Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.9 Madrid sep. 2011
https://dx.doi.org/10.4321/S1130-01082011000900009
Posterolateral Bochdalek diaphragmatic hernia in adults
Hernia diafragmática posterolateral de Bochdalek en el adulto
José Maximiliano Garófano-Jerez1,2, Juan de Dios López-González1, M.a Ángeles Valero-González2 and Manuel Valenzuela-Barranco3
1Department of Radiology and Physical Medicine. School of Medicine. University of Granada.
2Department of Radiodiagnosis. Hospital Universitario San Cecilio. Granada.
3Department of Internal Medicine. Facultad de Medicina. Universidad de Granada. Granada, Spain
ABSTRACT
Bochdalek hernias (BHs) are produced in the posterolateral area of the diaphragm. They are generally congenital, appearing in childhood, but are also detected in asymptomatic adult patients seeking medical attention for other reasons. Computed tomography (CT) or magnetic resonance imaging (MRI) is used for the correct diagnosis of the hernia type and for its localization, facilitating its management and the choice of treatment. We describe three cases of Bochdalek hernia, two on the right side and one bilateral, which was larger on the right than left side. All of these hernias contained only omental fat. In one patient, the right kidney was adjacent to the diaphragmatic defect but remained within the abdomen. The patients showed no symptoms and were not surgically treated. Examination by multi-slice CT with the possibility of coronal and sagittal reconstruction should be considered the standard method for diagnosing this entity. MRI in T1 is highly valuable to evaluate fat-containing chest lesions. The incidental finding of BH in asymptomatic adults is increasing, thanks to the wider application of new imaging techniques.
Key words: Bochdalek hernia. Congenital diaphragmatic hernia. Computed tomography. Magnetic resonance.
RESUMEN
Las hernias de Bochdalek se producen a través de la zona posterolateral del diafragma. Generalmente son congénitas y se presentan en la infancia, pero pueden verse también en la edad adulta en pacientes asintomáticos, que consultan por patologías diversas. El uso de tomografía computarizada o resonancia magnética permite el diagnóstico correcto del tipo y localización de la hernia, lo cual facilitará su manejo y la elección del tratamiento. Presentamos 3 casos clínicos, dos tenían una hernia de Bochdalek derecha, y, el otro caso es bilateral, siendo mayor la situada en el lado derecho. En todos nuestros casos, el contenido ha sido únicamente grasa omental. No obstante, en uno de ellos, el riñón derecho se situaba adyacente al defecto diafragmático, pero dentro del abdomen. Debido a la ausencia de sintomatología, nuestros pacientes no han sido tratados quirúrgicamente. La exploración mediante tomografía computarizada multicorte, con posibilidad de realizar reconstrucciones coronales y sagitales, debería ser considerada el método estándar para diagnosticar esta entidad. La resonancia magnética en T1 es muy valiosa en la evaluación de lesiones torácicas que contienen grasa. Para concluir, debemos resaltar que las hernias de Bochdalek en el adulto, asintomáticas, descubiertas de forma incidental, están siendo diagnosticadas cada vez con una mayor frecuencia gracias a los avances en las nuevas técnicas de imagen, permitiendo el diagnóstico correcto del tipo y localización de la hernia, lo cual facilitará su manejo y la elección del tratamiento.
Palabras clave: Hernia de Bochdalek. Hernia diafragmática congénita. Tomografía computerizada. Resonancia magnética.
Introduction
The presence of a weakened space or defect in the diaphragmatic muscle can allow some contents of the abdomen to enter into the thoracic cavity, forming a herniation. Diaphragmatic hernias (DHs) are most frequently produced in the esophageal (hiatal hernia) and paraesophageal hiatus (paraesophageal hernia) and posterolateral -Bochdalek hernia (BH)-, and anteromedial -Morgagni hernia (MH)- regions of the diaphragm (1-4).
