Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 no.4 Madrid abr. 2009
Psychological impact of Crohn's disease on patients in remission: anxiety and depression risks
Impacto psicológico de la enfermedad de Crohn en pacientes en remisión: riesgo de ansiedad y depresión
M. Iglesias1*, M. Barreiro de Acosta1,2*, I. Vázquez3, A. Figueiras4, L. Nieto1, A. Lorenzo2 and J. E. Domínguez-Muñoz1,2
1Fienad Hospital Clínico Universitario.
2Service of Digestive Diseases. Hospital Clínico Universitario.
3Department of Clinical Psychology. Universidad de Santiago.
4Service of Epidemiology. Hospital Clínico Universitario. Santiago de Compostela. A Coruña, Spain
*Both authors have equally contributed in the execution of the manuscript.
ABSTRACT
Background: the role of anxiety and depression in CD patients in remission has been poorly investigated.
Objective: the aim of the study was to evaluate the frequency of anxiety and depression symptoms in CD patients in remission, and potential factors influencing the development of these symptoms.
Methods: CD patients older than 18 years in remission for at least 6 months before study entry were included. CD remission was defined as a Crohn's disease Activity Index (CDAI) < 150 points together with C-reactive protein < 5 mg/L. A demographic questionnaire was filled in, and all patients were clinically classified. The therapy maintaining remission was also recorded. A Hospital Anxiety and Depression scale (HAD) was administered to all patients. Results are shown as OR and 95% CI, and analyzed by logistic regression.
Results: 92 consecutive patients were included (48 male, mean age 37 years, range from 18 to 71 years). One patient failed to correctly fill in the questionnaire. Anxiety and depression symptoms were present in 36 (39%) and 22 (24%) patients, respectively. Infliximab therapy was the only factor associated with anxiety (OR = 3.11; 95% CI: 1.03-9.43; p < 0.05). In contrast, the presence of depressive symptoms is less frequent in patients under infliximab therapy (OR = 0.16; 95% CI: 0.02-0.97; p < 0.05).
Conclusions: despite clinical remission, an important number of CD patients present with anxiety or depressive symptoms. Infliximab therapy in CD patients is associated to more anxiety but fewer depressive symptoms. CD patients in remission would probably benefit from psychological support.
Key words: Crohn's disease. Remission. Anxiety. Depression.
RESUMEN
Introducción: el papel de la ansiedad y depresión en pacientes con enfermedad de Crohn (EC) en remisión es incierto.
Objetivo: evaluar la frecuencia de ansiedad y depresión en pacientes con EC en remisión y potenciales factores que pueden influir en el desarrollo de esos síntomas.
Métodos: se incluyeron pacientes con EC mayores de 18 años, que estuviesen en remisión durante al menos 6 meses. La remisión se definió como un CDAI < 150 junto con una PCR < 5 mg/l. Se recogieron datos sociodemográficos y los pacientes fueron estratificados clínicamente y se evaluó el tratamiento empleado para el mantenimiento de la remisión. Los síntomas ansiosos y depresivos se evaluaron a través de la Hospital Anxiety and Depression Scale (HAD). Los resultados fueron analizados mediante regresión logística y se muestran como Odds ratio con un intervalo de confianza del 95%.
Resultados: se incluyeron 92 pacientes (48 hombres, edad media 37, rango 18 a 71 años). Un paciente no completó correctamente el cuestionario. Se encontraron síntomas ansiosos y depresivos en 36 (39%) y 22 (24%) pacientes respectivamente. El tratamiento con infliximab de mantenimiento fue el único factor asociado con ansiedad (OR = 3,11; 95% IC: 1,03-9,43; p < 0,05). Por el contrario, la presencia de síntomas depresivos es menos frecuente en pacientes en tratamiento de mantenimiento con infliximab (OR = 0,16; 95% IC: 0,02-0,97; p < 0,05).
Conclusiones: a pesar de estar en remisión clínica, un importante número de pacientes con EC presentas síntomas ansiosos o depresivos. El tratamiento con infliximab parece asociarse con más ansiedad pero menos síntomas depresivos. Probablemente algunos de estos pacientes serían susceptibles de tratamiento psicológico.
