My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 n.11 Madrid Nov. 2011
https://dx.doi.org/10.4321/S1130-01082011001100014
LETTERS TO THE EDITOR
Endoscopic ultrasound guided fistulization between left intrahepatic duct and jejunum in a patient with Roux-en-Y anastomosis and jaundice
Fistulización entre la vía biliar intrahepática izquierda y el yeyuno guiada por ultrasonografía endoscópica en paciente ictérico con anastomosis en Y- Roux
Key words: Endoscopic retrograde cholangiopancreatography. Endosonography. Obstructive jaundice. Biliary fistula.
Palabras clave: Colangiopacreatografía retrógrada endoscópica. Ecoendoscopia. Ictericia obstructiva. Fístula biliar.
Dear Editor,
Endoscopic retrograde cholangio-pancreatography (ERCP) is considered the elective procedure for biliary decompression in jaundiced patients (1). In the last decade a new endoscopic salvage procedure has been described which allows biliary and pancreatic transmural access guided by endoscopic ultrasound (EUS) in patients in whom ERCP is not feasible (2,3). Hereafter we will refer to this technique as endosonography-guided cholangio-pancreatography (ESCP). Data of ESCP with a transjejunal approach are scarce (4-6). We present a case of a jaundiced patient successfully treated by means of transjejunal ESCP.
Case report
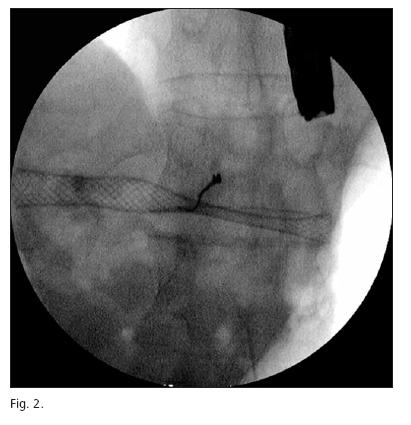
A 76 year old female diagnosed 9 months before of gastric adenocarcinoma surgically treated with total gastrectomy and Roux- en-Y reconstruction, was admitted because of weight loss and jaundice related to a lymphatic recurrence of gastric adenocarcinoma. ERCP was not attempted due to anatomic changes after surgery. ESCP drainage was planned after an informed consent process, by an experienced endoscopist (ELAA). The left intrahepatic duct (LIHD) was identified using a linear echoendoscope (Pentax, FG32-UA, USA). The tip end of device was positioned around 5 cm distally to the esophagus-jejunoanastomosis. The LIHD was punctured with a 19 gauge FNA needle (EUSN-19-T, Cook Endoscopy, Winston- Salem, NC, USA). Iodine contrast was injected under fluoroscopy to demonstrate biliary opacification. A 0.035-inch guidewire was introduced through the EUS needle and advanced in an antegrade fashion under fluoroscopy. The needle was withdrawn, a wire-guided needle knife (Boston Scientific Corp, Watertown, USA) was inserted and used to perform a micro-incision and dilation of the jejunal fistula. A 6 cm long and 1 cm caliber partially covered self-expandable metallic stent (Wallstent, Boston Scientific Corp, Watertown, USA) was passed over the guide through the LIHD fistula without any other dilatation procedure (Fig. 1). There were no complications related to the procedure and the hepaticojejunostomy was also clinically effective in relieving jaundice. The patient was followed until death which occurred 137 days after ESCP.
Discussion
Many descriptive series of ESCP have been published in the last decade with a clinical success rate (considered as jaundice resolution) of 75-100% of patients, but with a high morbidity rate of 10-36%, although death has been rarely described and not related to the procedure itself (6-8). Most of these patients were tackled by means of transgastric or transduodenal drainage, but transjejunal biliary drainage has been also previously described in a total of six patients with Roux-en-Y reconstruction, with good results (4-6).
One of the most critical points of ESCP is dilation of the fistulous tract to enable stent deployment. Different techniques have been used to perform this dilation such as bougie catheters, balloon dilation, cautery with a needle-knife or even Soehendra retriever (7). In this case, we decided to use needle-knife cautery in order to achieve a stable position as soon as possible, avoiding movements of the endoscope related to efforts for mechanical dilation. Although this manoeuvre poses an increased risk for complications, it is recommended by some authors especially when transmural drainage is the endpoint (9). Fortunately, our patient had an uneventful recovery and died without symptoms of biliary obstruction.
Everson L.A. Artifon2, Juan J. Vila2, Dayse Aparicio2, and José L.B. Paione1
1GI Unit of Endoscopy. Ana Costa Hospital. Santos, Brazil.
2Unit of Endoscopy. Complejo Hospitalario de Navarra. Pamplona, Spain
References
1. ASGE Guideline: the role of ERCP in diseases of biliary tract and the pancreas. Gastrointest Endosc 2005;62:1-8. [ Links ]
2. Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy 2001;33:898-900. [ Links ]
3. Pérez-Miranda M, Serna C, Diez-Redondo P, Vila JJ. Concept and techniques of endosonography-guided cholangiopancreatography (ESCP) as a salvage drainage procedure for obstructed biliary and pancreatic ducts. World J Gastrointest Endosc 2010;2(6):212-22. [ Links ]
4. Will U, Thieme A, Fueldner F, et al. Treatment of biliary obstruction in selected patients by endoscopic ultrasonography (EUS)-guided transluminal biliary drainage. Endoscopy 2007;39:292-5. [ Links ]
5. Püspök A, Lomoschitz F, Dejaco C, et al. Endoscopic ultrasound guided therapy of benign and malignant biliary obstruction: a case series. Am J Gastroenterol 2005;100:1743-7. [ Links ]
6. Burmester E, Niehaus J, Leineweber T, Huettereroth T. EUS-cholangio-drainage of the bile duct: report of 4 cases. Gastrointest Endosc 2003; 57:246-51. [ Links ]
7. Vila JJ, Goñi S, Arrazubi V, Bolado F, Ostiz M, Javier Jiménez F. Endoscopic ultrasonography-guided transgastric biliary drainage aided by Soehendra stent retriever. Am J Gastroenterol 2010;105:959-60. [ Links ]
8. Artifon EL, Chaves DM, Ishioka S, et al. Echoguided hepatico-gastrostomy: a case report. Clinics 2007;62:799-802. [ Links ]
9. Yamao K. EUS-guided choledochoduodenostomy. Gastrointest Endosc 2009;69(Supl. 2):S194-S199. [ Links ]











 text in
text in