The etiology can be congenital, due to alterations in diaphragm development, or acquired as the result of surgery, trauma, or infection. The causes of late-presenting hernias (i.e., in adults) include congenital herniation, penetrating or blunt trauma, physical effort (including sexual relationships), pregnancy, labor or delivery, sneezing or coughing episodes, and even the intake of a large amount of food (4-7). It has also been related to long-term complications of continuous ambulatory peritoneal dialysis (8).
Most congenital diaphragmatic hernias (CDHs) appear in the neonatal period with respiratory distress and can be life-threatening (6,9,10). However, cases have been reported outside this age group, usually in adults with non-specific or no symptoms (5,11-13). In Spain, the frequency (14) of a hernia or diaphragmatic agenesis diagnosis in the first three days of life was reported to be 2.15 per ten thousand in 2007 and has shown a linear tendency to decrease in subsequent years (2.800/000 in 1980-1985; 1.460/000 in 1986-2006). BHs are more frequent than MHs (2,9,15), to the extent that CDH and BH have become virtually synonymous (4). The estimated prevalence of BH ranges from 0.17 to 12.7 per cent (2,5,7,9,10,16), with the higher values being detected in CT-based studies. HBs are more frequent on the left (50-90%) than on the right side (6,11), which has been attributed to the earlier closing of the right pleuriperitoneal canal during normal development (2,9) and the protective effects of the liver on the right side (6). Hernias are bilateral in around 15% of reported cases (5,11). There can sometimes be a small diaphragmatic defect without hernia. There have been no cases of lung hernia through a diaphragmatic opening (11).
Most published cases of MH and BH diagnosis and repair are in children, with only 5 per cent being reported in adults (12). Although a diaphragmatic dysgenesis is widely considered to be the origin of CDH, only 10 per cent of CDH patients were found to have chromosomal anomalies (17).
BHs can affect both sides of the body, in the region where the lateral arcuate ligaments of the diaphragm curve, covering the quadratus lumborum muscles, and laterally fix on either side of the twelfth rib and medially to the transverse process of L1 (9,10,18).
Case reports
Case report 1
An 82-yr-old man was hospitalized for intense epigastric pain that did not respond to analgesic medication; he also reported persistent constipation with altered bowel habit. He suffered from senile heart disease, aortic sclerosis and venous insufficiency in lower limbs. He had a history of chronic obstructive pulmonary disease (COPD) and a major atrial fibrillation treated with actocortin in the emergency area, which has not recurred. He subsequently underwent surgery for bladder cancer (grade I papillary transitional carcinoma involving the corium).
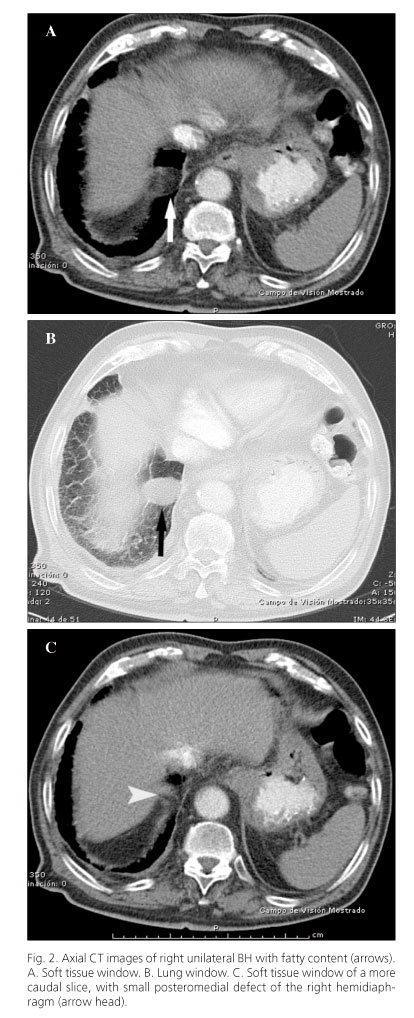
Conventional posteroanterior chest X-ray (Fig. 1) showed no findings of interest. Chest-abdominal computer tomography (CT) study revealed some paraseptal bullae with pulmonary emphysema, increased density of residual appearance in the apex of the right lung, interstitial pattern with bibasal predominance, cardiomegaly (at the expense of both atria), mitral and aortic valve calcifications, small subcarinal lymph nodes, and possible right hilar lymph nodes. There were also mild pleural thickenings with right predominance and chronic appearance. Additionally, there was a small right BH with fatty content of around 25 mm (Figs. 2 A-C). In the abdominal region, a small vesical diverticulum (12 mm) was observed on the right lateral wall.