Palabras clave: Enfermedad de Crohn. Remisión. Ansiedad. Depresión.
Introduction
Patients suffering from inflammatory bowel disease (IBD) usually show more psychological morbidity (mainly depression and anxiety) when compared to the general population (1-4). Morbidity figures are very similar to those found in other populations of patients suffering from chronic diseases, especially rheumatological ones (5,6). However, some gaps remain to be solved in the relationship between psychological disorders and IBD. Whereas some authors have suggested that certain patients could be particularly vulnerable to psychological disorders as a result of traumas regardless of intestinal diseases (7), others have described a very close and direct connection between disease activity and psychological disorders, going so far as to suggest that the latter are a direct consequence of clinical symptoms (8,9). Both psychological morbidity and quality of life are usually disturbed in patients suffering from IBD, regardless of disease duration (10). Studies have found that patients with Crohn's disease (CD) have a poorer quality of life as compared to those suffering from ulcerative colitis (UC), probably because the latter has fewer physical after-effects (11,12). Nevertheless, other studies, as the one carried out in our country, do not find variations between both diseases (13).
Anxiety and depression usually appear individually and independently in patients suffering from chronic diseases. There is great evidence that both depressive symptoms and anxiety manifestations have a harmful effect on the outcome of several chronic diseases. In patients with a heart condition, depressive symptoms are associated with higher mortality rates (14), and higher depression scale scores in breast cancer patients have been associated with decreased survival (15). On the other hand, it has been seen that glycemia control is more difficult in diabetic patients suffering from depression versus non-depressed individuals (16).
Intestinal inflammatory diseases, both CD and UC, are chronic disorders characterized by periods of relapse and periods of remission or lack of symptoms. Nowadays the main aim of treatments in CD is remission, ultimately maintained remission (17,18). Recent guidelines issued by the European Crohn and Colitis Organization (ECCO) establish that remission (a criterion used in many clinical trials) is defined by a Crohn's disease Activity Index (CDAI) score lower than 150 (19), although values cannot be extrapolated to endoscopic remission (20).
Our hypothesis is that clinical remission does not involve the absence of psychological morbidity, and patients with CD in remission who may display anxiety and/or depression symptoms could benefit from psychological support.
The aim of our research was to evaluate the frequency of anxiety and depression symptoms in patients with CD in remission, and also to assess factors potentially leading to their development.
Material and methods
A prospective study has been carried out with the inclusion of CD patients who attended a monographic inflammatory bowel disease unit and who fulfilled the following criteria: over 18 years, CD defined under Lennard-Jones' criteria (21), and in clinical remission with no disease flares in the previous 6 months. Clinical remission has been defined as a CDAI under 150, a Harvey-Bradshaw equal to or below 3 with a C-reactive protein value lower than 5 mg/L.
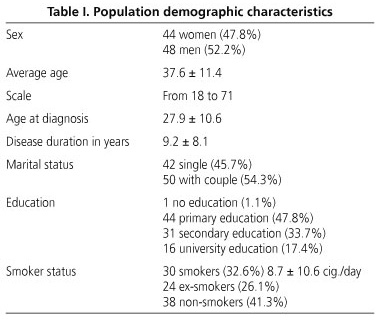
Based on previous findings in studies about quality of life, we selected variables with potential influence in psychological morbidity (22,23). Each patient filled a socio-demographic questionnaire which included age, sex, marital status, education, smoker status (including number of cigarettes smoked), age at diagnosis of CD, and number of years since diagnosis. All patients were clinically stratified by a specialist of the inflammatory bowel disease unit according to the phenotypes included in Montreal Classification (24), presence of extra-intestinal manifestations (EIM), perianal disease, previous surgery, and previous development of steroid dependence and steroid resistance, according to the definitions by ECCO (19). Likewise, the treatment employed to maintain remission was also assessed; if remission was sustained with biological therapies, it was specified whether with infliximab (IFX) or adalimumab (ADA); on the other hand, concomitant medications were evaluated, especially antidepressants and anxiolytics.
