My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.11 Madrid Nov. 2011
https://dx.doi.org/10.4321/S1130-01082011001100008
PICTURES IN DIGESTIVE PATHOLOGY
Ascaris lumbricoides as etiologic factor for pancreas inflammatory tumor
Ascaris lumbricoides como factor etiológico de tumor inflamatorio de páncreas
María Dolores Casado-Maestre, José María Álamo-Martínez, Juan José Segura-Sampedro, Elena Durán-Izquierdo, Luis Miguel Marín-Gómez, Carmen Bernal-Bellido, Gonzalo Suárez-Artacho, Juan Serrano-Díez-Canedo, Miguel Ángel Gómez-Bravo and Francisco Javier Padillo-Ruiz
Unit of Hepatobiliopancreatic and Transplant Surgery, Department of General Surgery and Digestive Diseases. Hospitales Universitarios Virgen del Rocío. Sevilla, Spain
Case report
A 58 years old male consulted to his practitioner due to long evolution and continuous abdominal pain with non constant diarrhea. His medical history includes chronic ischemic cardiopathy, atrial flutter, hypertension, bilateral hip prosthesis. A colonoscopy was performed finding no abnormalities. The scanner showed an infiltrative mesenteric mass of 7 x 14 cm with undefined margins which contacted with pancreatic cephalic portion and uncinate process (Fig. 1). A MRI dismissed local and linfovascular infiltration. The study was completed with a FNA cytology guided by EUS being positive for neoplastic cells, suggesting pancreatic adenocarcinoma moderately differentiated. After this diagnosis cephalic pancreaticoduodenectomy was performed.
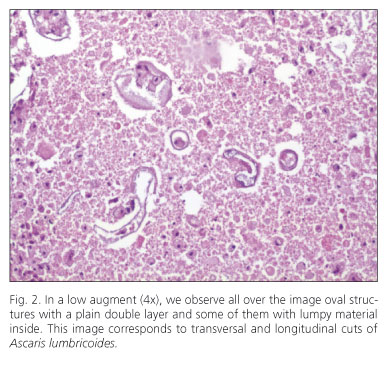
Postoperative evolution was good with a pancreatic leak solved with medical measures. Further anatomical pathology analysis demonstrated pancreatic ascariasis with fibrocaseous nodules and abscess affecting cephalic pancreas and transverse mesocolon (Fig. 2). There were no tumor cells founded in the surgical specimen. The patient was treated with albendazole 400 mg.
Discussion
Ascariasis is frequent helminthic infection which is suffered by a quarter of the human population. Its condition is endemic in developing countries, Asia and Latin America. In developed countries it is unusual (1). The biliopancreatic affection is unlikely, being in our environment extremely rare, but it can be responsible for potentially serious complications (2).
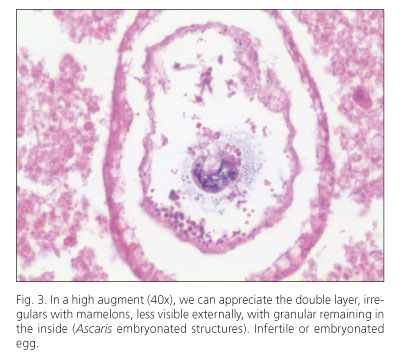
Their eggs (Fig. 3) are swallowed, the larvae emerge, they invade intestinal mucosa and get through the portal and systemic circulation to lungs where they maturate and move to pharynx getting the digestive tract again. They colonize the small intestine and they remain causing no symptoms in most of cases (1,2).
Inbetween abdominal manifestations we focus on biliopancreatic sphere. Toxins excreted by the nematodes (neurotoxins, anafilotoxins, hemolysins,...) produce a spam at Oddi's sphincter (3), and plus detritus from the intestinal tract, bile and pancreas canalicules may get occluded and infect organic fluids (2). The most common form is the biliary colic. Less frequent but more transcendental are other conditions such as acute cholecystic, cholangitis, liver abscess, obstructive jaundice, choledocolithiasis and acute and chronic pancreatitis (4,5).
The elective method of diagnosis is microscopic identification of the eggs in the feces, the fresh exam is able to detect moderate to high infections. The US may be diagnostic in case worms are directly seen.
The treatment for biliary ascariasis is bases in digestive repose, analgesia, extended spectrum antibiotherapy (if there is intra-abdominal infection) and to eradicate the worms using albendazole, pyrantel pamoate, mebendazole or levamisole (1). The extraction of worms using ERCP is a valid option in bile and pancreas obstructions (6).
Although it is exceptional in our environment, Ascaris lumbricoides should be part of differential diagnosis of cephalic pancreas inflammatory tumors.
References
1. Khuroo MS. Ascariasis. Gastroenterol Clin North Am 1996;25:553-77. [ Links ]
2. Khuroo MS, Zargar SA, Mahajan R. Hepatobiliary and pancreatic ascariasis in India. Lancet. 1990;335(8704):1503-6 [ Links ]
3. Alam S, Mustafa G, Rahman S, Kabir SA, Rashid HO, Khan M. Comparative study on presentation of biliary ascariasis with dead and living worms. Saudi J Gastroenterol 2010;16:203-6. [ Links ]
4. Tarafder MR, Carabin H, Joseph L, Balolong E Jr, Olveda R, McGarvey ST. Estimating the sensitivity and specificity of Kato-Katz stool examination technique for detection of hookworms, Ascaris lumbricoides and Trichuris trichiura infections in humans in the absence of a 'gold standard'. Int J Parasitol 2010;40(4):399-404. [ Links ]
5. Ochoa B. Surgical complications of ascariasis. World J Surg 1991;15:222-7. [ Links ]
6. Mangiavillano B, Carrara S, Petrone MC, Arcidiacono PG, Testoni PA. Ascaris lumbricoides-induced acute pancreatitis: diagnosis during EUS for a suspected small pancreatic tumor. JO. 2009;10(5):570-2. [ Links ]











 text in
text in