Case report 2
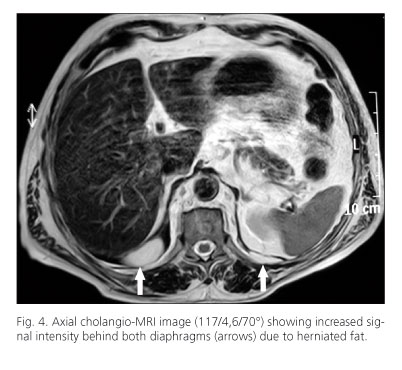
A 61-year-old male was hospitalized for epigastric pain and vomiting, which were interpreted as a biliary colic. However this diagnosis could not be confirmed by X-ray, which showed no findings of interest (Figs. 3 A and B). Cholangio-MRI (Fig. 4) and abdominal-pelvic MRI studies (Fig. 5) revealed a previously undiagnosed bilateral BH.
Three years earlier, he had been diagnosed with moderately differentiated rectal adenocarcinoma (pT3 pN0), which was treated with surgery, chemotherapy, and radiotherapy.
At his latest examination, he was disease-free with normal blood-count, although he showed elevated levels of total cholesterol, 278 mg/dL (upper limit: 200-239), triglycerides, 244 mg/dL (50-150), and LDL-cholesterol, 153 mg/dL (50-130).
Finally, chest-abdominal CT revealed small subpleural pulmonary nodules, a small hiatal hernia, and bilateral BH with fatty content (Figs. 6 A-C), which was larger on the right side (around 48 mm). In the abdominal region, there were small cysts in the renal parenchyma and a metal suture in the rectum from the previous surgery.
Case report 3
An 81-year-old female with respiratory insufficiency was hospitalized for a respiratory infection. Analytical results showed: leukocytosis of 21,530 leukocytes per µL (normal range, 4,800-10,800), with a shift to the left due to the presence of 18,900 neutrophils per µL (1,900-8,000); 100 mg/dL glycemia (70-100); 51.7 mg/dL uremia (10-50); 3.2 mEq/L K (3.8-5.2); 14.30 mg/dL PCR (0-0.8); and 65 ng/mL myoglobin (25-58).
Posteroanterior (Fig. 7A) and lateral (Fig. 7B) chest X-rays showed alveolar-interstitial lung involvement, with predominance in inferior lobules, as well as right posterior diaphragmatic lobulation. The lateral X-ray showed dorsal kyphosis and wedge-shaped vertebrae. Chest CT (Figs. 8 A-D) confirmed the presence of an interstitial "honeycomb" pattern of micro- and macro-cystic lesions, with peripheral, apical, and basal predominance and the presence of traction bronchiectasis, indicating an advanced stage of pulmonary fibrosis. The scan also showed a sliding hiatal hernia and right BH with fatty content.
Discussion
The diaphragm is formed between week 4 and 12 of gestation by four embryologic elements: septum transversum, pleuroperitoneal membranes, mediastinal dorsal mesentery of the esophagus, and muscles of the body wall (10,19). It has been hypothesized that the liver usually obstructs herniation through a possible defect on the right side. Furthermore, the right hemidiaphragm is completely formed before the left, because of the earlier closing of the right pleuroperitoneal canal when the intestine returns to the peritoneum from its rotation in the yolk sac (11), hence 70-90 per cent of all BHs, better described as posterior diaphragmatic defects (19), are on the left side (6), although Mullins et al. (5), in 2001, observed that 68 per cent were located on the right side. They also found a 14 per cent possibility of bilaterality.