Anxiety and depression symptoms were evaluated based on the Hospital Anxiety and Depression scale (HAD) (25). A trained psychologist administered the questionnaire to all patients individually, clarifying all potential doubts. This scale was designed to detect the presence of anxiety and depression specifically in patients suffering from chronic diseases, and it tries to identify when anxiety and/or depression may have their origin in the course of a disease being treated in a hospital environment.
Anxiety and depression symptoms are evaluated separately, though in the same scale. We considered, following this scale and both for anxiety and depression, scores of 8 or higher to be abnormal, that is, as markers of anxiety or depression symptoms.
A univariate analysis was performed first, followed by a multivariate one using logistic regression in order to determine which socio-demographic and clinical variables could be influencing the emotional state of patients. The results are shown as odds ratios with a confidence interval of 95%. Statistical significance was considered for values at p < 0.05.
Results
Ninety-two patients (48 men and 44 women, average age of 37 years, from 18 to 71 years, and average length of disease of 9.2 ± 8) who fulfilled the inclusion criteria were included in a consecutive way. The demographic characteristics of the population are shown in table I.
As for the clinical characteristics of patients, 42 (45.7%) displayed EIMs, 25 (27.5%) had had a prior intestinal removal related to their CD, 37 (40.2%) had previously developed steroid dependence, and 41 (44.6%) had steroid resistance. Phenotypical characteristics of patients, according to the Montreal classification and including perianal disease, are shown in table II. Forty-three patients (46.7%) sustained remission using biological therapy, 32 of them (34.8%) using IFX and 11 (12%) using ADA; 3.2% of the sample were taking antidepressants at the time of the interview, and 6.4% were taking anxiolytics.
One of the 92 patients (1.1%) did not satisfactorily answer the HAD questionnaire, so these results could not be analyzed. Anxiety symptoms (a value of 8 or higher in the specific part for anxiety in HAD) were found in 36 patients (39%), and depression symptoms (a value of 8 or higher in the specific part for depression in HAD) were found in 22 patients (24%).
Anxiety
None of the socio-demographic or clinical parameters was significantly associated with de development of anxiety symptoms (Table III). Patients who sustained remission with IFX showed a higher risk of anxiety (OR = 3.11; 95% RI: 1.03-9.43; p < 0.05).
Depression
None of the demographic parameters was associated with the risk of presenting depression symptoms (Table III). As for the Montreal classification, neither age (OR = 1.04; 95% RI: 0.97-1.10; p = n.s.) nor behavior (B) (OR = 0.030; 95% RI: 0.43-21.17; p = n.s.) or perianal involvement (OR = 8.26; 95% RI: 1.24-55.04; p < 0.05) were associated with depression risk. Patients suffering from ileal disease (OR = 8.26; 95% RI: 1.24-55.04; p < 0.05) developed depression symptoms more frequently.
Differences between the fact of having previously been steroid-resistant (OR = 1.22; 95% RI: 0.45-3.27; p = n.s.) or having developed extra-intestinal manifestations (OR=2.04; 95% RI: 0.75-5.50; p = n.s.) were not observed; however, patients who had undergone prior surgery (OR = 13.01; 95% RI: 1.89-89.51; p < 0.01) developed a higher number of depression symptoms, whereas patients who had been steroid-dependant developed fewer depression symptoms (OR = 0.17; 95% RI: 0.04-0.65; p < 0.01). As for the treatments employed to sustain remission, it has been observed that depression symptoms are less frequent in patients treated with IFX (OR = 0.16; 95% RI: 0.02-0.97; p < 0.05).
Discussion
The results of this research, carried out with CD patients in clear remission, show that, despite being in remission, patients frequently present depression and anxiety symptoms, the latter predominating. These results are more relevant if we take into account that the prevalence of anxiety disorders amongst the general population has a global prevalence rate between 4 and 8%, whereas figures of depression stand around 6.2% in our country (26). As for the numerous potential factors analyzed, both demographic and clinical, that may influence anxiety risk, only maintenance treatment with IFX was associated with this risk. Based on the fact that the subgroup of patients treated with IFX are the ones who suffer from more serious CD, these results could be explained because of this severity or by the fact of having to regularly (every 8 weeks) go to hospital, a situation that can generate anxiety symptoms. There are no specific data about this topic regarding CD; however, extrapolating from other chronic diseases, such as heart and rheumatologic disorders, anxiety symptoms have been seen to worsen by frequent hospital visits (27,28).
