My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 n.3 Madrid Mar. 2012
https://dx.doi.org/10.4321/S1130-01082012000300003
Transit of radiopaque particles through the gastrointestinal tract: comparison between type 2 diabetes patients and healthy individuals
Tránsito de partículas radiopacas a través del tracto gastrointestinal: comparación entre pacientes con diabetes tipo 2 y los individuos sanos
João Xavier Jorge1, Hugo C. Matos2, Joaquim P. Machado2 and Carlos C. Almeida1
1Faculty of Medicine. University of Coimbra. Portugal.
2Service of Radiology. Hospital Center of Coimbra. Portugal
ABSTRACT
Background/aims: some studies have reported controversial results when comparing the gastrointestinal transit between diabetic and healthy individuals. Therefore, we compared the gastrointestinal transit of radiopaque particles between diabetic and non-diabetic healthy individuals.
Methods: abdominal radiographies were performed for 45 type 2 diabetes mellitus patients and 35 healthy individuals (gender and age similar for both groups) at 24 and 72 h after they ingested radiopaque particles. The mean number of particles in the colon was compared for both groups. The data were expressed as mean and standard deviation values.
Results: at 24 h, the total number of particles in the colon did not differ significantly for the diabetic and non-diabetic individuals. At 72 hours, the distribution in the diabetic and non-diabetic individuals was as follows: right colon, 0.44 ± 0.88 and 0.26 ± 0.7, respectively (p = 0.8); left colon, 2.6 ± 4.2 and 0.49 ± 1.3 (p < 0.003); and rectosigmoid colon, 2.65 ± 3.8 and 0.80 ± 1.5 (p < 0.005). The mean number of radiopaque particles in the entire colon was 5.7 ± 7.1 and 1.5 ± 2.7 for diabetic and non-diabetic individuals, respectively (p < 0.001).
Conclusions: the number of radiopaque particles in the colon did not significantly differ for the diabetic and non-diabetic individuals at 24 h after ingestion but was significantly greater in diabetic individuals at 72 h after ingestion. At 72 h, the mean number of radiopaque particles in the left and rectosigmoid colon were significantly higher in the diabetics than in the non-diabetic individuals.
Key words: Transit of radiopaque particles. Diabetes mellitus.
Introduction
Gastrointestinal alterations seem to be common in patients with type 2 diabetes mellitus (DM) (1-3), although studies contradicting these observations also exist (4). Some studies have shown that gastrointestinal transit is altered in diabetic patients (5). Several studies have been performed to study the transit of particles through the small intestine and particularly through the colon; however, results of these studies are controversial (6,7). Several studies have shown that the time taken for orocecal and colorectal transit is longer for diabetic patients than for non-diabetic (ND) individuals (7-9). However, some other studies did not show any significant difference between diabetic and healthy individuals with respect to gastrointestinal transit (10,11). Currently, radiopaque markers are used for studying gastrointestinal transit (6,9,12,13); these markers allow the characterization of the transit time through each part of the gastrointestinal tract by using different methods and formulas and help determine the total transit time (14). This is the standard method, based on which the accuracy of other new methods is evaluated (15-19). Some authors believe that calculating gastrointestinal transit time by using different methods and formulas may produce different outcomes (14). Similarly, the physical characteristics of radiopaque particles can also influence the final results (20).
We hypothesized that diabetic patients have altered gastrointestinal transit and that these alterations may be responsible for the fact that they have a higher frequency of constipation than healthy individuals do (21,22). We aimed to compare the number of radiopaque particles that were retained in the colon of diabetic individuals and healthy controls, at 24 and 72 h after these particles were ingested.
Material and methods
Forty-five patients with DM were randomly selected. They were regularly observed in the Hospital and the Ethical Commission allowed this investigation. The participation was voluntary and all the individuals accepted to be part of this study on basis of an informed consent. Of these 45 patients, 18 were women and 27 were men. The patients' ages ranged between 38 and 69 years (mean age, 58.21 ± 7.7 years). We also selected another 35 ND healthy individuals (15 women and 20 men), who served as the control group. Their ages varied between 41 and 77 years (mean age, 56.8 ± 12.3 years); (p not significant). Thus, the study population comprised 2 groups: the DM and ND groups. Patients were included if they were: a) not undergoing any therapy that affected the gastrointestinal transit; b) had not undergone any surgery involving the gastrointestinal tract; c) did not have any neurological or mental perturbations; and d) if they (the female subjects) were not pregnant at the time of the study. The individuals included in the ND group showed no signs of diabetic autonomic neuropathy determined using the coefficients of variation of R-R intervals on the electrocardiograms (CV RR). The DM patients were undergoing therapy involving oral anti-diabetic medications, insulin, or both. During the study, the DM patients were allowed to continue their medications; all the subjects maintained their normal lifestyle during the study.