We report three cases of BH, two on the right side and one bilateral in which the largest hernia is on the right side. The size of a BH is usually highly variable, from a few millimeters to occupying most of the thorax, and it is not necessarily related to the size of the diaphragmatic defect (5,11,20); 20 per cent of BHs are contained by a sac, and the remainder show direct communication between thorax and abdominal cavity (21). BHs typically contain omental fat, which can be accompanied by the stomach, spleen, colon, and even the small intestine (10,11,16,20,22,23). The involvement of the liver, gallbladder, pancreas, kidney, or retroperitoneal fat is rare (5), and there has been no report of a lung component in adult BH (10).
In all our cases, the content was omental fat alone. However, in one of them, the right kidney was adjacent to the diaphragmatic defect but inside the abdomen (Figs. 8B).
In newborns, the protrusion of the liver inside the right hemithorax is typically due to a CDH. In these cases, the liver will cause a mass effect and displace the mediastinum towards the left. However, if the mediastinum is not displaced, other less common causes for intrathoracic liver should be considered, such as primary right pulmonary hypoplasia (e. g. scimitar syndrome) or agenesis and hepatic- pulmonary fusion (24).
Most congenital BHs are associated with a respiratory insufficiency (21) that becomes evident during the first weeks of life, and they are among the most frequent causes of respiratory distress in neonates. In adults, most BHs are usually asymptomatic (16) and their detection is incidental, as in our three patients. Symptoms, if any, are typically imprecise. Patients usually report chest pain or gastrointestinal symptoms (5,7,13). A case was reported of a 23-yr-old woman in the second trimester of pregnancy with symptoms of retching, oliguria, and shortness of breath that were initially attributed to the pregnancy itself but finally proved to be caused by a left BH with acute gastric volvulus (25). One of our patients was hospitalized for intense epigastric pain, but its relationship with the BH could not be demonstrated. There have been rare reports of late presenting BH with gastric volvulus, spleen rupture, obstruction, and gastrointestinal perforation (23,25,26).
Congenital BHs can be diagnosed by ultrasound, even in the prenatal period, as a displacement of the mediastinum and a mass in the thorax of the fetus (2). Chest-abdominal X-rays of a neonate with BH and respiratory distress show a soft tissue mass in the thorax that reveals gas or hydro-air levels when the neonate swallows air. X-rays with radiopaque contrast may be useful before surgery to assess the herniated intestinal loops and their possible malrotation (10,22).
Occasionally, a BH can appear as a lesion with soft tissue density in the posterior area of the pulmonary base in lateral chest X-rays (6,11), which may be confused with a pulmonary lymph node adjacent to the diaphragm (27) or, as in one of our cases, with a posterior diaphragmatic lobulation (Figs. 7 A and B). Using CT, however, a BH can be readily differentiated from a diaphragmatic eventration or lobulation ("bosselation") by examining the continuity of the diaphragm muscle itself. In BH, the muscle always shows a break or defect, whereas it is always whole, though thinned, in the other two conditions (11).
In two of our patients, with known malignant disease, the predominant clinical indication for CT was to rule out metastatic disease, as reported by other authors (5).
Examination by multi-slice CT, with the possibility of coronal and sagittal reconstruction, should be considered the standard method to diagnose BH (5). Some authors recommended replacing conventional axial images with coronal reformatted images, because there are fewer images and less time is required for interpretation (28). However, it has been verified that the lack of familiarity of observers with coronal visualization may contribute to detection errors and the missing of defects (28).
