My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.7 Madrid Jul. 2011
https://dx.doi.org/10.4321/S1130-01082011000700006
Non-IBD colitides: clinically useful histopathological clues
Colitis no relacionadas con la enfermedad inflamatoria intestinal: claves histopatológicas de utilidad clínica
Vincenzo Villanacci1, Stefania Manenti1, Elisabetta Antonelli2, Mariella Chiudinelli1, Vittorio Giuliano2 and Gabrio Bassotti2
1Department of Pathology. Spedali Civili, Brescia, Italy.
2Section of Gastroenterology and Hepatology. Department of Clinical and Experimental Medicine. University of Perugia. Italy
ABSTRACT
Apart from inflammatory bowel diseases (IBD), there are several other form of colitis that may resemble macroscopically IBD, entering the differential diagnosis. These forms are represented by infectious colitis, ischemic colitis, pseudomembranous colitis, colitis related to diverticular disease, colitis related to mucosal prolapse, drug colitis, allergic colitis, and microscopic colitis. However, to distinguish between these forms is not always easy, and it frequently requires a strict interrelationship between the pathologist and the gastroenterologist. Here we discuss the more frequent forms of non- inflammatory bowel diseases colitides, trying to give useful hints for helping the clinician to better understand the extent to which the pathologist is called to give a definitive response in the differential diagnosis of these entities.
Key words: Colon. Histopathology. Non-IBD colitides. Inflammation.
Introduction
Inflammatory and non inflammatory colitides represent a heterogeneous group of diseases, often difficult to diagnose and classify, whose diagnostic criteria are not always uniform. Moreover, epidemiological data are still relatively scarce, even for the best known entities. For instance, concerning inflammatory bowel diseases (IBD), there is evidence that in developed countries incidence rates have been increasing in recent years, reaching a plateau in most studies (1). Unfortunately, apart from infectious form of colitis (2), no such data are available for non-IBD colitides (3).
The diagnosis of various forms of colitides outside IBD embraces a miscellaneous group of entities that often represent a problem of differential diagnosis with IBD. Thus, the pathologist, in the daily routine practice, should keep well present these issues and try to give a precise classification in order to provide a correct diagnosis for a clinical targeted therapy.
As a starting point, it would therefore be wise to erase from one's pathologically-oriented diagnostic vocabulary such words as "non specific colitis" or "chronic non specific colitis". In fact, these terms seem to have no meaning and more often than not raise problems for the clinical gastroenterologist, since it may be safely stated that "all inflammation is non-specific" (Robert Riddell, personal communication).
It is of paramount importance that the clinician and the pathologist work as a well-integrated team; thus, the pathologist should receive accurate and detailed clinical information about the clinical problem (Table I), in addition to an adequate (at least three samples for each colonic segment, possibly including the terminal ileum, samples taken on both visible lesions and in the near, apparently normal mucosa) and correctly oriented number of biopsies (4).
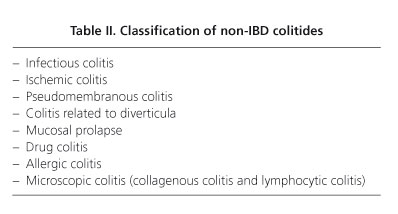
The various main nosological entities outside IBD are summarized in table II.
Below, for each entity, a few useful morphological elements borrowed from personal experience and literature will be provided for a more accurate diagnostic analysis in daily routine, but also to allow the clinician to better understand the extent to which the pathologist is called to give a definitive response in the differential diagnosis with IBD.
Infectious colitis
The morphological feature most useful for the exact classification of this condition is the careful evaluation of glandular architecture, since this morphological aspect is the discriminating factor between IBD and other forms of colitis (5,6).
In particular, the suspicion of infectious colitis is based on a complete preservation of the glandular architecture despite the presence of inflammatory infiltrate aggressive on glandular structures. The formation of cryptic abscesses is also present, as well as the reduction of mucous production. Another useful feature is the absence of basal plasmacytosis. Epithelial erosions or superficial irregularities (hairy appearance) are not particularly useful, in this setting, being commonly observed in many other colitides.
Small granulomas, mainly in the vicinity of the glandular elements, are often the result of rupture of cryptic gland abscesses and must be carefully evaluated in order to avoid a false diagnosis of Crohn's disease.