Each individual was asked to swallow 25 radiopaque particles at 1 time, in the morning. The particles were approximately 3 mm long with a maximum diameter of 2 mm.
Abdominal radiographs were obtained at 2 time points, i.e., at 24 and 72 h after ingesting radiopaque particles, for both groups.
Regarding the fact that different formulas for calculating gastrointestinal transit time may produce different outcomes and that all of them are based in the number of radiopaque particles in the gastrointestinal tract, in this study we just compared the total number of radiopaque particles in each segments and in the total colon, at 24 and at 72 h after ingesting radiopaque particles.
Three medical doctors (1 gastroenterologist and 2 radiologists) analyzed the number of radiopaque particles present in the colon by using radiographs obtained at each time point. The data were analyzed using the Student t test of SPSS17 and are presented as mean and standard deviation (± SD), with the minimum significance of p < 0.05.
Results
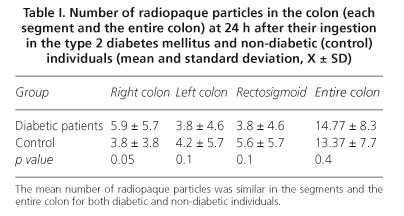
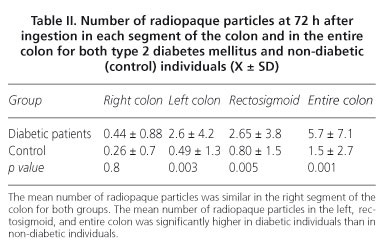
At 24 h the mean number of radiopaque particles in the colon of DM patients was 14.77 ± 8.3, whereas that in the colon of ND individuals was 13.37 ± 7.7; this difference was not statistically significant (p = 0.4). At 24 h, the distribution of radiopaque particles in the 3 segments of the colon -the right colon (RC), left colon (LC), and rectosigmoid (RS) colon- was similar for both DM and ND individuals. The mean number of radiopaque particles in the RC of DM and ND individuals was 5.9 ± 5.7 and 3.8 ± 3.8, respectively (p = 0.05); in the LC, 5.4 ± 4.2 and 4.3 ± 4.5, respectively (p = 0.1); and in the RS colon, 3.8 ± 4.6 and 5.6 ± 5.7, respectively (p = 0.1). These data are presented in table I. The distribution of radiopaque particles at 72 hours greatly differed between the DM and ND individuals (Table II). At 72 h, the distribution of radiopaque particles in the RC was similar for both groups (DM vs. ND), 0.44 ± 0.88 vs. 0.26 ± 0.7 (p = 0.8); however, the number of particles in the LC was significantly higher (p < 0.003) for the DM patients (2.6 ± 4.2) than for the ND individuals (0.49 ± 1.3). Similar results were obtained while comparing the 2 groups with respect to the distribution of radiopaque particles in the RS colon (2.65 ± 3.8 and 0.80 ± 1.5 for the DM and ND individuals, respectively; p < 0.005). The mean number of the radiopaque particles in the entire colon at 72 h was 5.7 ± 7.1 and 1.5 ± 2.7 (p < 0.001) for the DM and ND individuals, respectively.
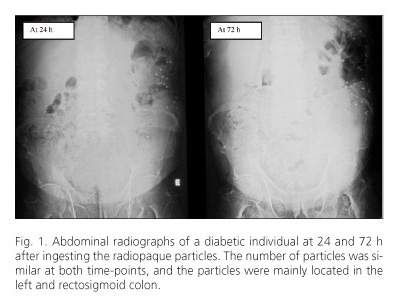
Two radiographs of a DM patient that were obtained at 24 and 72 h after ingesting the particles are shown in figure 1, along with the distribution of the radiopaque particles. The figure shows that the number of radiopaque particles was similar at 24 and 72 h after ingestion. Moreover, at 72 h, most of the radiopaque particles were located in the LC and RS colon.
Discussion
Our results showed that the mean number of radiopaque particles in the colon, at 24 h after ingestion was statistically similar for the 2 groups. This may be because of the similar orocecal transit of these particles through the gastrointestinal tract for these 2 groups. Many studies have shown that orocecal transit is not altered in diabetic patients without neuropathy (11,23).