CT and MRI studies are highly valuable for the assessment of fat-containing thoracic lesions (6), detecting, localizing, and identifying lesions and markedly reducing the time required for the differential diagnosis (Figs. 4 and 5). CT or MRI diagnosis can be definitive. In BHs, sagittal and coronal reformatted images can reveal the diaphragmatic defects and hernia contents (Figs. 8 C and D).
The treatment of incidental BH remains controversial (5). All DH types are assumed to have a congenital origin, but the clinical presentation, management, complications, and prognosis markedly differ between neonate and adult cases. The prognosis for late-presenting BH is usually more favorable (13,16), as in the present patients, who have shown no clinical or imaging changes after a follow-up of up to six years. Despite the generally symptom-free nature of incidental BH in adults, some authors recommend surgery, including hernia reduction and defect closure, arguing that the risk of tissue strangulation and even death warrants an aggressive approach (7).
The diagnosis of BH as an incidental finding in adulthood appears to be increasingly frequent. Given the growing prevalence of obesity in our society, there may be a connection between these phenomena, which would have public health implications (7).
The incidental finding of BH in asymptomatic adults appears to be increasing, largely due to the application of new imaging techniques. The use of CT or MRI offers greater precision in the diagnosis, localization and characterization of the hernia, facilitating its management and the choice of treatment.
References
1. Fultz PJ, Hampton WR, Skucas J, Sickel JZ. Diferencial diagnosis of fat-containing lesions with abdominal and pelvis CT. RadioGraphics 1993;13:1265-80. [ Links ]
2. Miller PA, Mezwa DG, Feczko PJ, Jafri ZH, Madrazo BL. Imaging of abdominal hernias. RadioGraphics 1995;15:333-47. [ Links ]
3. Pereira JM, Sirlin CB, Pinto PS, Casola G. CT and MR imaging of extrahepatic fatty masses of the abdomen and pelvis: techniques, diagnosis, differential diagnosis, and pitfalls. Radiographics 2005;25:69-85. [ Links ]
4. Arráez-Aybar LA, González-Gómez CC, Torres-García AJ. Morgagni-Larrey parasternal diaphragmatic hernia in the adult. Rev Esp Enferm Dig 2009;101:357-66. [ Links ]
5. Mullins ME, Stein J, Saini SS, Mueller PR. Prevalence of incidental Bochdalek's hernia in a large adult population. AJR 2001;177:363-6. [ Links ]
6. Gaerte SC, Meyer CA, Winer-Muram HT, Tarver RD, Conces DJ. Fat-containing lesions of the chest. RadioGraphics 2002;22:S61-S78. [ Links ]
7. Mullins ME, Saini S. Imaging of Incidental Bochdalek Hernia. Semin Ultrasound CT MRI 2005;26:28-36. [ Links ]
8. Stuart S, Booth TC, Cash JC, Goode JA, Harvey C, Malhorta A. Complications of continuous ambulatory peritoneal dialysis. RadioGraphics 2009;29:441-60. [ Links ]
9. Panicek DM, Benson CB, Gottlieb RH, Heitzman ER. The diaphragm: anatomic, pathologic, and radiologic considerations. RadioGraphics 1988;8:385-425. [ Links ]
10. Losanoff JE, Sauter ER. Congenital posterolateral diaphragmatic hernia in an adult. Hernia 2004;8:83-5. [ Links ]
11. Gale ME. Bochdalek Hernia: Prevalence and CT characteristics. Radiology 1985;156:449-52. [ Links ]
