Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.4 Madrid Abr. 2010
LETTERS TO THE EDITOR
Schwannoma of the rectum: report of a case and review of the literature
Schwannoma de recto: comunicación de un caso y revisión de la literatura
Key words: Schwannoma. Rectum. Perianal intersphincteric approach. Immunohistochemistry.
Dear Editor,
Schwannoma is well-known as a benign tumor originating from the Schwann cells, which produce insulating myelin sheath to cover peripheral nerves. It could occur in any nerve region, typically in the extremities, spinal cord and central nervous system (1).
In the literature, only few cases of rectal schwannoma have been reported (2-8). The surgical approaches, including abdominoperineal resection, transanal excision, perianal intersphincteric excision and transanal endoscopic resection were described for rectal schwannoma (2-8). In this report, we report one rare case of rectal schwannoma and review the published literatures. The surgical approaches and diagnosis are discussed.
Clinical case
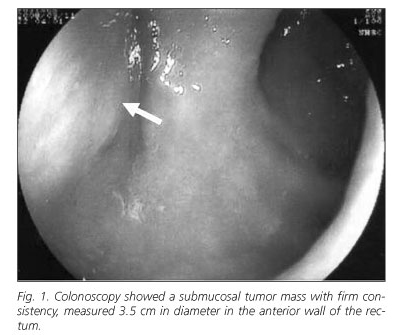
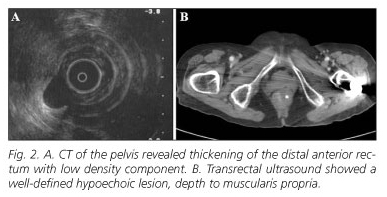
An 88-year-old woman presented with a one-month history of difficulty in defecation and frequently abdominal distension. She also complained the incomplete evacuation sensation following defecation. There were no changes in her appetite and body weight. In the medical history, she had diabetes mellitus but no gastrointestinal disease. Physical examination showed no remarkable finding on abdomen but a palpable, firm mass with intact mucosa at 1 o´clock on the rectal wall was demonstrated per rectum. Laboratory investigations and tumor markers as CEA, CA-199 and CA-125 were within normal limits. Colonoscopy disclosed a 3.5 cm submucosal mass in the anterior wall of the rectum with firm consistency, locating at 4cm from the anal verge (Fig. 1). Computed tomography (CT) of the pelvis revealed thickening of the distal anterior rectum with low density component (Fig. 2A). There was no enlarged lymph node to be identified. Transrectal ultrasound showed a well-defined hypoechoic lesion, depth to muscularis propria (Fig. 2B).
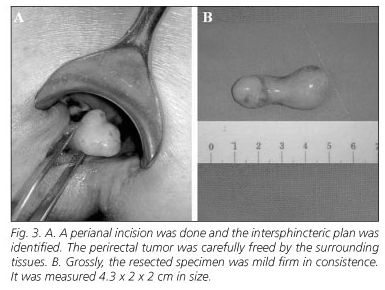
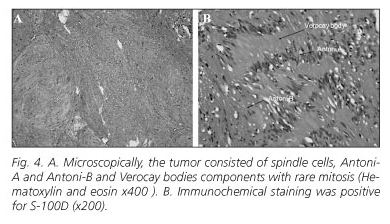
Considering the possibility of malignant submucosal tumor, removal of tumor was performed by perianal intersphincteric excision. We carried out this procedure in the Jacknife position, under heavy sedation and pudendal nerve block. An incision at 1 o´clock direction on perianal1 region was done and the intersphincteric plan was identified (Fig. 3A). The tumor was carefully freed by the surrounding tissues. The submucosal tumor was resected intactly (Fig. 3B). Grossly, the resected specimen was gray-yellow in color, mild firm in consistence and looked like lipoma in appearance. It was measured 4.3 x 2 x 2 cm in size. Microscopically, the tumor consisted of spindle cells, Antoni-A and Antoni-B and Verocay body components with rare mitosis (Fig. 4). Immunohistochemically, the tumor cells had strong positivity for S-100 protein, and negativity for CD34, c-kit protein and actin. The diagnosis of benign schwannoma was confirmed. The postoperative course was uneventfully without complication. The patient was well without evidence of recurrence at 9 months follow-up.
Discussion
Gastrointestinal schwannoma is categorized into gastrointestinal autonomic nerve tumor (GANT), which is originated from the myenteric plexus and accounting for 0.1% of benign gastrointestinal tumors (3). GANT is a subtype of gastrointestinal stromal tumors (GISTs), which are mesenchymal neoplasms and mostly occur in the stomach and small intestine (9). Gastrointestinal schwannomas are relatively rare and stomach is the most frequent site followed by small intestine (10). We herein present an extremely rare case of rectal schwannoma and review other published literatures (2-8) (Table I).
