Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.9 Madrid sep. 2010
LETTERS TO THE EDITOR
A strange duodenal lesion
Una lesión duodenal extraña
Key words: Inverted duodenal diverticulum. Submucosal-like lesion. Hemorrhage.
Dear Editor:
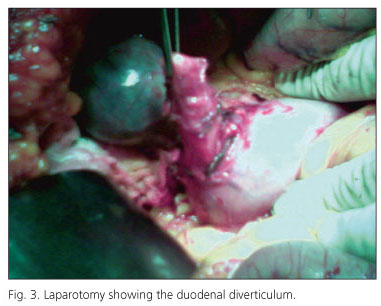
We study the case of a 72 years old woman, with a past history of osteoarticular degenerative disease and recent non-steroidal anti-inflammatory drug (NSAID) intake, who was admitted to our emergency department with a first episode of tarry stools. She was hemodinamically stable with a hemoglobin level of 9 g/dL. Upper gastrointestinal endoscopy (UGIE) identified, on the posterior wall of the first portion of the duodenum, an elevated, oval lesion of 15 mm diameter, with regular mucosa, a central depression hematin covered and hard consistency when probed with forceps biopsy (Fig. 1). Biopsies were taken and revealed a normal architecture with mild inflammation in the lamina propria. Endoscopic ultrasonography (EUS) showed a submucosal lesion, well defined by the muscular layer, without regional lymphadenopathies (Fig. 2). She was submitted to endoscopic submucosal tumorectomy by standard snare polypectomy (1) which was complicated with perforation. It was not possible to retrieve the specimen as it immediately passed into the distal duodenum. The patient underwent urgent laparotomy which revealed a sacular and oval structure, with 3 x 4 cm, opened in the extremity (Fig. 3). A diagnosis of an inverted duodenal diverticulum was made and diverticulectomy was performed. Histology of the operative specimen revealed a true diverticulum, with duodenal wall constituted by all four layers. Patient recovery was rapid and uneventful.
Discussion
The first documented report of a duodenal diverticulum was made by Chomel in 1710 (2). These structures can be classified into intra- or extraluminal diverticula and can have a congenital or acquired origin (3,4). Most extraluminal duodenal diverticula are acquired, consisting only of mucosal layers herniating through the muscular wall by pulsion or tractional mechanisms, and are a very common entity that can be present in up to 25% of the general population with increasing age (5-7). The duodenum is the second site after the colon regarding the frequency of diverticula (4,7,8). Approximately 70% of them are within 2 cm of the Vater ampulla and are termed juxtapapillary (4,8). Only 4% arise on the lateral duodenal wall (5,8). The great majority are asymptomatic and less than 10% can complicate with inflammation, bleeding, pancreatitis, perforation, common bile duct or duodenal obstruction (4,5,7,8). NSAIDs intake can favor inflammation and ulceration, leading to hemorrhage (5,7,9).
This case was a true diverticulum, with all the four wall layers, probably with a congenital origin. The patient did not had previous history of gastrointestinal symptoms and symptoms arose after taking NSAID, so this was probably the precipitating factor, as previously described in the literature.
The head of the diverticulum may prolapse into the lumen, causing a misleading macroscopic appearance, resembling a polypoid lesion, offering a true diagnostic challenge (10-15). This phenomenon has been described with Meckel diverticula (16) and appendiceal intussusception (17). However, references on inverted bowel diverticula in the endoscopic literature are limited. There are a few reported cases, concerning inverted duodenal (5) and colonic diverticulum (10-15) diagnosed by UGIE. This "polypoid lesion" is described as being voluminous, soft, pliable, congestive, broad stalked, easily indented when probed with forceps biopsy, dimpling at the site of invagination, presenting the characteristic "pillow sign" with radiating folds and disappearing with application of gentle air insufflation (10-15). The first recorded inadvertent endoscopic diverticulectomy of an inverted sigmoid diverticulum was made in 1982 (14). It is referred that EUS may help to further characterize these lesions (18).
In our case, the polypoid lesion was a truly misleading lesion. Not only the lesion did not behaved as previously described, as it was not a soft, pliable, easily indented lesion, but also gave a false image on the EUS, simulating a submucosal lesion. We believe that this was related to inflammation at the ostium of the diverticulum creating stenosis and trapping it firmly, giving a false submucosal image.
