Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.11 Madrid nov. 2010
LETTERS TO THE EDITOR
Upper digestive bleeding due to Dieulafoy's lesion during the postoperative period of aortocoronary bypass surgery in a patient treated with clopidogrel
Hemorragia digestiva alta por lesión de Dieulafoy durante el postoperatorio de bypass aorto coronario en un paciente en tratamiento con clopidogrel
Key words: Gastrointestinal Hemorrhage. Cardiovascular surgical procedures. Gastroscopy. Proton pump inhibitor. Clopidogrel. CYP219.
Palabras clave: Hemorragia digestiva. Cirugía cardiovscular. Gastrocopia. Inhibidores de la bomba de protones. Clopidogrel. CYP219.
Dear Editor,
Gastrointestinal complications of cardiac surgery are infrequent (0.3-3%) (1-3), but condition the prognosis of the patient. Upper digestive bleeding (UDB) is the most frequent complication of this kind. UDB is regarded as the expression of diffuse aggression on the body in the context of a risk situation, representing 28-31% of all gastrointestinal complications (4). In this setting, ulceration is the most common manifestation. The underlying etiopathogenesis would involve splanchnic hypoperfusion produced by the release of endotoxins, with immune alterations of the gastric mucosa and an increased risk of bacterial translocation (5). We present the case of a patient with UDB in the postoperative period of aortocoronary bypass surgery.
Clinical case
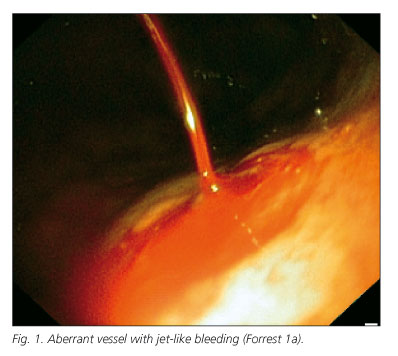
A 65-year-old male reported to the emergency service with hematemesis and melena. The personal history revealed ischemic heart disease with coronary revascularization and double bypass surgery without the use of an extracorporeal circuit (ECC) performed 10 days before in another center; dyspepsia not subjected to evaluation; arterial hypertension; dyslipidemia; and type 2 diabetes. The patient was being treated with clopidogrel, candesartan, hydrochlorothiazide, diltiazem, simvastatin, pentoxifylline, cinitapride and insulin. The physical examination revealed hypotension (70/50 mmHg), heart rate 110 bpm, and pale skin and mucosal membranes. The rest of the findings were normal. Blood testing in turn showed hematocrit 26.7%, hemoglobin 9.2 g/dl, MCV 84 fl, urea 18 mmol/l, platelet count 579,000, with normal values for aPTT and prothrombin time. Severe (9 points of the Rockall scale) UDB was thus diagnosed. Treatment was started with the water and electrolyte replacement and intravenous pantoprazole. Gastroscopy in turn revealed a 3-4 mm aberrant vessel with jet-like bleeding (Forrest 1a): 10 ml of adrenalin (1/10,000) and 3 ml of 1% polydocanol were injected, after which the bleeding subsided. Two hours later the patient developed another episode of hematemesis with hypotension (70/45 mmHg); as a result, endoscopy was again performed, with the placement of two clips targeted to the lesion, thereby securing permanent hemostasis. A total of 8 red cell concentrate units and two platelet units were transfused, with discharge on day 7 of admission to hospital.
Discussion
Ulcus-related upper digestive bleeding (UDB) is the most common complication during the postoperative period of cardiac surgery. Other complications are mesenteric infarction, ischemic colitis, cholecystitis and acute pancreatitis (4). Predisposing factors are a patient age of over 70 years, anticoagulation, a history of ulcus, Helicobacter pylori, renal failure, extracorporeal circuit duration, blood transfusion, the involvement of three coronary vessels, and NYHA class III-IV heart failure (1,4,6).
Antiplatelet drugs have been shown to be effective in preventing cardiovascular disease, reducing the incidence of cardiovascular events. An increasing number of patients require these drugs, and it is therefore necessary to know their adverse effects and interactions. The use of clopidogrel or aspirin in patients with a history of ulcus has not shown differences in terms of the risk of developing UDB. The use of double antiplatelet medication is associated with increased UDB rates. The combination of a proton pump inhibitor (PPI) and antiplatelet agents significantly lowers the risk of UDB; as a result, all patients with risk factors who are treated with antiplatelet drugs should receive a PPI. In our case, the patient was receiving clopidogrel without the association of a PPI.
