Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.12 Madrid dic. 2011
https://dx.doi.org/10.4321/S1130-01082011001200013
LETTERS TO THE EDITOR
Liver abscess mimicking colon cancer
Absceso hepático simulando una neoplasia colónica
Key words: Colonic mass. Fever. Subhepatic abscess.
Palabras clave: Neoplasia colónica. Fiebre. Absceso subhepático.
Dear Editor,
Liver abscesses are infrequent and cause 0.013 to 0.02% of admissions (1). These abscesses are located more frequently at right lobe of the liver. The major risk factor is the biliary tract disease such as stones and malignant obstruction (40-60%). The diabetes and liver transplantation are other risk factors (2).
Case Report
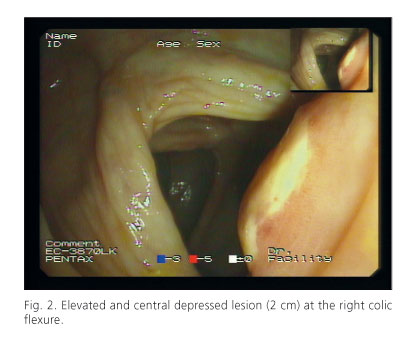
We report the case of a 78 years-old man who was admitted with complains of fever, right lumbar pain and weigh loss of 2 kg the last three months. His past medical history included hypertension, hyperuricemia, kidney stones, and a cholecystectomy because of cholecystitis four months earlier. An abdominal ultrasound scan before the admission showed a splenomegaly (15 cm) and bilateral kidney cysts, the liver, pancreas and bile ducts were normal. Laboratory tests showed the following: elevated erythrocyte sedimentation rate, 86 mm/h, elevated C-reactive protein, 69.9 mg/L, elevated fibrinogen, 731 mg/dL and hemoglobin 11 g/dL. These laboratory findings and the persistent fever prompted hospital admission. On abdominal CT showed hypertrophy of left and caudate hepatic lobes suggestive of chronic hepatitis, a subhepatic abscess of 1 cm and a wall thickening of antrum, pylorus, duodenum and right colic flexure with regional lymph nodes (the biggest 1,7 cm) (Fig. 1). Therefore colonoscopy was performed showing a 2 cm, elevated and central depressed lesion at the hepatic flexure (Fig. 2). The pathologic evaluation showed necrosis and colonic mucosa without cancer. He continued with fever, elevated acute phase reactants and anemia. An ultrasound-guided drainage of subhepatic abscess was performed with a pig-tail catheter of 8,5 Fr and 40 ml of purulent fluid were evacuated, keeping the catheter in site after the procedure. Culture of the fluid grew Citrobacter freundii, Streptococcus viridians and Bacteroides spp. sensible to imipenem that was introduced. Five days after abscess drainage, a colonoscopy was again performed because the biopsy specimen was negative for malignancy. In the same location, the right colic angle, it showed a 1 cm flat lesion (Fig. 3). Another biopsy sample was obtained again, with no neoplastic tissue observed. A follow up abdominal ultrasound did not show any subhepatic abscess and so, the catheter was retired.
Discussion
Our patient had a subhepatic abscess (Fig. 1) secondary to laparoscopic cholecystectomy involving the right colic flexure (Fig. 2), the endoscopic lesion disappeared after the abscess drainage (Fig. 3). It was necessary a second drainage for recurrent abscess and 40 ml were evacuated again. A third colonoscopy was performed and there was not any lesion at the hepatic flexure.
At first, the endoscopic images suggested a colon cancer. There are a few cases reported of colon cancer and the development of a secondary liver abscess, but the location used to be in the rectum or sigmoid colon in 62,5%, the right colic flexure is a rare location. Endoscopic examination is important to establish a correct diagnosis and exclude malignancies (1). In the present case the biopsy specimens were negative for twice.
The ingestion of foreign body can produce a gastrointestinal tear (less than 1%) and the most commonly affected areas are the duodenum, the ileocecal and rectosigmoidal regions. Fish bones are the most common foreign bodies, but this patient has not previous history of this ingestion. Usually, the abscess formation secondary to a foreign body involves the left lobe (3).
There are other conditions that can develop a hepatic abscess such as laparoscopic cholecystectomy (LC) secondary to spill of bile fluid or gallstones to peritoneal cavity due to an accidental gallbladder perforation during the laparoscopy. In this case, the gallstones were observed neither in CT nor abdominal ultrasound. 0.1-2.9% of LC are complicated with intraabdominal abscesses, of which the most frequent location is subhepatic (31.1%). In 90.5% requires surgical treatment (4), but in this case this was not required, although a second drainage was performed. High mortality rates have been described when a second therapeutic procedure is necessary (> 40%) (5). Surgery should be suggested when the response to a medical treatment and drainage is poor.
This case shows a misleading endoscopic suspicion of a colon cancer. Therefore, it is essential to make an accurate differential diagnosis because in some cases this abscess could be secondary to malignant colonic disease.
Cristina Jimeno-Ayllón, Raquel Martínez-Fernández, Lorena Serrano-Sánchez,
Carmen Julia Gómez-Ruiz, Julia Morillas-Ariño, José Ignacio Pérez-García,
Jesús García-Cano-Lizcano and Ángel Pérez-Sola
Division of Digestive Diseases. Unit of Endoscopy.
Hospital General Virgen de la Luz. Cuenca, Spain
References
1. Hiraoka A, Yamashita Y, Uesugi K, Koizumi Y, Yamamoto Y, Doi H, et al. Three cases of liver abscesses complicated with colon cancer without liver metastasis: importance of screening for digestive disease. Int Med 2007;46(24):2013-7. [ Links ]
2. Kaplan, GG, Gregson DB, Laupland KB. Population-based study of the epidemiology of and the risk factors for pyogenic liver abscess. Clin Gastroenterol Hepatol 2004;2(11):1032-8. [ Links ]
3. Santos SA, Alberto S, Cruz E, Pires E, Figueira T, Coimbra E, et al. Hepatic abscess induced by foreign body: Case report and literature review. World J Gastroenterol 2007;13(9):1466-70. [ Links ]
4. Castellón Pavón CJ, Fernández Bermejo M, Morales Artero M, del Amo Olea E. Subhepatic abscess as a late complication of missed intraperitoneal gallstone after laparoscopic cholecystectomy. Gastroenterol Hepatol 2004;27(10):568-72. [ Links ]
5. Chen SC, Huang CC, Tsai SJ, Yen CH, Lin DB, Wang PH, et al. Severity of disease as main predictor for mortality in patients with pyogenic liver abscess. Am Journal Surg 2009;20(10):1-9. [ Links ]











 texto en
texto en