Schwannomas mostly present asymptomic masses or non-specific symptoms as pain, fatigue, and low grade fever. Patients with rectal schwannoma frequently complain of abdominal pain, difficulty in defecation, or only an asymptomatic rectal mass. Image modalities including transrectal ultrasound, CT, barium enema and colonoscopy are applied in the rectal tumors to gain tumor margin, size, depth of penetration, relationships with adjacent structures and the presence of metastatic spread. However, no definite criteria of image are obtained to diagnose the rectal schwannoma (10). Colonoscopy would offer a biopsy in rectal tumor. It is not mandatory for a submucosal lesion and may not confirm the cell type of the tumor or differentiate benign from malignant tumor. If, however, a biopsy is performed, it should be multiple and deep enough to reduce the false negativity of pathology. In our patient, a rectal submucosal tumor with smooth surface was clearly identified by colonoscopy and was evaluated by transrectal ultrasound and CT. Biopsy was not taken. Preoperative definite diagnosis was uncertain and malignancy could not be ruled out completely. Surgical resection was needed.
Although schwannomas are considered as benign tumors, the risk of recurrences was reported 30% in local recurrences (11) and 2% in distant metastases (12). The mainstay treatment for benign schwannoma is radical surgical excision. Unlike traditional surgical approach such as trans-sphinteric, trans-sacral, or trans-anorectal excision, we performed perianal intersphincteric approach and found the advantage of decreased perioperative bleeding, anal incontinence and less contamination, the same to the Pescatori et al. (7). Besides, due to aggressive growth of schwannoma, regular control of the patient during follow-up is important.
In conclusion, rectal schwannomas are extremely rare and only few cases have been reported in the literature, which are usually benign and carry a good prognosis. Perianal intersphincteric excision seems more safe and effective and it is less unlikely to carry complications such as perioperative bleeding and anal incontinence.
Drs. Hsu and Lin contributed equally to this work.
K. F. Hsu1, C. T. Lin1, C. C. Wu1, C. W. Hsiao1, T. Y. Lee1, C. M. Mai1,2, J. S. Jin3 and S. W. Jao1
1Division of Colon and Rectal Surgery. Department of Surgery. Tri-Service General Hospital. National Defense Medical Center. Taipei, Taiwan. Republic of China.
2Department of Surgery. Huailien Armed Forces General Hospital. Huailien, Taiwan. Republic of China.
3Department of Pathology. Tri-Service General Hospital. National Defense Medical Center, Taipei, Taiwan. Republic of China.
References
1. Brooks JJ. Disorders of soft tissue. In: Sternberg SS, editor. Diagnostic surgical pathology. New York: Raven Press, 1989. p. 178-89. [ Links ]
2. Kakizoe S, Kuwahara S, Kakizoe K, Kakizoe H, Kakizoe Y, Kakizoe T, et al. Local excision of benign rectal schwannoma using rectal expander-assisted transanal endoscopic microsurgery. Gastrointest Endosc 1998; 48: 90-2. [ Links ]
3. Maciejewski A, Lange D, Wloch J. Case report of schwannoma of the rectum--clinical and pathological contribution. Med Sci Monit 2000; 6: 779-82. [ Links ]
4. Miettinen M, Shekitka KM, Sobin LH. Schwannomas in the colon and rectum: a clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol 2001; 25: 846-55. [ Links ]
5. Bhardwaj K, Bal MS, Kumar P. Rectal schwannoma. Indian J Gastroenterol 2002; 21: 116-7. [ Links ]
6. Mulchandani MH, Chattopadhyay D, Obafunwa JO, Joypaul VB. Gastrointestinal autonomic nerve tumours--report of a case and review of literature. World J Surg Oncol 2005; 3: 46. [ Links ]
7. Pescatori M, Brusciano L, Binda GA, Serventi A. A novel approach for perirectal tumours: the perianal intersphincteric excision. Int J Colorectal Dis 2005; 20: 72-5. [ Links ]
8. Lee SH, Kim TO, Hwang SY, Ryu DY, Lee DH, Park WI, Kim GH, et al. A case of rectal schwannoma presenting with hematochezia. Korean J Gastroenterol 2006; 48: 195-9. [ Links ]
9. Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumours. Ann Chir Gynaecol 1998; 87: 278-81. [ Links ]
10. Rueda O, Escribano J, Vicente JM, Garcia F, Villeta R. Gastrointestinal autonomic nerve tumours (plexosarcomas). Is a radiological diagnosis possible? Eur Rad 1998; 8: 458-60. [ Links ]
11. Lauwers GY, Erlandson RA, Casper ES, Brennan MF, Woodruff JM. Gastrointestinal autonomic nerve tumours. A clinicopathological, immunohistochemical and ultrastructural study of 12 cases. Am J Surg Pathol 1993; 17: 887-97. [ Links ]
12. Das Gupta TK, Brasfield RD, Strong ET, Hajdn SI. Benign solitary schwannomas (neurilemmomas). Cancer 1969; 24: 355-66. [ Links ]