At 72 h after ingestion, the DM patients showed a significantly higher mean number of radiopaque particles in the colon than the ND individuals. Similar results were reported by Iida (6) who observed that the transit of radiopaque particles through the colon was slower in diabetic patients but there were no significant differences in the upper gastrointestinal transit. In particular, he also observed that the differences were not significant in the right segments of the colon. This observation was similar to that made by Kawagishi (24) who observed that the transit time was similar in the proximal segments of the colon. In fact, our results indicate that at 72 h, the difference in the number of radiopaque particles was not significant for the DM and ND groups in the case of the RC but was extremely significant in the case of the LC and RS. Ours results contradict those mentioned in the registry established by Ron (10). In his study on diabetic and ND individuals, Ron did not find a significant difference in the transit of radiopaque particles, although the diabetic patients had a slightly longer transit time than the ND individuals did.
We used a small radiopaque marker (length, 3/2 mm), which according to W. Guilford (25), has a transit similar to those of food when it passes through the gastrointestinal tract, and is retained in the stomach for a shorter time during gastric emptying.
DM patients had a slower colonic transit, particularly through the SR colon and LC, than the ND healthy individuals did. This slower transit time explains the high frequency of constipation in diabetic individuals, which is clinically relevant because it influences their quality of health. On a similar sense, the high frequency of constipation among diabetics augments the amount of drugs taken by these patients, raising the monetary value of their treatment.
In conclusion were found that at 24 h after ingestion, there were no significant differences in the number of radiopaque particles in the colon of DM and ND healthy individuals. At 72 h after ingestion, the mean number of radiopaque particles in the colon was significantly higher in DM patients than in ND healthy controls. At 72 h after ingestion, the differences in the number of radiopaque particles in the LC and RS colon were significantly higher in DM patients than in ND individuals.
Conclusions
- At 24 h after ingestion, the mean number of radiopaque particles in the colon was similar for the type 2 DM and ND (control) individuals. This may indicate that the orocecal transit was probably similar for both groups.
- In general, the transit of particles through the colon in the ND individuals was faster than that in the DM individuals; this difference was highly significant.
- The transit of radiopaque particles through the RC was similar for type 2 DM patients and ND individuals.
- At 72 h after ingestion, type 2 DM patients showed a slower transit of radiopaque particles through the LC and SR colon than the ND individuals did.
Acknowledgments
We would like to thank the patient and volunteer groups that participated in our study. We would also like thank Dr. Cristina Martins, Department of Mathematics, Coimbra University and Dr. Bárbara Oliveiros, the Institute of Biostatistics, Faculty of Medicine, Coimbra University for their contribution in the statistical analysis of the results.
Dr. João X. Jorge and Dr. Cláudia I.C. Borges were supported by Enterprises Sonangol.
References
1. Chandrasekharan B, Anitha M, Blatt R, Shahnavaz N, Kooby D, Staley C, et al. Colonic motor dysfunction in human diabetes is associated with enteric neuronal loss and increased oxidative stress. Neurogastroenterol Motil 2011;23:131-8. [ Links ]
2. Frøkjær JB, Egsgaard LL, Graversen C, Søfteland E, Dimcevski G, Blauenfeldt RA, et al. Gastrointestinal symptoms in type-1 diabetes: Is it all about brain plasticity? Eur J Pain 2011;15:249-57. [ Links ]
3. Kim JH, Park HS, Ko SY, Hong SN, Sung IK, Shim CS, et al. Diabetic factors associated with gastrointestinal symptoms in patients with type 2 diabetes. World J Gastroenterol 2010;16:1782-7. [ Links ]
4. Lodefalk M, Aman J. Gastrointestinal symptoms in adolescents with type 1 diabetes. Pediatr Diabetes 2010;11:265-70. [ Links ]