To our knowledge no cases of an inverted duodenal diverticulum simulating a submucosal lesion have ever been reported. This case demonstrates that, despite its rarity, inverted duodenal diverticulum should be considered in the differential diagnosis of polypoid structures.
P. Peixoto1, P. Amaro1, A. Sadio1, P. Figueiredo1, N. Almeida1, H. Gouveia1, L. Coutinho2, A. Barros2, M. R. Silva3 and M. C. Leitão1
1Gastroenterology Department, 2Surgery 1 Department and 3Pathology Department. Coimbra University Hospital. Portugal
References
1. Shim CS, Jung IS. Endoscopic removal of submucosal tumors: preprocedure diagnosis, technical options, and results. Endoscopy 2005; 37: 646-54. [ Links ]
2. Maingot R. Gastric and duodenal diverticula. In: Maingot R. Abdominal operations. New York: Appleton-Century-Crofts; 1980. p. 141-56. [ Links ]
3. Sleisenger MH, Feldman M, Scharschmidt BF. Sleisenger & Fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/management. 8th ed. Philadelphia: WB Saunders; 2006. p. 470-1. [ Links ]
4. Graur F, Bala O, Bodea R, Geczi-Toth I, Vlad L, Iancu C. Laparoscopic resection of duodenal diverticulum. A case report. Rom J Gastroenterol 2005; 14: 405-8. [ Links ]
5. Mendelson RM, Shepherd HA, Mitchell A. "Inverted" diverticulum mimicking an ulcerated duodenal tumour. Br J Radiol 1984; 57: 426-30. [ Links ]
6. Rodríguez S, Ossorio J. Divertículo duodenal congénito extraluminal. Cir Pediatr 2004; 17: 202-4. [ Links ]
7. Mahajan Sanjay K, Kashyap Rajesh, Chandel Upender K, Mokta Jatinder, Minhas Satinder S. Duodenal diverticulum: review of literature. Indian Journal of Surgery 2004; 66: 140-5. [ Links ]
8. Coelho JC, Sousa GS, Salvalaggio PR. Laparoscopic treatment of duodenal diverticulum. Surg Laparosc Endosc 1999; 9: 74-7. [ Links ]
9. Mahajan SK, Vaidya P, Sood BR, Gupta D, Sharma A. Duodenal diverticular haemorrhage in a patient taking NSAID. J Assoc Physicians India 2003; 51: 416-8. [ Links ]
10. Yusuf SI, Grant C. Inverted colonic diverticulum: a rare finding in a common condition? Gastrointest Endosc 2000; 52: 111-5. [ Links ]
11. Dumas O, Jouffre C, Desportes R, Etaix JP, Barthélémy C, Audigier JC. Inverted sigmoid diverticulum: a misleading polyp. Gastrointest Endosc 1991; 37: 587-8. [ Links ]
12. Ladas SD, Prigouris SP, Pantelidaki C, Raptis A. Endoscopic removal of inverted sigmoid diverticulum-is it a dangerous procedure? Endoscopy 1989; 21: 243-4. [ Links ]
13. Shah AN, Mazza BR. The detection of an inverted diverticulum by colonoscopy. Gastrointest Endosc 1982; 28: 188-9. [ Links ]
14. Schuman BM. Endoscopic diverticulectomy in the sigmoid colon. Gastrointest Endosc 1982; 28: 189-90. [ Links ]
15. Triadafilopoulos G. Images in clinical medicine. Inverted colonic diverticulum. N Engl J Med 1999; 341: 1508. [ Links ]
16. James GK, Berean KW, Nagy AG, Owen DA. Inverted Meckel's diverticulum: an entity simulating an ileal polyp. Am J Gastroenterol 1998; 93: 1554-5. [ Links ]
17. Ram AD, Peckham C, Akobeng AK, Thomas AG, David TJ, Patel L. Inverted appendix mistaken for a polyp during colonoscopy and leading to intussusception. J Cyst Fibros 2005; 4: 203-4. [ Links ]
18. Yoshida M, Kawabata K, Kutsumi H, Fujita T, Soga T, Nishimura K, et al. Polypoid prolapsing mucosal folds associated with diverticular disease in the sigmoid colon: usefulness of colonoscopy and endoscopic ultrasonography for the diagnosis. Gastrointest Endosc 1996; 44: 489-91. [ Links ]