My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 n.6 Madrid Jun. 2009
LETTERS TO THE EDITOR
Bowel perforation secondary to intestinal tuberculosis
Perforación intestinal secundaria a tuberculosis intestinal
Key words: Intestinal perforation. Gastrointestinal tuberculosis. Peritonitis.
Palabras clave: Perforación intestinal. Tuberculosis intestinal. Peritonitis.
Dear Editor,
Tuberculosis (TB) continues to be a major health problem worldwide and one of the illness that should be kept in mind currently due to its varying clinical symptoms. Its incidence is increasing in developed countries, where most cases of multifocal TB are reported among immigrants from high endemic areas and in immunodepressed subjects (1). WHO estimates that there were 9,2 million new cases of TB in 2006 (139 per 100,000), being the incidence in Spain 30/100,000 inhabitants/year (2). The most common place affected by TB is the lung, followed by the gastrointestinal tract and the genitourinary system (3).
Case report
We herein describe a 33-years old Hispanic-American male, residing in Spain the last 4 years, who was admitted to the hospital due to constitutional syndrome, fever, productive cough and abdominal pain of seven month's duration. He had a history of parapneumonic effusion 2 years before and strongiloidosis treated with albendazol.
On physical examination, he was febrile (38.2 ºC), eupneic, normotense, his abdomen was spreading painful without signs of peritoneal irritation and bowel sounds were audible. Blood analysis demonstrated anaemia (haemoglobin 7.7 g/dL), leukocytes 7,300 (88% neutrophils; 9.1% lymphocytes; 2.2% monocytes), platelets 631,000, erythrocyte sedimentation rate 127 mm/h and serum total protein level 51 g/L (albumin 24 g/L).
He was diagnosed of smear-positive pulmonary TB with positive bacilloscopy and cultures for Mycobacterium tuberculosis. Chest radiograph was normal and computed tomography (CT) showed numerous nodes in lung parenchyma, intestinal wall thickening, disseminated peritoneal and mesenteric nodules and multiple thoracic and abdominal swollen lymph nodes strongly suggestive of multifocal TB.
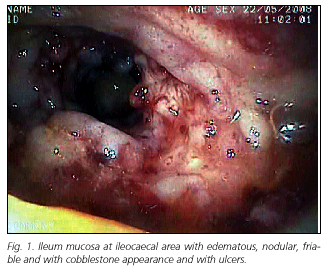
Colon-ileoscopy identified an edematous, nodular, friable and with cobblestone appearance mucosa with ulcers compatible with a diagnosis of TB (Fig. 1).
Anti TB treatment was performed with isoniazid, rifampicin and pyrazinamide, but after two weeks with no clinical response, he had acute abdomen symptoms. CT showed free peritoneal air and fluid, therefore urgent laparotomy was performed. Surgical findings were a widespread of whitish tuberculomas resembling "millet grain" on peritoneum, intestinal serosa and epiploon and a terminal ileal perforation too, which was treated by cleaning of the lesion borders and simple closure. During the following two months the patient had to be reoperated twice due to new yeyunal and ileal perforation episodes, where perforations were identified and simply sutured in both cases. On last surgery the correct cicatrization of the previously sutured perforations was confirmed.
Pathology results of the obtained biopsy samples revealed the presence of chronic caseating granuloma type TB and the absence of acid-fast bacilli (AFB) with the Ziehl-Nielsen staining. Ascitic fluid culture was likewise negative for AFB.
Discussion
Mycobacterium tuberculosis is responsible for most cases of abdominal tuberculosis, either primary due to ingestion of contaminated food, or secondarily due to sputum swallow or during a bacteraemic phase in pulmonary TB, in which case the peritoneum, the mesenteric nodes, the intestines and other abdominal organs can be affected (4).
The most common site affected by intestinal TB is the ileocaecal region, which explains many of its symptoms (4). The bacillus nests at that area, developing an inflammation process that finishes in mucosa ulceration and subsequent cicatrisation (1).
The most common symptoms of intestinal TB are abdominal pain, diarrhoea, weight loss, anorexia, fever, anemia and lower gastrointestinal bleeding, which can be associated with symptoms of pulmonary TB if presents (5,6). Physical examination usually shows abdominal tenderness, distension and/or abdominal mass (5).
