Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.1 Madrid ene. 2010
LETTERS TO THE EDITOR
Gastric transposition after esophago-coloplasty failure by the graft necrosis in the surgical management of the long gap esophageal atresia type I
Transposición gástrica tras fracaso de esófago-coloplastia por necrosis del injerto en el tratamiento de atresia esofágica tipo I de brecha larga
Key words: Esophageal atresia type I. Complications. Gastric ascension.
Palabras clave: Atresia esofágica tipo I. Complicaciones. Ascenso gástrico.
Dear Editor,
Type 1 esophageal atresia represents around 5% of all atresias in this organ. This nosological entity is not a commonly presentation and represent a challenge from the surgical resolution view point (1). Some important factors to consider are the length of the atresic segment, the conditions of the proximal esophagic sac as well as the existence and condition of the distal esophagic sac. From the therapeutic point of view there are different proposals that range from the reconstruction of the gap with resection and termino-terminal anastomosis of autologus esophagus because the atresic segment is short, as with circular miotomies that allow esophagic elongation, or the current Kimura or Foker techniques in an attempt to elongate the esophagus by continuous traction of the esophagic ends; even the techniques of interposition of other organs like small bowel, colon or full stomach or through the realization of a gastric tube (iso or anisoperistaltic) without dependence of the ascendent way (retro-sternal, mediastinical, etc.) (1-6).
The complication rates of these different techniques is not insignificant (2-5) and in the case of organic ascends, the graft necrosis (6) is probably the most distressing, not only because of the high risks of this complication, but also because the posterior reestablishment of the digestive continuity is usually extremely difficult.
The aim of this communication is to present the results obtained in a patient who presented total necrosis of the colonic graft and a posterior gastric ascent.
Case report
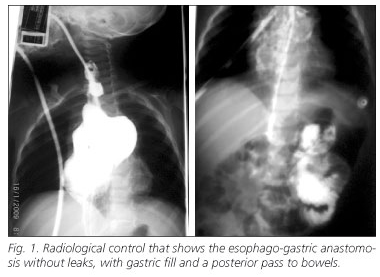
Female patient whom at the 24 h of born was diagnosed with a long gap esophagic atresia type I, a cervical esophagostomy and a feeding gastrostomy was made. At 8 months later a esphago-coloplasty with left colon was made on a retro-sternal way, putting in evidence a graft necrosis 72 h later of surgery, which was proceeded by a graft removal, staying only with the esophagostomy and feeding gastrostomy. Eight months later with a 16 months age a gastric ascent was performed with a prior Vautrin-Kocher maneuver and vasculature preservation of the stomach and a closure of the gastrostomy. A retro-sternal ascent was made again because the tunnel could be made without inconveniences. Ten days later of the post-surgery the patient presented saliva leaking via the cervical wound, of low quantification. A radiological control was performed that objectified a left lateral fistula of the esophago-gastric anastomosis. It was decided to re-operate, finding a longitudinal tearing of the esophagus corresponding to one of the suture points of approximately 0.5 mm which is repaired with a non absorbable suture. The patient was discharged from the hospital at the 10th day of the post-surgery prior to a radiological control (Fig. 1). Actually the patient is tolerating a soft oral diet.
Discussion
Type 1 esophageal atresia represents around 5% of all atresia which affect this organ. There is a consensus that while the reparation can be done on the esophagus, this is the best option, as with descent techniques with circular miotomies simple or doubles, the Kimura or Folker techniques or both (1). The challenge arises in those type 1 atresia with long gap, where there is an almost totally absence of thoracic esophagus, in this circumstances the replacement with colon, stomach, gastric or small bowel tubes (2,3,5) occupy a preponderant place in the therapeutic procedure, with an agreement that the coloplasties and the gastric ascents are probably the two better options (5). Being the choice of the organ to ascent a decision according to the surgeon experience, though similar analysis whit a the consult of 88 pediatric surgeons from the United Kingdom and other countries that most of them preferred the utilization of stomach with a satisfaction rate of 98% meanwhile with the use of esophagic elongation techniques there was a 76% of satisfaction (1). The results with the use of gastric or small bowel tubes have been disappointing (2).
Concerning the complications, the trend is to divide them in minor and major, and earlier and later (3).
Fistulas, total anastomotic dehiscence, stenosis, delayed stomach dumping, reflux and necrosis or ischemic disturbance of the ascended organ, are some of them (2,3,5). The ascended organ necrosis happens around 1-2% on the grafted patients (6), which makes this case more uncommon, after the coloplasty necrosis, the patient was left with the cervical esophagostomy and the feeding gastrostomy, the possibility of a gastric ascent, even knowing that the stomach was manipulated for the collocation of the feeding probe, was chosen. Moreover it was chosen again the ascent in a retro-sternal way, the same which was successful, achieving, even though the small cervical fistula that involved just one suture point, a good evolution and posterior discharge of the patient. It still to be know the prolonged follow up of the patient and the possibility of further complications like stenosis, reflux or delayed dumping.
Finally and coinciding with some authors reports (1), we have the impression that in those cases where the ascension of an organ is mandatory in the treatment of long gap atresia, the stomach is the best option, fundamentally because of its location, it is a more noble organ at the time of the anastomosis making and we have the sensation that vasculature can be identified and preserved better.
G. A. Nari, J. García-Luevano, C. Guerrero-Huerta and R. Barragán-Reveles
Surgery Department. Hospital Tercer Milenio -ISEA. Aguascalientes, Mexico
References
1. Ron O, De Coppi P, Pierro A. The surgical approach to esophageal atresia repair and the management of long-gap atresia: results of survey. Semin Pediatr Surg 2009; 18: 44-9. [ Links ]
2. Bax KM. Jejunum for bridging long-gap esophageal atresia. Semin Pediatr Surg 2009; 18: 34-9. [ Links ]
3. Bagolan P, Iacobelli B, De Angelis P, di Abriola GF, Laviani R, Trucchi A, et al. Long gap esophageal atresia and esophageal replacement: moving toward a separation? J Pediatr Surg 2004; 39: 1084-90. [ Links ]
4. Arul GS, Parikh D. Oesophageal replacement in children. Ann R Coll Surg Engl 2008; 90: 7-12. [ Links ]
5. Ahmad SA, Sylvester KG, Hebra A, Davidoff AM, McClane S, Stafford PW, et al. Esophageal replacement using the colon: is it a good choice? J Pediatr Surg 1996; 31: 1026-30. [ Links ]
6. Andrés AM, Burgos AL, Encinas JL, Suárez O, Murcia J, Olivares P, et al. What can we do when a esophagocoloplasty fails? Cir Pediatr 2007; 20: 39-43. [ Links ]











 texto en
texto en