Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 no.10 Madrid oct. 2009
PICTURES IN DIGESTIVE PATHOLOGY
Endoscopic ultrasound (EUS) elastography of the liver
Elastografía hepática guiada por ultrasonografía endoscópica
J. Iglesias García J1,2, J. Lariño Noia1,2, R. Souto1,2, A. Álvarez Castro1,2, B. Cigarrán2,3 and J. E. Domínguez Muñoz1,2
1Gastroenterology Department, and 2Foundation for Research in Digestive Diseases. University Hospital of Santiago de Compostela. A Coruña, Spain. 3Department of Internal Medicine. Virxe da Xunqueira Hospital. Cee. A Coruña, Spain
Case report
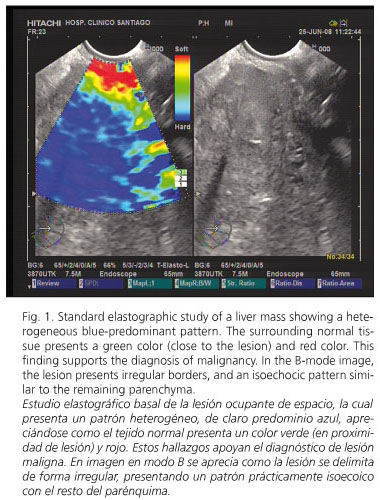
A 68-year-old woman with no previous medical history, except a lumbar vertebra broken at the age of 35, was first admitted because of abdominal pain in the right hypochondria for the last few weeks, together with anorexia and weight loss of 6 kg. A lab workup showed a slight increase of bilirubin (2.34 mg/dL) as well as liver and cholestasis enzymes [AST (245), ALT (375), GGT (636) and alkaline phosphatase (694)]. The remaining parameters, including tumor markers, were completely normal. A helical CT scan identified an enlarged choledocus with an associated dilatation of the intrahepatic biliary tree. A liver solid lesion in segment IVB, 6 x 5.1 x 3.5 cm in size, was also detected, which had poorly defined borders and exofitic growing, suggesting metastasis. We obtained an endoscopic ultrasonogram (EUS) with the linear EUS probe (EG 3870 UTK; Pentax Europe GmbH, Hamburg, Germany) attached to a platform 900 (Hitachi Medical Systems GmbH, Wiesbaden, Germany), which includes the elastography module. During EUS we performed an elastographic evaluation of the solid liver lesion, and obtained a heterogeneous blue-predominant pattern with slight green areas and red lines resulting in a geographic appearance (characteristic of malignant tumors); the mass was clearly differentiated from normal tissue (Fig. 1). In the second-generation elastography study, the strain ratio obtained was 11.76, with a value for area A (corresponding to the lesion) of 0.04% (Fig. 2). A EUS-guided fine-needle aspiration of the liver lesion with a 22-gauge needle (Echo-Tip from Wilson-cook Medical, Winston-Salem, North Carolina, USA) was performed. This biopsy confirmed the diagnosis of cholangiocarcinoma. Finally, the patient underwent an endoscopic retrograde cholangio-pancreatography that confirmed the presence of a 2-cm filiform stenosis in the middle portion of the common bile duct (Fig. 3); a Wallstent® (10 mm diameter, 60 mm length) was inserted for palliative treatment.
Discussion
Transient liver elastography is mainly used for the quantification of liver fibrosis. In this setting, Fibroscan® has been the method most commonly used to perform this quantification, allowing an easy, quick and a non-invasive measurement of tissue stiffness. Many publications analyze the usefulness of this technique, which demonstrates a very high diagnostic accuracy, close to 90%, for the determination of cirrhosis, but more limited for the evaluation of fibrosis in early stages (1). However, there are few studies evaluating its usefulness in the differential diagnosis of solid liver lesions.
A new model of elastographic equipment has been developed by Hitachi®, which allows a real-time evaluation of tissue stiffness; it has been used for the analysis of superficial organ lesions, associated with percutaneous ultrasounds (2), and of pancreatic lesions and lymph nodes, associated with EUS (3,4). The technology is based on the detection of small structure deformations within the B-mode image as caused by compression, so that strain is smaller in hard tissue versus soft tissue. The degree of deformation is used as an indicator of tissue stiffness. Different elasticity values are marked with different colors resulting in different tissue elasticity patterns.
Tissue elasticity is usually uniform in benign lesions, with stiffness ranging from soft to intermediate (colors yellow and green); on the other hand, malignant tumors grow in a disorganized manner, and show heterogeneous patterns with hard tissue (blue color) (4,5). In order to obviate the bias related to the subjective interpretation of the color map, a quantitative analysis is possible with second-generation elastogragphy. With this method, two different areas (A and B) from the region of interest are selected: area A is representative of the mass, and area B refers to a soft reference area; finally, a B/A ratio (strain ratio) is considered the result of the elastographic evaluation. Data published on this new technique are scarce, but malignant lesions show higher strain ratios when compared to benign lesions (5).
We present two images demonstrating the feasibility of a EUS-guided elastographic study of the liver, both standard and second-generation. This is possible due to the proximity of the liver (mainly left liver lobe) to the gastric and duodenal wall. The probe is pressed against the wall with only the pressure needed for an optimal and stable B-mode image at 7.5 MHz. In conclusion, liver EUS-guided elastography could be a useful tool in the evaluation of some patients with solid liver tumors.
References
1. Talwalkar JA. Elastography for detecting hepatic fibrosis: options and considerations. Gastroenterology 2008; 135: 299-302. [ Links ]
2. Gao L, Parker KJ, Lerner RM, Levinson SF. Imaging of the elasticity properties of tissue-a review. Ultrasound Med Biol 1996; 22: 959-77. [ Links ]
3. Saftoiu A, Vilman P. Endoscopic ultrasound elastography - a new imaging technique for the visualization of tissue elasticity distribution. J Gastrointestin Liver Dis 2006; 15: 161-5. [ Links ]
4. Giovannini M, Hookey LC, Bories E, Pesenti C, Monges G, Delpero JR. Endoscopic ultrasound elastography: the first step towards virtual biopsy? Preliminary results in 49 patients. Endoscopy 2006; 38(4): 344-8. [ Links ]
5. Iglesias-García J, Lariño-Noia J, Dominguez-Muñoz JE. Elastografía pancreática. Gastroenterología y Hepatología Continuada 2009 (en prensa). [ Links ]











 texto en
texto en