5. Yamamoto T, Watabe K, Nakahara M, Ogiyama H, Kiyohara T, Tsutsui S, et al. Disturbed gastrointestinal motility and decreased interstitial cells of Cajal in diabetic db/db mice. J Gastroenterol Hepatol 2008;23:660-7. [ Links ]
6. Iida M, Ikeda M, Kishimoto M, Tsujino T, Kaneto H, Matsuhisa M, et al. Evaluation of gut motility in type II diabetes by the radiopaque marker method. J Gastroenterol Hepatol 2000;15:381-5. [ Links ]
7. Jung HK, Kim DY, Moon IH, Hong YS. Colonic transit time in diabetic patients-comparison with healthy subjects and the effect of autonomic neuropathy. Yonsei Med J 2003;44:265-72. [ Links ]
8. Sarno S, Erasmas LP, Haslbeck M, Hölzl R. Orocaecal transit, bacterial overgrowth and hydrogen production in diabetes mellitus. Ital J Gastroenterol 1993;25:490-6. [ Links ]
9. Triantafyllou K, Kalantzis C, Papadopoulos AA, Apostolopoulos P, Rokkas T, Kalantzis N, et al. Video-capsule endoscopy gastric and small bowel transit time and completeness of the examination in patients with diabetes mellitus. Dig Liver Dis 2007;39:575-80. [ Links ]
10. Ron Y, Leibovitz A, Monastirski N, Habot B, Segal R. Colonic transit time in diabetic and nondiabetic long-term care patients. Gerontology 2002;48:250-3. [ Links ]
11. Wegener M, Börsch G, Schaffstein J, Luerweg C, Leverkus F. Gastrointestinal transit disorders in patients with insulin-treated diabetes mellitus. Dig Dis 1990;8:23-36. [ Links ]
12. Feldman M, Smith HJ, Simon TR. Gastric emptying of solid radiopaque markers: studies in healthy subjects and diabetic patients. Gastroenterology 1984;87:895-902. [ Links ]
13. Wu MJ, Chang CS, Cheng CH, Chen CH, Lee WC, Hsu YH, et al. Colonic transit time in long-term dialysis patients. Am J Kidney Dis 2004;44:322-7. [ Links ]
14. Bouchoucha M, Prado J, Chtourou L, Devroede G, Atanassiu C, Benamouzig R. Non-compliance does not impair qualitative evaluation of colonic transit time. Neurogastroenterol Motil 2011;23:103-8. [ Links ]
15. Camilleri M, Thorne NK, Ringel Y, Hasler WL, Kuo B, Esfandyari T, et al. Wireless pH-motility capsule for colonic transit: prospective comparison withradiopaque markers in chronic constipation. Neurogastroenterol Motil 2010;22:874-82. [ Links ]
16. Abrahamsson H, Antov S. Accuracy in assessment of colonic transit time with particles: how many markers should be used? Neurogastroenterol Motil 2010;22:1164-9. [ Links ]
17. Xu HM, Han JG, Na Y, Zhao B, Ma HC, Wang ZJ. Colonic transit time in patient with slow-transit constipation: Comparison of radio paque markers and barium suspension method. Eur J Radiol 2011;79:211-3. [ Links ]
18. Rao SS, Kuo B, McCallum RW, Chey WD, DiBaise JK, Hasler WL, et al. Investigation of colonic and whole-gut transit with wireless motility capsule and radiopaque markers in constipation. Clin Gastroenterol Hepatol 2009;7:537-44. [ Links ]
19. Zhang WQ, Yan GZ, Ye DD, Chen CW. Simultaneous assessment of the intraluminal pressure and transit time of the colon using a telemetry technique. Physiol Meas 2007;28:141-8. [ Links ]
20. Olmos J, Soifer L, De Paula JA, San Román J, Varela E, Bustos Fernández L, et al. Do the physical characteristics of radiopaque markers modify the results of the measurement of colonic transit time? Acta Gastroenterol Latinoam 1994;25(5):287-90. [ Links ]
21. Ron Y, Wainstein J, Leibovitz A, Monastirsky N, Habot B, Avni Y, et al. The effect of acarbose on the colonic transit time of elderly long-term care patients with type 2 diabetes mellitus. J Gerontol A Biol Sci Med Sci 2002;57:M111-4. [ Links ]
22. Rossol S. Constipation in patients with diabetes mellitus. MMW Fortschr Med 2007;149:39-42. [ Links ]
23. Kawagishi T, Nishizawa Y, Okuno Y, Sekiya K, Morii H. Segmental gut transit in diabetes mellitus: effect of cisapride. Diabetes Res Clin Pract 1992;17:137-44. [ Links ]
24. Keshavarzian A, Iber FL. Intestinal transit in insulin-requiring diabetics. Am J Gastroenterol 1986;81:257-60. [ Links ]
25. Guilford WG, Lawoko CR, Allan FJ. Accuracy of localizing radiopaque markers by abdominal radiography and correlation between their gastric emptying rate and that of a canned food in dogs. Am J Vet Res 1997;58:1359-63. [ Links ]
![]() Correspondence:
Correspondence:
João Xavier Jorge.
e-mail: cambombo@hotmail.com
Received: 04-08-11.
Aceppted: 21-10-11.