more likely to result in complications from portal hypertension and are less likely to heal (6).
In this case, fistula was not suspected clinically and was discovered incidentally at the time of color Doppler sonography. Our patient never had evidence of portal hypertension.
References
1. McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology 1990; 99(5): 1396-400.
2. Piccinino F, Sagnelli E, Pasquale G, Giusti G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 1986; 2(2): 165-73.
3. Preger L. Hepatic arteriovenous fistula after percutaneous liver biopsy. Am J Roentgenol Radium Ther Nucl Med 1967; 101(3): 619-20.
4. Okuda K, Musha H, Nakajima Y, Takayasu K, Suzuki Y, Morita M, et al. Frequency of intrahepatic arteriovenous fistula as a sequela to percutaneous needle puncture of the liver. Gastroenterology 1978; 74(6): 1204-7.
5. Sato M, Ishida H, Konno K, Komatsuda T, HamashimaY, Naganuma H, et al. Longstanding arterioportal fistula after laparoscopic liver biopsy. Abdom Imaging 1999; 24(4): 383-5.
6. Foley WJ, Turcotte JG, Hoskins PA, Brant RL, Ause RG. Intrahepatic arteriovenous fistulas between the hepatic artery and portal vein. Ann Surg 1971; 174(5): 849-55.