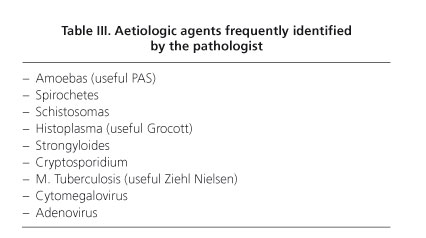
It must be always kept well in mind that the pathologist can only express compatibility (possibility or probability) with a diagnosis of an infective origin, as it is not often possible to offer sure evidence regarding the causative agent based only on pathological investigation. The situation may differ when one is faced with parasitic colitides, in which the identification of several infectious agents is often possible. Table III shows the infective agents frequently identifiable in routine pathological practice.
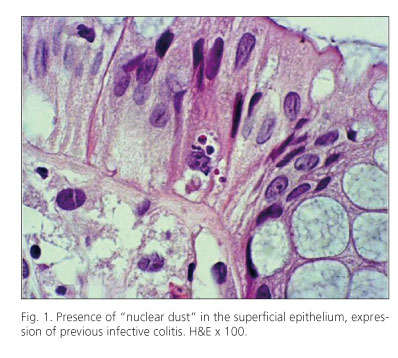
The morphological aspects described above are mostly pertinent to infectious colitis in the acute phase; in cases of previous infectious colitis it can be very useful to identify the so-called "nuclear dust" in the intraepithelial surface epithelium, which represents evidence of a previous inflammatory insult (Fig. 1).
It must also be taken into consideration the fact that a IBD, with its typical morphological elements, requires a time frame of at least two weeks to establish its histopathologic features; thus, it is extremely important for the pathologist to know at least the timing of symptoms' onset, to be usefully helped by the clinician to establish a differential diagnosis when the suspicion between IBD and an infective colitis arises.
Ischemic colitis
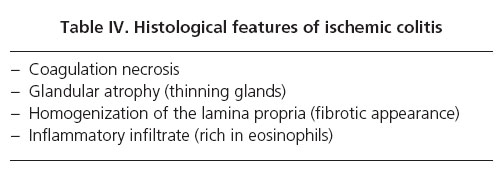
In this form of colitis, often found in middle aged or older subjects, and whose colonoscopic feature may mimic that of IBD (7) (Fig. 2A) the key diagnostic element is represented by the finding of coagulation necrosis and/or the presence of vascular thrombi. Beyond the obvious forms, one should pay particular attention, especially in young people (in whom a form of ischemic colitis must not be excluded a priori on the basis of age), to the segmentation of the lesions, the glandular atrophy, the homogenization of the lamina propria (Fig. 2B), and the presence of an inflammatory infiltrate rich in eosinophils (Table IV). When the latter is present, the genesis of the process can also recognize a pharmacological origin, especially in younger patients (use of oral contraceptives, kayexalate, cholestiramine, cocaine, etc.), and this fact should be pointed out by the pathologist to the clinician.
Pseudomembranous colitis
This form of colitis is known to be related to the use of antibiotics, with subsequent colonic colonization by Clostridium difficile; the toxins produced by this bacterium are responsible for the clinical symptoms. The morphological alterations are well known and subdivided in various stages (type I, II, and III); and types II and III enter the differential diagnosis with ischemic colitis. In type I, very rare today, are present small pseudomembranes composed of hyaline fibrinous material with occasional eosinophils typically located in the superficial epithelium between two crypts (Fig. 2, C and D). In type II, the aspect of the crypts, in which there is a reduction of the thickness of the epithelium (ghost crypts) and the presence of eosinophils within the lumen of the glandular elements are important features, helpful for the differential diagnosis with other entities. Type III is characterized by a severe damage of the mucosa with diffuse coagulative necrosis more similar to ischemic colitis. In this case the strict correlation with the clinician for a correct diagnosis is of absolute importance (8).
Colitis relates to diverticular disease
This entity usually does not represent a problem on diagnostic gross specimens, but may be very difficult to individuate on biopsy material. The morphological picture can be comparable to those found in infectious colitides (Fig. 3A), as these pathologic conditions share the same etiology; however, the possibility to suspect the presence of diverticula (when not specifically stated in the accompanying endoscopic report) is often related to the identification of cystic dilated or irregular glandular elements (Fig. 3B) that may represent a good indicator of their presence.
It must also not be forgotten that this condition often poses problems of differential diagnosis with Crohn's disease and, sometimes, with ulcerative colitis (9), especially in patients first diagnosed above 60 years of age (10); in these cases the collaboration with the clinician and the radiologist is of paramount importance.
Colitis related to mucosal prolapse
This represents a condition that is becoming increasingly common and whose detection and reporting can be particularly useful to the clinician for a correct therapeutic approach. Since the condition is related to a mucosal prolapse, the typical morphological elements are the presence of foamy histiocytes in the lamina propria of the rectum (Fig. 3C) and, above all, of muscle bundles penetrating into the lamina propria from the muscularis mucosae.
