My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 n.11 Madrid Nov. 2009
LETTERS TO THE EDITOR
Giant lipoma and intestinal intussusception
Lipoma gigante de colon e invaginación intestinal
Key words: Lipoma. Intestinal intussuseption. Polyps. Suboclusion. Colonoscopy.
Palabras clave: Lipoma. Invaginación intestinal. Pólipos. Suboclusión. Colonoscopia.
Dear Editor,
We have recently read in your magazine an interesting case report of a polypoid colonic lesion (colonic lipoma) in which Gonzalez López et al. highlighted the rarity of this benign lesion and reviewed various aspects of this entity, concerning the localization and the clinical features (1). We have had the opportunity to diagnose two cases of giant colonic lipoma with suboclusive clinic between June and November of 2008.
Case report 1
A 43 years old woman consulted for episodes of abdominal pain and diarrhoea for 6 month. She did not have any anal bleeding or weight lost. The physical exam was irrelevant. Complementary analysis showed: Hb: 9,8 g/dl. Fe: 13 mcg/100 (normal: 50-140). The rest of the biochemical parameters, including CEA and CA 19.9, were normal. Colonoscopy revealed a giant mobile polypoid tumour at the union of the spleen angle and the descending colon, which prevented the passage of the endoscope. The head of the lesion was ulcerated. Biopsies were negative for malignancy. An abdominal CT image showed an intussusception in the descending colon. The patient was admitted before the scheduled date for surgery, presenting new and more intense suboclusive symptoms. During surgery, a large wide base polypoid tumour in the descending colon, near the splenic angle, was warned. A left hemicolectomy was performed. The pathologist report informed of a submucosal lipoma in the splenic angle, of 5 cm in diameter, with ulcerated mucosa. Twenty two lymph nodes were isolated and informed as of reactive origin.
Case report 2
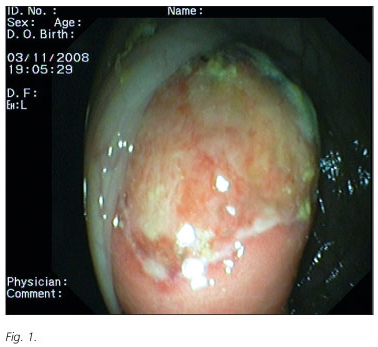
A 57 years old woman, with no pathologic history, consulted for intermittent episodes of abdominal pain and diarrhoea of 4 month. She did not present any anal bleeding. The physical exam was irrelevant and the laboratory tests were normal. Colonoscopy revealed a large polypoid lesion into the transverse colon, occupying almost entirely the light, and showing ulcerations on top (tumour's head) (Fig. 1). The place was marked with a clip to better assess the location of the polyp by a plain X-ray. Biopsies were taken which were reported as colonic mucosa with ulceration signs and granulation tissue and fibrous connective tissue, without evidence of malignancy. The abdominal CT scan confirmed the endoscopic findings. Three weeks later the patient had to be operated on emergency, for presenting suboclusive symptoms. Surgery revealed a colonic intussusception associated to a tumour of 5.5 cm, of submucosal origin. A left hemicolectomy was performed. Several lymph nodes were isolated and informed as of reactive origin.
Discussion
Lipomas are rare benign tumours of the gastrointestinal tract. Nevertheless, colon is a common site to diagnose this pathology. The most usual to diagnose is the right colon, reducing its frequency in the distal end. Diagnose of two cases of lipoma in such a small period of time demonstrates that this rare pathology does exist and must be taken into account. In our experience, both cases were affecting women of middle age. Colonoscopy plays an important role in the giant colonic lipomas management, since this may be seen generally as a rough, brownish, polypoid lesion with ulcerated areas. There is not always present the typical yellowish colour. The placement of a clip adjacent to the lipoma permits a more accurately localization of the lesion, especially when a previous abdominal CT scan is not performed. The options to confirm the diagnosis include the echoendoscopy to confirm the lesion of hipo-echogenic aspect, and the endoscopy. The final treatment of the giant colonic lipoma is surgery, especially when this implies symptoms of acute intestinal occlusion or recurrent intussusception, as we show in the two cases reported here. There are several older publications presenting cases in which safe endoscopic resections of this kind of tumour are performed (2,3). In other publication, the authors warn that endoscopic resection of lipomas bigger than 2 cm in diameter may be associated with bigger perforation risk (4). Recently, isolated cases were published, with good results concerning the endoscopic resection (5,6). In one of them, after the completion of an echoendoscopy which confirmed that the tumour was superficial to the muscle layer, no complications occurred after resection (5). Nowadays, surgery remains the recommended treatment for giant colonic lipomas. However, increased experience with endoscopic resection can make it a safe option. The treatment of choice should be based on the clinical trial and in any case must be performed as soon as possible, in order to prevent recurrent episodes of suboclusive symptoms.
J. Espinel, E. Pinedo1 and G. Rascarachi
Departments of Gastroenterology, and 1Radiology. Hospital de León. Spain
References
1. González López C, Vallejo A, Armas JR, Pellicer F, Herrerias JM. Lesión polipoidea colónica infrecuente. Rev Esp Enferm Dig 2008; 100(10): 663-4. [ Links ]
2. Papp JP, Haubrich WS. Endoscopic removal of colonic lipomas. Gastrointest Endosc 1973; 20: 66-7. [ Links ]
3. Waye JD, Frankel A. Removal of pedunculated lipoma by colonoscopy. Am J Gastroenterol 1974; 61: 221-2. [ Links ]
4. Bar-Meir S, Halla A, Baratz M. Endoscopic removal of colonic lipomas. Endoscopy 1981; 13: 135-6. [ Links ]
5. Kim CY, Bandres D, Tio L, Benjamin SB, Al-Kawas FH. Endoscopic removal of large colonic lipomas. Gastrointest Endosc 2002; 55(7): 929-31. [ Links ]
6. Wild D, Fiore J, Guelrud M. Successful endoscopic resection of a giant colonic lipoma causing intussusception. Gastrointest Endosc 2008; 68(4): 774-5. [ Links ]











 text in
text in