Due to its nonspecific clinical features and without a high index of suspicion, diagnosis can be ignored or delayed increasing consequently the rates of mortality and morbidity (3,5). Colonoscopy with biopsy is the diagnostic procedure of choice in intestinal involvement, even though the absence of histological confirmation does not exclude the presence of TB (5-7). Colonoscopy can show ulcerations, nodules, polypoid lesions and stenosis. Macroscopic findings can be ulcerative, hyperplasic and sclerotic lesions (1,3,4). Ascitic fluid culture and the presence of adenosine deaminase can help to differentiate it from other processes too (7).
The imaging procedure of choice is CT, which can show thickening at the ileocaecal area, diffuse peritoneum, omentum and mesenteric involvement, coexisting with lymph nodes with hypodense nucleus and peripheral ring enhancement. These are not, however, pathognomic features (6). Laparoscopy has become a sure and accurate diagnostic tool under the suspicion of abdominal TB and is considered the primary intraperitoneal approach. It allows us to obtain histological samples and guarantees a correct viewing of the peritoneal cavity, providing characteristic images such as adhesions between peritoneum and other abdominal organs and caseum granulomas throughout the peritoneum (8).
Differential diagnosis should include specially Crohn's disease, and definitive diagnosis is established by histology and culture of the lesions (1,6).
Medical treatment with triple therapy during 12 months should start as soon as TB is diagnosed and the response is usually satisfactory (3,4).
Surgical management should be used only to treat complications such as obstruction, perforation, stenosis, haemorrhage, abscess and fistula, which requires early surgical treatment (1,3-5). In these cases, a bowel resection of the affected segments and end-to-end anastomosis is recommended, with better results than other less aggressive techniques like excision of perforation margins and simple suture with patch of epiploon, bypass or drainage alone (5). In our case, simple closure was preferred due to the wide intestinal involvement and the bad general status of the patient, like other authors advocate (3).
Although most recommendations advocate for a more aggressive surgical attitude, from our point of view this one should be valued according to the patient medical condition and the extension of enteric involvement as well as the attendant pathologies.
M. Ruiz Marín, F. M. González Valverde, J. A. Benavides Buleje, C. Escamilla
Segade, M. F. Candel Arenas, E. Terol Garaulet and A. Albarracín Marín-Blázquez
Departament of General Surgery and Digestive Diseases. Reina Sofía General University Hospital. Murcia. Spain
References
1. Ruiz Gómez, JL García Díaz RA, Rodríguez San Juan JC, García Palomo D, Gómez Fleitas M. Tuberculosis intestinal perforada en paciente inmunocompetente. Rev Esp Enferm Dig 2006; 98(10): 793-4. [ Links ]
2. Global tuberculosis control: surveillance, planning, financing: WHO report 2008. [ Links ]
3. Akgun Y. Intestinal and peritoneal tuberculosis: changing trends over 10 years and a review of 80 patients. Can J Surg 2005; 48(2): 131-6. [ Links ]
4. Muquit S, Shah M, Abayajeewa K. A case of miliary tuberculosis presenting with bowel perforation. Emerg Med J 2006; 23: e62. [ Links ]
5. Polat KY, Aydinli B, Yilmaz O, Aslan S, Gursan N, Ozturk G, et al. Intestinal tuberculosis and secondary liver abscess. Mt Sinai J Med 2006; 73(6): 887-90. [ Links ]
6. Serf R, Rotterova P, Konecny J. Perforation peritonitis in primary intestinal tuberculosis. Dig Surg 2001; 18(6): 475-9. [ Links ]
7. Fernández Sarabia MT, Cardenal Escarcena A, Roldán Lora FA, Rivero Cruz MA, Encinas Tobajas VM. Intestinal perforation: an unusual complication of the intestinal tuberculosis that simulated Crohn's disease Rev Esp Enferm Dig 2005; 97(7): 536-7. [ Links ]
8. Suárez Grau JM, Rubio Chaves C, García Moreno JL, Martín Cartes JA, Socas Macías M, Alamo Martínez JM, et al. Atypical peritoneal tuberculosis. Use of laparoscopy in the diagnosis. Rev Esp Enferm Dig 2007; 99(12): 725-8. [ Links ]











 text in
text in