Clopidogrel is a prodrug that is converted in the liver to the active metabolite thanks to the intervention of cytochrome P450, and in particular isoenzyme CYP2C19. The drug inhibits the platelet P2Y receptor for adenosine diphosphate - thereby irreversibly preventing platelet aggregation. The CYP2C liver cytochromes comprise an enzyme group among the P450 enzymes that metabolize 20% of all commonly used drugs, including clopidogrel and PPIs. There are four members in this group, CYP2C8, CYP2C9, CYP2C19 and CYP2C18 (9); of these, CYP2C9 and CYP2C19 are of clinical relevance (8). The CYP2C19 genotypes in turn are classified as representing "extensive metabolizers", "intermediate metabolizers" and "poor metabolizers" (7-9).
All PPIs are metabolized via the CYP2C cytochrome system, though not all in the same proportion. In this sense, omeprazole and esomeprazole are the PPIs most extensively metabolized via this route, followed by pantoprazole and lansoprazole. Rabeprazole is the drug least metabolized via this enzyme route (10). Studies analyzing the capacity of the different PPIs to suppress gastric acid have shown that the mean pH value with the administration of rabeprazole is not influenced by the CYP2C19 genotypes (10-12).
It has been shown that the antiplatelet action of clopidogrel decreases when added to omeprazole. This phenomenon is not observed with other PPIs (13). There is evidence suggesting that this loss of antiplatelet effect could have clinical repercussions. A case-control study has reported an increased risk of reinfarction among patients treated with clopidogrel plus PPIs - most such patients having been treated with omeprazole (14). Another study has reported no such risk when the prescribed PPI is pantoprazole - though no comparisons have been made versus the rest of the PPIs (15). We therefore consider that in patients treated with clopidogrel, contraindication cannot be extended to all PPIs, and that consideration is required of the pharmacokinetics of each individual drug, and of the clinical evidence, when selecting a concrete PPI.
L. Fernández-Sender, F. J. Martínez-Cerezo, S. Amorós, F. J. Tena, J. Marsal, D. Pascual
Servei d'Exploracions Complementàries i Aparell Digestiu. Hospital Universitari Sant Joan de Reus. Tarragona
References
1. Zacharias A, Schwan TA, Parentau GL, et al. Predictors of gastrointestinal complications in cardiac surgery. Tex Herat Inst J 2000; 27: 93-9. [ Links ]
2. Mangi A, et al. Gastrointestinal complications in patients undergoing heart operation: an análisis of 8709 consecutive cardiac surgical patients. Ann Surg 2005; 241: 895-901; Discusión 901-4. [ Links ]
3. Christenson JT et al. Postoperative visceral hypotension the common cause for gastrointestinal complications after cardiac surgery. Cardiovascular Surg 1994; 42: 152-7. [ Links ]
4. M. Ait Houssa, et al. Hémorragies digestives hautes après chirurgie cardiaque. Annales de Cardiologie et d'angeiologie 2007; 56: 126-9. [ Links ]
5. Abdellah A, et al. Complications digestives sévères après chirurgie cardiaque sous circulation extracorporelle. Can J Anesth 1999; 46(2): 114-21. [ Links ]
6. Christenson JT, et al. Gastrointestinal complications after coronay bypass grafting. J Torca Cardiovasc Surg 1994; 108: 899-906. [ Links ]
7. Mc Coll KE, Kennerly P. Proton pump inhibitors diferences emerge in hepatic metabolism. Dig Liver disease 2002; 34: 461-7. [ Links ]
8. Lim PMY, et al. CYP2C19 genptype and de PPIs focus on rabeprazole. J Gastroenterology and Hepatology 2005; 20: S22-8. [ Links ]
9. Ishiazi T, Horai Y, Review article: cytochrome P450 and the metabolism of proton pump inhibitors-emphasis on rabeprazole. Aliment Pharmacol Ther 1999; 13(Supl. 3): 27-36. [ Links ]
10. Robinson M. Review article: the pharmacodynamics and pharmacokinetics of proton pumps inhibitors- overview and clinical implications. Aliment Pharmacol Ther 2004; 20(Supl. 6): 1-10. [ Links ]
11. Adachi K, et al CYP2C19 genotype status and intragastric pH during dosing with lansoprazol or rabeprazol. Aliment Pharmacol Ther 2000; 14: 1259-66. [ Links ]
12. Sayito T, et al. Effects of rabeprazole, lansoprazole and omeprazole on intragastric pH in CYP2C19 extensive metabolizers. Aliment Pharmacol Ther 2002; 16: 1811-8. [ Links ]
13. Gilard M, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol 2008; 22: 256-60. [ Links ]
14. David N, et al. A populstion based study of the durg interaction between proton pump inhibitors and clopidogrel. CMAJ 2009; 7: 31-180. [ Links ]
15. Ho PM, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary sindrome. JAMA 2009; 301(9): 397-44. [ Links ]











 texto en
texto en