Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 no.6 Madrid jun. 2009
PICTURES IN DIGESTIVE PATHOLOGY
Abdominal pain for 9 days
Dolor abdominal de 9 días de evolución
J. P. Miramontes González, J. M. Fernández Rodríguez1, E. Puerto Pérez, J. M. Sánchez Tocino1, N. Cubino Bóveda and S. Carrero García1
Services of Internal Medicine I and 1General Surgery. Hospital Virgen de la Vega. Salamanca, Spain
Case report
We report the case of a 22-year-old male patient who was admitted at the ER because of abdominal pain for 9 days. His personal record did not reveal any significant findings, operations, toxic habits, or regular medications.
The patient reported abdominal pain in the right lower quadrant for 9 days. He did not relate the pain to any specific event, and he described it as of moderately severe, constant pain irradiating to the left thigh, unaltered when moving, resting or sleeping. The patient did not present nausea or vomiting, and his intestinal habit was normal. He had no fever or feelings of dysthermia.
Physical exploration revealed: BP: 117/82, HR: 92 bpm, T: 37.1 ºC. Abdominal exploration revealed normal abdominal noises, and no masses or enlargement of the abdominal organs were observed. Surface palpation was normal, but deep palpation triggered a moderately severe pain in the right lower quadrant (RIF) with no peritoneal response.
Emergency blood testing revealed: biochemistry: glucose 109 mg/dl, urea 23 mg/dl, Cr 0,86 mg/dl, Na 138 mmol, K+ 5,3 mmol, C-reactive protein (CRP) 6,0 mg/dl, osmolarity 266 msom/kg; the urinalysis showed no disorders. Hemogram: hemoglobin 15.6 g/dl, hematocrit 45.4%, mean corpuscular volume (MCV) 87 fl, leukocytes 11900/ml, neutrophils 74.1%, platelets 220,000/ml. Coagulation: prothrombin time (PT): 98%, activated partial thromboplastin time (APTT): 32.7 s.
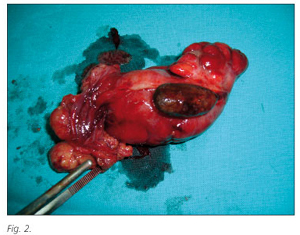
An abdominal X-ray reveals a well-defined oval mass of 4 cm in the right hemipelvis (we include the picture with the surgical specimen).

Afterwards, an ultrasonogram was performed, which was compatible with appendicitis, although other pathologies could not be ruled out. The test also showed free periappendicular fluid, a big appendicolith, and big, 8-9-cm adenopathies in the RIF.
A McBurney's incision was performed, and the appendix was removed, showing a great inflammatory reaction that reached the mesoileum and cecum. The report from the Pathology Department on the surgical specimen suggested acute appendicitis, intra-appendicular fecalith, and reactive lymphadenitis.
Discussion
The slow progression of symptoms, absence of common symptoms (1) (such as abdominal pain with acute-subacute onset, located mainly in the RIF, fever or peritoneal reaction, which are common in acute appendicitis), poor lab expression with low leukocyte count, and absence of other atypical symptoms (2), together with the presentation of a big surgical specimen and inflammatory reaction, prompted a differential diagnosis with appendicular tumors (3).
References
1. Sabiston DC, Townsend CM, Bauchamp RD, Evers BM, Mattox KL, Balibrea Cantero JL. Tratado de Cirugía: Fundamentos biológicos de la práctica quirúrgica moderna. Ed. 17. Elsevier España; 2005. [ Links ]
2. Beltrán MS, Villar RM, Tapia TF, Karina EU, Cruces B. Sintomatología atípica en 140 pacientes con apendicitis. Rev Chilena de Cirugía 2004;56: 269-74. [ Links ]
3. Muñoz Madero VA, Pérez Sánchez CB. Estrategia diagnóstica y terapéutica en los tumores del apéndice vermiforme. Cirugía Española 2000; 68(3): 229-34. [ Links ]











 texto en
texto en 