No potential associations have been found with demographic parameters or the risk of developing depression symptoms, but a relation with some of clinical characteristics has been described. We did observe a higher presence of depression symptoms in patients who had undergone intestinal surgery. In this situation, there are no previous data specific for CD, although our results differ from those of a German study in that they do not find a higher number of depression symptoms in patients with UC having undergone restoring proctocolectomy with ileo-anal reservoir (29). In some conditions other than IBD, such as gynecological or epileptic surgery, a higher presence of depression symptoms has been seen - as in our study - in patients who underwent surgery, regardless of the positive effect of surgery and time elapsed since the procedure (30,31). It is more difficult to justify why patients with exclusive ileal involvement have a higher number of depression symptoms; these results must be verified by further studies.
The only clinical factor that we found associated with fewer depression symptoms is prior steroid dependence. This result alerts us to the dangers of constantly using corticosteroids, which already in the TREAT registry proved to be the drugs associated with a higher number of infections and deaths in CD (32); on the other hand, they are drugs employed in the treatment of CD, and are associated with higher psychological morbidity, especially among younger patients (33,34). So, it is easy to understand that steroid-dependent patients with adverse effects directly related to cosmetic (cushingoid), who are in remission on novel drugs and no corticoids, are those who experienced greater improvement, and because of this, have fewer depression symptoms. As for the treatment used to sustain remission, we saw that patients who sustained remission using IFX had fewer depression symptoms. Our results are similar to those described by the Leuven group (35), who observed that, in patients treated with IFX, CDAI drops were greater in patients with depression at treatment onset, and depression symptoms decreased with CDAI improvement.
Nowadays, even if it seems clear that the therapeutic goal for patients with CD is clinical remission, a debate about considering endoscopic remission, besides measuring remission by clinical indexes, is gaining importance; that is, considering mucusal healing as an objective (20). On observing that one third of patients have anxiety symptoms and more than one fifth have depression symptoms even during clinical remission, we should try to include psychological stabilization among treatment objectives.
Previously, several studies had proven that disease activity was clearly related to the development of psychological symptoms, both in CD and UC (36,37). A more recent 18-month, prospective research concluded that both depression and anxiety have a negative influence in the course of IBD (9). Lack of data about CD patients in remission is surprising, even though an Italian study found that, in patients with UC in remission, depressive symptoms were not associated with a higher risk of flare-ups, while stress was (38).
Our research has some limitations that may determine some of the results. The main one is that, even if these patients were clearly in clinical remission, some serious and high-risk patients were included, since 46.7% were being treated with biological therapies. This information makes us believe that some of the psychological symptoms of these patients could stem from previous seriousness. Another limitation of our research is that we do not know the emotional status of patients during their previous flare, so we cannot assess whether psychological morbidity had improved with the treatment employed to achieve remission.
Taking as a basis studies previously published, in which an improvement of anxiety and depression symptoms was clearly seen in patients with DII receiving psychological support, we believe that CD patients with psychological symptoms should, regardless of disease activity, receive psychological therapy from specialized clinical psychologists. Psychotherapy may have positive effects on the psychological magnitude of this disease - psychological wellbeing, coping strategies, psychological unease (39-41). This therapy, together with conventional medicine, would render remission more complete in cases with associated psychological morbidity, which would improve quality of life and make it similar to that of healthy subjects.
![]() Correspondence:
Correspondence:
Manuel Barreiro de Acosta.
Servicio de Aparato Digestivo.
Hospital Clínico Universitario.
C/ Choupana, s/n-.
15706 Santiago de Compostela. A Coruña, Spain.
e-mail: manubarreiro@hotmail.com
Received: 30-12-08.
Accepted: 30-01-09.
