My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.1 Madrid Jan. 2011
Heterotopic gastric mucosa diagnosed by confocal endomicroscopy
Mucosa gástrica heterotópica diagnosticada mediante endomicroscopía confocal
M. López-Cerón Pinilla1, M. Jimeno Ramiro2, C. Rodríguez de Miguel1 y M. Pellisé Urquiza1
1Servicio de Gastroenterología, Institut de Malalties Digestives i Metabòliques;
2Servicio de Anatomía Patológica, Hospital Clínic de Barcelona. Spain
Key words: Heterotopic gastric mucosa, Confocal endomicroscopy.
Introduction
Confocal endomicroscopy (CE) is a new endoscopic tool that consists of a miniaturized confocal microscopy attached in the tip of a conventional endoscope. It allows high-resolution and high-magnification assessment of the mucosa providing images that can reliably predict histology in vivo.
Case
A 23-year-old woman was referred for a gastroscopy. She had a long history of upper abdominal pain, pyrosis and postprandial fullness without a complete response to proton-pump-inhibitors. She didn't relate any other relevant symptom or antecedent. Routine blood analysis revealed no abnormalities.
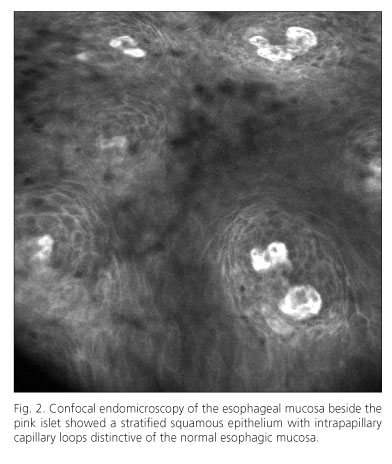
The exam was made with a confocal endomicroscope (Pentax EPK-1000, ISC-1000). White light examination found a small flat orange mucosal islet in the cervical esophagus adjacent to the upper esophagic sphincter. It had a diameter of approximately 30mm and beside it there was a 2mm satellite islet. The rest of the exam was normal. The islets were explored with CE after intravenous injection of 5 mL fluoresceine as a contrast agent. It provided images of small glands with round luminal openings and polygonal epithelial cells with cobblestone appearance distinctive of gastric mucosa. Intestinal metaplasia was ruled out since no goblet cells were visualized. The regular architecture of glandular epithelium and the microvasculature as well as the absence of a strong fluoresceine leakage indicated a benign process (Figure 1). Confocal images of adjacent mucosa showed normal esophagic epithelium with intracapillary papillary loops inside the papillae (Figure 2). Biopsies of the islet were obtained. Histopathologic examination confirmed the diagnosis showing gastric type superficial epithelium and oxyntic glands in deeper layers with no intestinal metaplasia or dysplasia (Figure 3).
Discussion
Heterotopic gastric mucosa (HGM) islets in the esophagus are generally located in its proximal portion, adjacent the upper esophagic sphincter. It can present as a single islet or as a group and its size varies from 0,2 to 4cm. Prevalence ranges from 0,1 to 10% in endoscopic studies but it is believed to be infraestimated because of the poor accessibility of its location. HGM is regarded as a result of incomplete embryologic epithelization process. Most of inlet patches are asymptomatic and the diagnosis is incidental. However they can produce symptoms related to acid production such as dysphagia and odinophagia due to chronic inflammation, ulceration and subsequently strictures and webs. Intestinal metaplasia, dysplasia and malignant progression to adenocarcinoma have also been reported (1).
Confocal endomicroscopy is a new endoscopic tool that consists of a miniaturized confocal microscope which is integrated in the tip of a conventional endoscope. A fluorescent agent is needed to explore the mucosal layers providing high-resolution and high-magnification images that can predict histology with a high accuracy level, as several studies have proven (2). The information obtained during ongoing endoscopy examinations allows making forthwith therapeutic decisions thereby saving biopsies. Hence, CE can be a useful tool when a mucosal islet is found in the upper esophagus allowing in vivo diagnosis of heterotopic gastric mucosa with no need of biopsies.
References
1. von Rahden BH, Stein HJ, Becker K, Liebermann-Meffert D, Siewert JR. Heterotopic gastric mucosa of the esophagus: literature-review and proposal of a clinicopathologic classification. Am J Gastroenterol. 2004; 99(3):543-51. [ Links ]
2. Kiesslich R, Neurath MF. Endoscopic confocal imaging. Clin Gastroenterol Hepatol. 2005; 3(7 Suppl 1):S58-60. [ Links ]
![]() Correspondence:
Correspondence:
Maria Pellisé Urquiza.
Gastroenterology Department.
Hospital Clínic Barcelona.
C/ Villarroel, 170. 08036 Barcelona.
E-mail: mpellise@clinic.ub.es
Received: 30-04-10.
Accepted: 01-06-10.











 text in
text in