These two elements are complemented, in more severe forms, by coagulative necrosis and granulation tissue of ulcers related to the often associated condition of solitary rectal ulcer syndrome.
Drug colitis-allergic colitis
Both entities are very common today, and are considered together as they share many morphological similarities. The very few elements in the hands of the pathologist to establish a proper diagnosis are represented by a substantial architectural regularity of glandular architecture as the most important feature (11), beyond the identification of pseudomelanosis coli (a clear expression of laxative abuse), coupled to the careful evaluation of the location and the number of eosinophils. Under normal conditions, in fact, eosinophils are sparsely present only in the right colon; when they are present also in the left colon and, moreover, their number is higher than 60 in 10 fields of view at high magnification (Fig. 3D), the possibility of a form of eosinophilic colitis of probably allergic nature must be considered in children, whereas in adults this is more frequently related to a possible drug etiology (12). These possibilities should be always underlined in the histological report.
Microscopic colitis (collagenous colitis-lymphocytis colitis)
This entity is characterised clinically by chronic watery diarrhoea, with a macroscopically normal colonic mucosa -even though some suggestive abnormalities may be sometimes found that raise suspicion toward this disease (13)- where diagnostic histopathological features are seen on microscopic examination (14). However, some authors believe that the term microscopic colitis should be abandoned by the pathologist (and also by the clinician), because it is a misleading and inconclusive definition for both professional figures, in that it represents a sort of semantic umbrella for two actual entities, namely collagenous colitis and lymphocytic colitis (15,16). These conditions need to be correctly diagnosed to provide a clear direction to help clinicians to better target the treatment, even though these entities may often share important similarities, and probably represent morphologic different phases of one disease process.
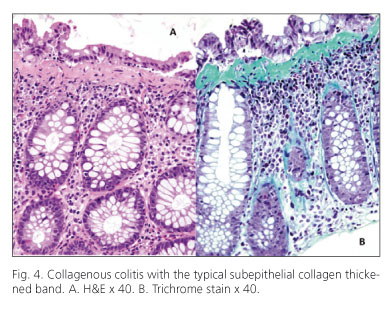
Concerning collagenous colitis, one should be careful not to confuse the thickening of the subepithelial connective band with a framework of ischemic colitis; in this case the implementation of Masson's trichrome stain may be useful to better visualize the important thickening of the connective tissue band (Fig. 4) in which context numerous CD3 positive T lymphocytes and eosinophils are often observed; in some cases these cell populations may obscure the thickened band in some sections, thus requiring careful assessment of numerous microscopic fields. Beyond cases of unknown etiology, many cases of collagenous colitis have been linked to the use of non steroidal anti inflammatory drugs and/or of other drugs, such as ticlopidine. Suspension of the culprit drugs has often led to the resolution of symptoms (that may reach up to 15-20 episodes of watery diarrhea per day).
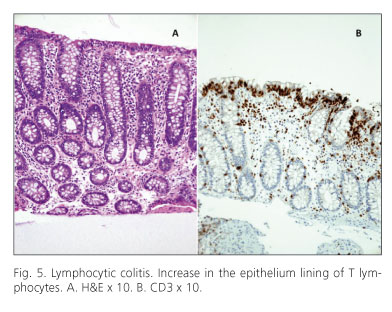
Lymphocytic colitis, considered another side of the same coin, is by definition linked to an increase in the epithelium lining of T lymphocytes CD3 and CD8 positive, with a cutoff of 30 lymphocytes per 100 epithelial cells (Fig. 5). Apart from forms also related to the use of drugs (ticlopidine, ranitidine, flutamide) (15-17), one must remember the close morphological similarity and correlation with celiac disease, which may be an associated condition. Thus, the identification of lymphocytic colitis should always prompt the clinician to exclude a concomitant celiac disease with the appropriate serological tests (18,19).
Concluding remarks
The above considerations do not have the pretense to be conclusive or binding, but we feel that in their own simplicity and practicality are to be mainly viewed as suggestions, as a stimulus for the pathologist not to be restricted to generic diagnoses, but to instead search the most precise and correct diagnosis that can at least allow the clinician a more specific diagnostic approach. At the same time, this increased precision could also allow the patient to better understand the different pathological entities outside IBD.
It is obvious that this is only possible through close cooperation between the pathologist and the clinician, with the purpose of receiving an adequate amount of clinical information and, above all, a sufficient number of biopsies. Thus, hopefully, we will no longer hear speaking of "non-specific therapy against a non-specific diagnosis"!