References
1. Maunder RG, Levenstein S. The role of stress in the development and clinical course of inflammatory bowel disease: epidemiological evidence. Curr Mol Med 2008; 8: 247-52. [ Links ]
2. Maunder RG. Evidence that stress contributes to inflammatory bowel disease: evaluation, synthesis, and future directions. Inflamm Bowel Dis 2005; 11: 600-8. [ Links ]
3. Helzer JE, Stillings WA, Chammas S, Norland CC, Alpers DH. A controlled study of the association between ulcerative colitis and psychiatric diagnoses. Dig Dis Sci 1982; 27: 513-8. [ Links ]
4. Addolorato G, Capristo E, Stefanini GF, Gasbarrini G. Inflammatory bowel disease: a study of the association between anxiety and depression, physical morbidity, and nutritional status. Scand J Gastroenterol 1997; 32: 1013-21. [ Links ]
5. O'Malley PG, Jackson JL, Kroenke K, Yoon K, Hornstein E, Dennis GJ. The value of screening for psychiatric disorders in rheumatology referrals. Arch Intern Med 1998; 158: 2357-62. [ Links ]
6. Maiden NL, Hurst NP, Lochhead A, Carson AJ, Sharpe M. Medically unexplained symptoms in patients referred to a specialist rheumatology service: prevalence and associations. Rheumatology 2003; 42: 108-12. [ Links ]
7. Walker EA, Unutzer J, Rutter C, Gelfand A, Saunders K, VonKorff M, et al. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Arch Gen Psychiatry 1999; 56: 609-13. [ Links ]
8. Porcelli P, Leoci C, Guerra V. A prospective study of the relationship between disease activity and psychologic distress in patients with inflammatory bowel disease. Scand J Gastroenterol 1996; 31:792-6. [ Links ]
9. Mittermaier C, Dejaco C, Waldhoer T, Oefferlbauer-Ernst A, Miehsler W, Beier M, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med 2004; 66: 79-84. [ Links ]
10. Casellas F, López Vivancos J, Malagelada JR. Previous experience and quality of life in patients with inflammatory bowel disease during relapse. Rev Esp Enferm Dig 2003; 95: 476-9. [ Links ]
11. Drossman DA, Li Z, Leserman J, Patrick DL. Ulcerative colitis and Crohn's disease health status scales for research and clinical practice. J Clin Gastroenterol 1992; 15: 104-12. [ Links ]
12. Bernklev T, Jahnsen J, Aadland E, Sauar J, Schulz T, Lygren I, et al. Health-related quality of life in patients with inflammatory bowel disease five years after the initial diagnosis. Scand J Gastroenterol 2004; 39: 365-73. [ Links ]
13. Casellas F, Arenas JI, Baudet JS, Fábregas S, García N, Gelabert J, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis 2005; 11: 488-96. [ Links ]
14. Lespérance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002; 105: 1049-53. [ Links ]
15. Watson M, Haviland JS, Greer S, Davidson J, Bliss JM. Influence of psychological response on survival in breast cancer: a population-based cohort study. Lancet 1999; 354: 1331-6. [ Links ]
16. Lustman PJ, Griffith LS, Freedland KE, Clouse RE. The course of major depression in diabetes. Gen Hosp Psychiatry 1997; 19: 138-43. [ Links ]
17. Vermeire S, van Assche G, Rutgeerts P. Review article: altering the natural history of Crohn's disease--evidence for and against current therapies. Aliment Pharmacol Ther 2007; 25: 3-12. [ Links ]
18. Travis S. Advances in therapeutic approaches to ulcerative colitis and Crohn's disease. Curr Gastroenterol Rep 2005; 7: 475-84. [ Links ]
19. Stange EF, Travis SP, Vermeire S, Beglinger C, Kupcinkas L, Geboes K, et al. European evidence based consensus on the diagnosis and management of Crohn's disease: definitions and diagnosis. Gut 2006; 55 Supl. 1: i1-15. [ Links ]
20. Rutgeerts P, Vermeire S, Van Assche G. Mucosal healing in inflammatory bowel disease: impossible ideal or therapeutic target? Gut 2007; 56: 453-5. [ Links ]
21. Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl 1989; 170: 2-6. [ Links ]
22. Casellas F, López-Vivancos J, Casado A, Malagelada JR. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res 2002; 11: 775-81. [ Links ]
23. López Blanco B, Moreno-Jiménez B, Devesa Múgica JM, Rodríguez Muñoz A. Relationship between socio-demographic and clinical variables, and health-related quality of life in patients with inflammatory bowel disease. Rev Esp Enferm Dig 2005; 97: 887-98. [ Links ]
24. Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19 (Supl. A): 5-36. [ Links ]
25. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361-70. [ Links ]
26. Bernardo M, Fuente E. Epidemiología psiquiátrica. En: Vallejo Ruiloba J. Introducción a la psicopatología y a la psiquiatría. 6ª ed. Editorial Masson. p. 47-54. [ Links ]
27. Tully PJ, Baker RA, Turnbull D, Winefield H. The role of depression and anxiety symptoms in hospital readmissions after cardiac surgery. J Behav Med 2008; 31: 281-90. [ Links ]
28. Carone AR, D'Amore S, Albanese L, Craig F, Scagliusi P, D'Amore M. Hospital anxiety and depression. Reumatismo 2007; 59: 304-15. [ Links ]
29. Häuser W, Janke KH, Stallmach A. Mental disorder and psychologic distress in patients with ulcerative colitis after ileal pouch-anal anastomosis. Dis Colon Rectum 2005; 48: 952-62. [ Links ]
30. Yen JY, Chen YH, Long CY, Chang Y, Yen CF, Chen CC, et al. Risk factors for major depressive disorder and the psychological impact of hysterectomy: a prospective investigation. Psychosomatics 2008; 49: 137-42. [ Links ]
31. Siegel AM, Cascino GD, Fessler AJ, So EL, Meyer FB. Psychiatric co-morbidity in 75 patients undergoing epilepsy surgery: lack of correlation with pathological findings. Epilepsy Res 2008; 80: 158-62. [ Links ]
32. Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Chen DM, et al. Serious infections and mortality in association with therapies for Crohn's disease: TREAT registry. Clin Gastroenterol Hepatol 2006; 4: 621-30. [ Links ]
33. Brown ES, Suppes T. Mood symptoms during corticosteroid therapy: a review. Harv Rev Psychiatry 1998; 5: 239-46. [ Links ]
34. Stuart FA, Segal TY, Keady S. Adverse psychological effects of corticosteroids in children and adolescents. Arch Dis Child 2005; 90: 500-6. [ Links ]
35. Persoons P, Vermeire S, Demyttenaere K, Fischler B, Vandenberghe J, Van Oudenhove L, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn's disease treatment with infliximab. Aliment Pharmacol Ther 2005; 22: 101-10. [ Links ]
36. Andrews H, Barczak P, Allan RN. Psychiatric illness in patients with inflammatory bowel disease. Gut 1987; 28: 1600-4. [ Links ]
37. North CS, Alpers DH, Helzer JE, Spitznagel EL, Clouse RE. Do life events or depression exacerbate inflammatory bowel disease? A prospective study. Ann Intern Med. 1991; 114: 381-6. [ Links ]
38. Levenstein S, Prantera C, Varvo V, Scribano ML, Andreoli A, Luzi C, et al. Stress and exacerbation in ulcerative colitis: a prospective study of patients enrolled in remission. Am J Gastroenterol 2000; 95: 1213-20. [ Links ]
39. Díaz Sibaja MA, Comeche Moreno MI, Mas Hesse B. Protocolized cognitive-behavioural group therapy for inflammatory bowel disease. Rev Esp Enferm Dig 2007; 99: 593-8. [ Links ]
40. Mussell M, Böcker U, Nagel N, Olbrich R, Singer MV. Reducing psychological distress in patients with inflammatory bowel disease by cognitive-behavioural treatment: exploratory study of effectiveness. Scand J Gastroenterol 2003; 38: 755-62. [ Links ]
41. García Vega E, Fernández Rodríguez C, Sánchez Lombraña JL. Behavioral profile of the patient with Crohn's disease. Rev Esp Enferm Dig 1994; 86: 791-5. [ Links ]











 texto en
texto en