My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 n.7 Madrid Jul. 2010
LETTERS TO THE EDITOR
Kikuchi-Fujimoto, abdominal tumor as atypical location
Kikuchi-Fujimoto, localización atípica como tumoración abdominal
Key words: Kikuchi-Fujimoto. Histiocytic necrotizing lymphadenitis. Abdominal tumor.
Dear Editor,
Kikuchi-Fujimoto disease or histiocytic necrotizing lymphadenitis is a process characterized by fever and cervical lymphadenopathy, usually in young women. With the diagnosis of pancreatic tumor in an adult male patient, we report an unusual presentation of this condition.
Case report
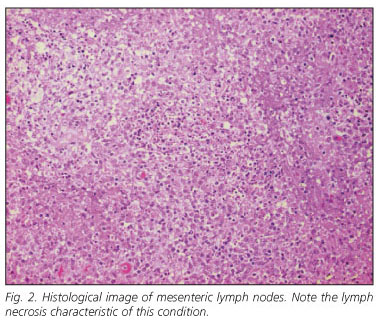
A 46 years old male with history of hypertension, smoking, psoriasis presented with epigastric discomfort radiated to the right hypochondrium and both renal fosses. Physical examination revealed no details. Laboratory tests showed a normal hemogram: ESR: 89; fibrinogen: 726.07; platelets: 527,000; biochemistry with PCR: 94; IgG: 1690; C3: 193 C4: 46.1, tumor markers (AFP, PSA, CEA and Ca 19.9), liver, thyroid, and rheumatologic tests, vitamins and urine were normal. Imaging tests (Fig. 1) reported the presence of a tumor in the head of the pancreas suggestive of adenocarcinoma, with radiological signs of infiltration into the duodenal wall and superior mesenteric vein. Bilateral subcostal laparotomy was performed and a 7-8 cm mass was observed covering the exit of the superior mesenteric artery and vein suggestive of a lymphomatous process. Intraoperative ultrasound revealed no lesions in the pancreas. Histological study (Fig. 2) showed histiocytic necrotizing lymphadenitis without granulocytic infiltration of mesenteric lymph node. The patient did not receive any medical or surgical treatment. The patient remained asymptomatic 24 months following with negative radiological study.
Discussion
Histiocytic necrotizing lymphadenitis is an uncommon condition that develops with fever and lymphadenopathy predominantly in the cervical region. It was originally described by Kikuchi (1) and Fujimoto et al. (2), in 1972, in young Japanese women, but later it has also been described in males of different ethnic and racial groups, with varying age ranges (3). Its etiology is unknown, and the histopathological study and evolution is self-limiting and benign. This condition distinguishes this rare pathology from other more serious diseases.
Clinical presentation, course and histological changes suggest an immune response of T cells and histiocytes against various infectious agents (4). It has also been associated with histological features of systemic lupus erythematosus (SLE), behaving as a disease SLE-like. The most common presentation is the appearance of laterocervical lymphadenopathy although it may appear in other nodal regions (3). Fever, present in 30-50% of patients, is often accompanied by systemic symptoms such as weight loss, vomiting, diarrhea and, occasionally, chest and abdominal pain, splenomegaly and hepatomegaly and may be related to abdominal lymphadenopathy (5).
Physical and analytical data are not usually relevant, except for a nonspecific slight thrombocytopenia, neutropenia with lymphomonocitosis, elevation of erythrocyte sedimentation rate (ESR) (3,5). Imaging tests do not provide differences from other lymphadenopathies (3), although sometimes, as in our patient may be confused with other malignant processes.
Definitive diagnosis is achieved by histopathological study of lymph node. We recommend obtaining an open biopsy, as the fine-needle aspiration (FNA) can often lead to misdiagnosis, if it is not performed by an experienced pathologist (6). Differential diagnosis is mandatory with SLE, lymphoma, and mononucleósicos syndromes (6,7). Other entities to consider are Kawasaki disease, metastatic carcinoma (4,7) and acute necrotizing lymphadenitis. Microscopic examamination usually shows patchy areas constituted by plamocitoides cells, histiocytes and immunoblasts mixed with cellular debris, eosinophils and basophils. A common finding is the absence of neutrophils with a progressive increase of histiocytes (3).
A self limited course of the illness, usually with spontaneous resolution of symptoms within the first six months is observed, as it was in our case. Treatment is generally symptomatic with non-steroidal anti-inflammatory drugs although severe or persistent cases may benefit from corticosteroid and immunosuppressors agents (6). Follow-up is essential for some years due to possibility of recurrence, progression to SLE (7) or fatal development.
In summary, surgeons must be aware of the Kikuchi-Fujimoto disease whenever atypical abdominal pain, tumor mass, and non-specific radiological and laboratory findings are present in a given patient. Definitive diagnosis has always to be made by histological examination of lymph nodes.
D. González-Ballester1, G. Blanco Fernández1, M. Tejero García1, J. Márquez Rojas1,
F. Botello Martínez1, G. Solórzano Peck1 and I. Catalina Fernández2
1Department of Hepatobiliopancreatic Surgery and Liver Transplant, and 2Pathology. Hospital Infanta Cristina. Badajoz, Spain
References
1. Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes. A clinico-pathological study. Acta Haematol 1972; 35: 379-80. [ Links ]
2. Fujimoto Y, Kojinia Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis. A new clinicopathological entity. Inter Med 1972; 41: 323-6. [ Links ]
3. Blanco Fernández G, Esteban Duran E, Zarallo Durán L, Núñez Núñez R, Blesa Sánchez E. Kikuchi-Fujimoto disease in the inguinal region. An Esp Pediatr 2002; 56(2): 193-4. [ Links ]
4. Radhi JM, Skinnider L, McFadden A. Kikuchi's lymphadenitis and carcinoma of the stomach. Journal of Clinical Pathology 1997; 50(6): 530-1. [ Links ]
5. Fitzsimmons PR, Akpan A, Michael B. Kikuchi-Fujimoto disease as a rare cause of fever of unknown origin in a septuagenarian. Age and ageing. Oxford 2008; 37(2): 233-4. [ Links ]
6. Mannarà GM, Boccato P, et al. Histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto Disease) diagnosed by Fine Needle Aspiration Biopsy. ORL: Journal for Oto-Rhino-Laryngology and Its Related Specialties. Basel: Nov/Dec 1999; 61(6): 367-71. [ Links ]
7. Hsin-Ching L, Chih-Ying SU, et al. Kikuchi's disease: a review and analysis of 61 cases. Otolaryngology - Head & Neck Surgery 2003; 128(5): 650-3. [ Links ]











 text in
text in