References
1. Gismera CS, Aladrén BS. Inflammatory bowel diseases: a disease(s) of modern times? Is incidence still increasing? World J Gastroenterol 2008;14:5491-8. [ Links ]
2. Navaneethan U, Giannella RA. Infectious colitis. Curr Opin Gastroenterol 2010, Sep 20. (Epub ahead of print). [ Links ]
3. Nielsen OH, Vainer B, Rask-Madsen J. Non-IBD and noninfectious colitis. Nat Clin Pract Gastroenterol Hepatol 2008;5:28-39. [ Links ]
4. Stange EF, Travis SPL, Vermeire S, Reinisch W, Geboes K, Barakauskiene A, et al.; for the European Crohn's and Colitis Organization (ECCO). European evidence-based Consensus on the diagnosis and management of ulcerative colitis: definitions and diagnosis. J Crohn's Colitis 2008;2:1-23. [ Links ]
5. Surawicz CM, Belic L. Rectal biopsy helps to distinguish acute self-limited colitis from idiopathic inflammatory bowel disease. Gastroenterology 1984;86:105-13. [ Links ]
6. Jenkins D, Balsitis M, Gallivan S, Dixon MF, Gilmour HM, Shepherd NA, et al. Guidelines for the initial biopsy diagnosis of suspected chronic idiopathic inflammatory bowel disease. The British Society of Gastroenterology Initiative. J Clin Pathol 1997;30:93-105. [ Links ]
7. Lozano-Maya M, Ponferrada-Díaz A, González-Asanza C, Nogales-Rincón O, Senent-Sánchez C, Pérez-de-Ayala V, et al. Usefulness of colonoscopy in ischemic colitis. Rev Esp Enferm Dig 2010;102:478-83. [ Links ]
8. Price AB. Pathology of drug-associated gastrointestinal disease. Br J Clin Pharmacol 2003;56:477-82. [ Links ]
9. Gledhill A, Dixon MF. Crohn's like reaction in diverticular disease. Gut 1998, 42: 392-5. [ Links ]
10. Hadithi M, Cazemier M, Meijer GA, Bloemena E, Felt-Bersma RJ, Mulder CJ, et al. Retrospective analysis of old-age colitis in the Dutch inflammatory bowel disease population. World J Gastroenterol 2008;14:3183-7. [ Links ]
11. Villanacci V, Casella G, Bassotti G. The spectrum of drug-related colitides: important entities, though frequently overlooked. Dig Liver Dis 2011 (in press). [ Links ]
12. Casella G, Villanacci V, Fisogni S, Cambareri AR, Di Bella C, Corazzi N, et al. Colonic left-side increase of eosinophils: a clue to drug-related colitis in adults. Aliment Pharmacol Ther 2009;29:535-41. [ Links ]
13. Nomura E, Kagaya H, Uchimi K, Noguchi T, Suzuki S, Suzuki M, et al. Linear mucosal defects: a characteristic endoscopic finding of lansoprazole-associated collagenous colitis. Endoscopy 2010;42(Supl. 2):E9-10. [ Links ]
14. Nyhlin N, Bohr J, Eriksson S, Tysk C. Microscopic colitis: a common and an easily overlooked cause of chronic diarrhoea. Eur J Intern Med 2008;19:181-6. [ Links ]
15. Geboes K, Villanacci V. Terminology for the diagnosis of colitis. J Clin Pathol 2005;58:1133-4. [ Links ]
16. Chang F, Deere H, Vu C. Atypical forms of microscopic colitis: morphological features and review of the literature. Adv Anat Pathol 2005;12:203-11. [ Links ]
17. Olesen M, Eriksson S, Bohr J, Järnerot G, Tysk C. Lymphocytic colitis: a retrospective clinical study of 199 Swedish patients. Gut 2004;53:536-441. [ Links ]
18. Fernández-Bañares F, Esteve M, Farré C, Salas A, Alsina M, Casalots J, et al. Predisposing HLA-DQ2 and HLA-DQ8 haplotypes of celiac disease and associated enteropathy in microscopic colitis. Eur J Gastroenterol Hepatol 2005;17:1333-8. [ Links ]
19. Casella G, Villanacci V, Di Bella C, De Marco E, Pagni F, Drera E, et al. Colonoscopic findings in coeliac disease on a gluten-free diet. Rev Esp Enferm Dig 2010;102:538-41. [ Links ]
![]() Correspondence:
Correspondence:
Gabrio Bassotti.
Clinica di Gastroenterologia ed Epatologia.
Ospedale Santa Maria della Misericordia.
Piazzale Menghini, 1.
06156 San Sisto (Perugia), Italy.
e-mail: gabassot@tin.it
Received: 13-09-10.
Accepted: 03-02-11.