12. Richardson WS, Bolton JS. Laparoscopic repair of congenital diaphragmatic hernias. J Laparoendosc Adv Surg Tech 2002;12:277-80. [ Links ]
13. Cigdem MK, Onen A, Otcu S, Okur H. Late presentation of Bochdalek-type congenital diaphragmatic hernia in children: a 23-year experience at a single center. Surgery Today 2007;37:642-5. [ Links ]
14. Bermejo E, Cuevas L, Mendioroz J, Grupo Periférico del ECEMC, Martínez-Frías ML. Frecuencia de anomalías congénitas en España: vigilancia epidemiológica en el ECEMC en el periodo 1980-2007. Bol ECEMC Rev Dismor Epidemiol 2008;V,7:58-87. [ Links ]
15. Yoo E, Kim JH, Kim MJ, Yu JS, Cheng JJ, Yoo HS, et al. Greater and lesser omenta: normal anatomy and pathologic processes. RadioGraphics 2007;27:707-20. [ Links ]
16. Kinoshita F, Ishiyama M, Honda S, Matsuzako M, Oikado K, Kinoshita T, et al. Late-presenting posterior transdiaphragmatic (Bochdalek) hernia in adults: prevalence and MDCT Characteristics. Thorac Imaging 2009;24(1):17-22. [ Links ]
17. Pober BR. Overview of epidemiology, genetics, birth defects, and chromosome abnormalities associated with CDH. Am J Med Genet Part C Semin Med Genet 2007;145C:158-71. [ Links ]
18. Restrepo CS, Eraso A, Ocazionez D, Lemos J, Martinez S, Lemos DF. The diaphragmatic crura and retrocrural space: normal imaging appearance, variants, and pathologic conditions. RadioGraphics 2008;28: 1289-305. [ Links ]
19. Santamarina MG, Crespo SR, Baltazar AD, Volpacchio MM. Rol de la TC multicorte en las hernias diafragmáticas. Ensayo iconográfico. RAR 2009;73:421-32. [ Links ]
20. Liman ST, Topçu S, Okay E, Özerdem A, Çiftçi E, Özker E. Symptomless massive herniation: giant adult Bochdalek hernia. Inönu Üniversitesi Tip Fakültesi Dergisi 2006;13 (3):171-3. [ Links ]
21. Swain JM, Klaus A, Achem SR, Hinder RA. Congenital diaphragmatic hernia in adults. Semin Laparoc Surg 2001;8:246-55. [ Links ]
22. Raymond GS, Miller RM, Müller NL, Logan PM. Congenital thoracic lesions that mimic neoplastic disease on chest radiographs of adults. AJR 1997;168:763-9. [ Links ]
23. Temizöz O, Gençhellaç H, Yekeler E, Ümit H, Ünlü E, Özdemir H, et al. Prevalence and MDCT characteristics of asymptomatic Bochdalek hernia in adult population. Diagn Interv Radiol 2010;16:52-5. [ Links ]
24. Keller RL, Aaroz PA, Hawgood S, Higgins CB. MR imaging of hepatic pulmonary fusion in neonates. AJR 2003;180:438-40. [ Links ]
25. Palanivelu C, Rangarajan M, Maheshkumaar GS, Parthasarathi R. Laparoscopic mesh repair of a Bochdalek diaphragmatic hernia with acute gastric volvulus in a pregnant patient. Singapore Med J 2008;49(1):e26-e28. [ Links ]
26. Kumar A, Maheshwari V, Ramakrishnan TS, Sahu S. Caecal perforation with faecal peritonitis -unusual presentation of Bochdalek hernia in an adult: a case report and review of literature. World Journal of Emergency Surgery 2009;4:16. [ Links ]
27. Katsenos S, Kokkonouzis I, Lachanis S, Psathakis K. Right-sided Bochdalek hernia presenting as a solitary pulmonary nodule. Radiology Case Reports. [Online] 2008;2:114. [ Links ]
28. Kwan SW, Partik BL, Zinck SE, Chan FP, Kee ST, Leung AN, et al. Primary interpretation of thoracic MDCT images using coronal reformations. AJR 2005;185:1500-8. [ Links ]
![]() Correspondence:
Correspondence:
Juan de Dios López González Garrido.
e-mail: jdlopezg@ugr.es
Received: 17-11-10.
Accepted: 02-12-10.