Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.100 no.4 Madrid abr. 2008
PICTURES IN DIGESTIVE PATHOLOGY
Endoscopic ultrasound for cholangiocarcinoma re-evaluation after Wallstent® placement
Ecografía endoscópica en la reevaluación de un colangiocarcinoma tras la colocación de una prótesis Wallstent®
J. Iglesias-García, J. Lariño-Noia, S. Seijo-Ríos and J. E. Domínguez-Muñoz
Gastroenterology Department. Foundation for Research in Digestive Diseases (FIENAD). University Hospital of Santiago de Compostela. A Coruña. Spain
Together with methods as magnetic resonance imaging (MRI) cholangiography and endoscopic retrograde cholangiography (ERC), endoscopic ultrasound (EUS) readily visualizes common bile duct (CBD) and allows the diagnosis of bile duct masses or strictures (1). Once a Wallstent® has been placed, re-evaluation of the bile duct and stent patency may be difficult. We present the case of a patient with a Klastkin tumor to show the utility of EUS in this setting.
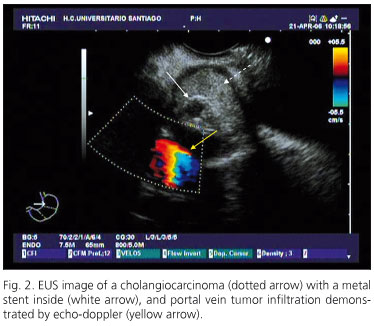
A 55 year old male, smoker, with medical history of ischemic heart disease and atrial fibrillation, was first admitted to our hospital because of jaundice. The diagnosis of Klastkin tumor IIIA-IV was established based on contrast-enhanced computed tomography (CECT) and ERC. The tumor was considered to be not resectable due to relevant portal infiltration. An uncovered biliary Wallstent¬reg; was placed endoscopically for palliation of jaundice and a palliative chemotherapy with oxaliplatin and gemcitabine was administered. Eighteen months later the patient was admitted again because of jaundice relapse and the suspicion of biliary Wallstent® obstruction due to tumor growth. The exact cause of jaundice could not be demonstrated by CECT, and the obstruction of the Wallstent® could only be suspected. MRI cholangiography provided no further information because of stent-related artifacts, whereas ERC was only able to show complete stop at the very distal portion of the stent. On the contrary, lineal EUS (PENTAX FG-3830UT) precisely revealed the growth of the tumor inside the Wallstent® lumen as the cause of biliary obstruction (Fig. 1). The infiltration of the portal vein could also be confirmed during the procedure (Fig. 2). Finally, a palliative EUS-guided transgastric biliary drainage was placed during the same procedure.
Several imaging techniques are used in clinical practice for bile duct evaluation, among them MRI cholangiography, CT scan, ERC and EUS (2). In this context, EUS has proved to be a useful diagnostic tool in patients with obstructive jaundice, as it does not only allow a clear visualization of the neoplasia, but also an accurate local tumor staging (3-5). In a recent study comparing ERC, MRI cholangiography, CT and EUS for evaluation of biliary strictures, Rosch et al. (6) demonstrated the highest diagnostic accuracy for MRI associated with EUS. This supports the previous statement of an international panel of experts regarding the major role of EUS for the diagnosis and staging of biliary tumors in clinical practice (7).
The problem arises when re-evaluation of biliary tumors is required once a metal stent has been placed. Actually, the scientific evidence to this respect is scarce. MRI and CT scan have a limited accuracy in cases of small tumors (8,9). In addition, the metal stent-related MRI artifacts are well known (10). ERC requires some stent patency to evaluate the length of the biliary obstruction and the proximal segments of the biliary tree, as well as to place a new stent for palliation of jaundice. However, a complete obstruction of the bile duct is not an unusual finding, as it is the case of the patient here presented.
Despite the high accuracy of EUS for the primary diagnosis and staging of biliary tumors (3-7), the role of this technique for tumor re-evaluation after metal stent placement is far to be established. The presence of a metal stent may limit to some extent EUS examination, which may lead to tumor understaging (11). Nevertheless, EUS may provide with useful diagnostic information and therapeutic options, as supported by the present case report.
We report the case of a patient with bile duct obstruction due to an unresectable Klastkin tumor, who presented with jaundice relapse 18 months after endoscopic placement of a Wallstent® Due to stent-related artifacts, MRI and CT scan were unable to provide with useful information in this setting, whereas ERC was unsuccessful due to complete obstruction at the distal tip of the stent. EUS was the only technique allowing us to precisely know the cause and extent of the bile duct obstruction. Actually, EUS was able to demonstrate clearly the presence and magnitude of tumor growth inside the stent as the cause of jaundice relapse. In addition, EUS confirmed the advanced tumor stage with portal vein infiltration, and allowed palliative insertion of a transgastric EUS-guided biliary stent.
In conclusion, EUS should be considered for the evaluation of biliary tumors even after insertion of a metal stent. It may not only allow for accurate re-staging of the tumor, but it also offers an alternative for palliative therapy.
References
1. Tio TL, Cheng J, Wijers OB, Sars PR, Tytgat GN. Endosonographic TNM staging of extrahepatic bile duct cancer: Comparison with pathological staging. Gastroenterology 1991; 100: 1351-61. [ Links ]
2. Lazaridis KN, Gores GJ. Cholangiocarcinoma. Gastroenterology 2005; 128: 1655-67. [ Links ]
3. Dancygier GH, Naterman C. The role of endoscopic ultrasonography in biliary tract disease: Obstructive jaundice. Endoscopy 1994; 26: 800-2. [ Links ]
4. Songour Y, Temucin G, Sahin B. Endoscopic ultrasonography in the evaluation of dilated common bile duct. J Clin Gastroenterol 2001; 33: 302-5. [ Links ]
5. Mukai H, Nakajima M, Yasuda K, Mizuno S, Kawai K. Evaluation of endoscopic ultrasonography in the preoperative staging of carcinoma of the ampulla of Vater and common bile duct. Gastrointest Endosc 1992; 38: 676-83. [ Links ]
6. Rosch T, Meining A, Fruhmorgen S, Zillinger C, Schusdziarra V, Hellerhoff K, et al. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in the biliary strictures. Gastrointest Endosc 2002; 55: 870-6. [ Links ]
7. Lambert R, Caletti G, Cho E, Chang KJ, Fusaroli P, Feussner H, et al. International workshop on the clinical impact of endoscopic ultrasound in gastroenterology. Endoscopy 2000; 32: 549-84. [ Links ]
8. Fulcher AS, Turner MA, Capps G, Zfass AM, Baker KM. Half-Fourier RARE MRCP: Experience in 300 subjects. Radiology 1998; 207: 21-32. [ Links ]
9. Bret PM, Reinhold C. Magnetic resonance cholangiopancreatography. Endoscopy 1997; 29: 472-86. [ Links ]
10. Nitatori T, Hanaoka H, Hachiva J, Yokoyama K. MRI artefacts of metallic stents derived from imaging and the ferromagnetic nature of materials. Radiat Med 1999; 17 (4): 329-34. [ Links ]
11. Cannon ME, Carpenter SL, Elta GH, Nostrant TT, Kochman ML, Ginsberg GG, et al. EUS compared with CT, magnetic resonance imaging, and angio-graphy and the influence of biliary stenting on staging accuracy of ampullary neoplasm. Gastrointest Endosc 1999; 50: 27-33. [ Links ]