Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.3 Madrid mar. 2010
LETTERS TO THE EDITOR
A paraduodenal hernia (Treitz's hernia) causing acute bowel obstruction
Obstrucción intestinal aguda causada por hernia paraduodenal (hernia de Treitz)
Key words: Internal hernia. Paraduodenal hernia. Treitz's hernia. Computed tomography.
Dear Editor,
Paraduodenal hernias, also called Treitz's hernia, are unusual causes of intestinal obstruction and account for 0.9% of all intestinal obstructions (1). Paraduodenal hernias constitute half of all internal abdominal hernias and occur when the small bowel herniates into the paraduodenal fossa with manifestation of intestinal obstruction (2). Specific clinical signs are often absent, leading to the frequent delay of correct diagnosis, with bowel necrosis resulting in up to 20% of patients (3). Herein, we present our case to increase the awareness of Treitz's hernia and suggest the early CT scan intervention may be helpful to make the preoperative diagnosis of paraduodenal hernia.
Clinical case
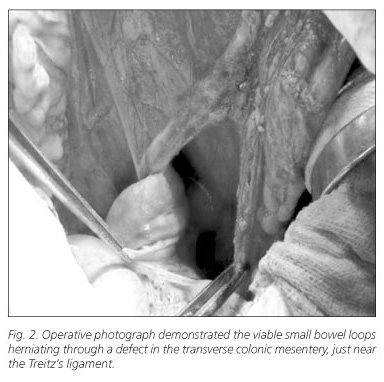
A 30-year-old male presented to the emergency department with a 1-week history of intermittent abdominal pain and non-bilious vomiting. His vital signs revealed temperature of 37.2 oC, pulse of 110/min and blood pressure of 116/68 mmHg. Physical examination showed a distended and muscle guarding abdomen without rebounding tenderness, particularly in the periumbilical region while increased bowel sound was noted. The blood tests showed white blood count of 8,700/ul with 85% segmented neutrophils. Plain film of the abdomen showed dilated small bowel loops in the central abdomen. Computed tomography of the abdomen showed encapsulation of dilated small bowel loops and looping of venous branches of the superior mesenteric vein in the central abdomen (Fig. 1). The intestinal obstruction was diagnosed and internal hernia was highly suspected. The patient was admitted and received the conservative treatment with nasogastric (NG) drainage tube and intravenous fluid support. However, the obstruction failed to resolve and his abdomen became progressively distended with massive output from NG tube. Subsequently, the patient underwent laparotomy under the impression of total intestinal obstruction. We found a large defect in the transverse mesocolon, near Treitz's ligament region and almost the entire small bowel was herniated into this defect, compatible with a paraduodenal hernia (Fig. 2). Lysis of adhesion, reduction of hernia and repair of mesentery defect were done. Postoperative course was uneventful. The patient was discharged on the 5th post-operative day and experienced no further symptoms.
Discussion
Paraduodenal hernia is an unusual cause of small bowel obstruction. Paraduodenal hernia accounts for about 30-53% of all internal hernias, which defined by Treitz in 1857 (1). Vague symptoms of paraduodenal hernia, caused by either partial or complete intestinal obstruction, include nausea, vomiting and abdominal pain. Physical examination may be normal, unless the hernia produces a mass or causes intestinal obstruction.
Since internal hernias are uncommon and have non-specific clinical features, preoperative diagnosis is difficult. Plain abdominal radiography may demonstrate a distended, fluid-filled stomach or reveal dilated loops of small bowel in an ovoid mass. Clustering of small bowel loops at the level of the ligament of Treitz or behind the pancreas may be seen on computerized tomography, with the sac providing a well-circumscribed edge (4). Early laparotomy is mandatory because obstruction of the entrapped bowel can lead to ischemia and perforation with a high mortality (5). The steps of operation include adequate incision, reduction of the hernia content, repair of the defect and avoiding injury to the mesenteric vessels.
Although internal hernias are uncommon as the primary etiology of mechanical small bowel obstruction, they should be considered in patient with obstructive symptoms, especially in younger people without previous abdominal surgery. In addition, image studies of CT should be obtained immediately to provide more information while the diagnosis of internal hernia is suspected. Surgical intervention is indicated for patients with intestinal obstruction or high risk of incarceration. Early diagnosis and prompt treatment prevent further complications and prolonged hospitalization.
C. T. Lin, K. F. Hsu, Z. J. Hong, J. C. Yu, C. B. Hsieh, D. C. Chan, M. L. Shih and G. S. Liao
Division of General Surgery. Department of Surgery. Tri-Service General Hospital. National Defense Medical Center. Taipei, Taiwan. Republic of China
References
1. Khan MA, Lo AY, Vande Maele DM. Paraduodenal hernia. Am Surg 1998; 64: 1218-22. [ Links ]
2. Hirasaki S, Koide N, Shima Y. Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to jejunal strangulation. J Gastroenterol 1998; 33: 734-8. [ Links ]
3. Nishida T, Mizushima T, Kitagawa T. Unusual type of left paraduodenal hernia caused by a separated peritoneal membrane. J Gastroenterol 2002; 37: 742-4. [ Links ]
4. Warshauer DM, Mauro MA. CT diagnosis of paraduodenal hernia. Gastrointest Radiol 1992; 17: 13-5. [ Links ]
5. Davis R. Surgery of left paraduodenal hernia. Am J Surg 1975; 129: 570-3. [ Links ]