Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 no.3 Madrid mar. 2012
https://dx.doi.org/10.4321/S1130-01082012000300007
PICTURES IN DIGESTIVE PATHOLOGY
Mantle cell lymphoma with intestinal involvement
Linfoma de células del manto con afectación intestinal
Paola Quintas-Lorenzo, Inés Castro-Novo, Andrés Dacal-Rivas, María Francisco-González, Joaquín Cubiella-Fernández and Javier Fernández-Seara
Department of Digestive Diseases. Complexo Hospitalario Universitario de Ourense. Spain
Case report
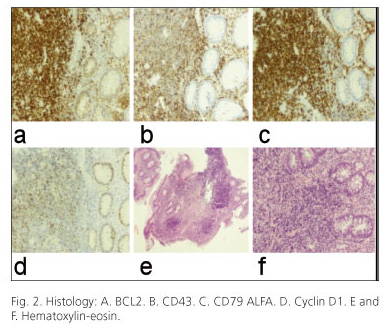
A 53-year-old male was referred to our unit due to tenesmus, rectal bleeding and altered bowel habit. On rectal examination a hard mass was palpable. A colonoscopy was performed where multiple polyps, most of them larger than 10 mm (Fig. 1), and a protruded neoplastic lesion in rectum were found. The histology (Fig. 2) showed infiltration by B cell lymphoma (BCL), suggestive of mantle cell lymphoma (MCL). In computed tomography (CT) multiple thoracic-abdominal-pelvic adenopathies, some of them forming a conglomerate (Fig. 3), were observed. The patient was referred to the haematology department with the diagnosis of BCL for further study and treatment.
The study was completed with a bone marrow aspirate that suggested infiltration by BCL. He was initially treated with R-CHOP chemotherapy plus G-CSF. After a partial response, he was switched to a second line with R-MINE/ESHAP and autologous peripheral blood precursors to full recovery of blood count parameters.
Discussion
The BCL is a subtype of NHL B phenotype that accounts for 2.5 to 10% of all lymphomas (1). Although the most common gastrointestinal location is multiple lymphomatous polyposis, this endoscopic diagnosis remains very rare. It is characterized by the presence of multiple tumour-like polyps (2). Its natural history is very aggressive, with a median survival of 3 to 5 years. The mean onset age is around 60 years and predominantly in males (3-5).
It often occurs in a disseminated form and with frequent extranodal involvement. It usually affects the colon and rectum in 90%, but it can also affect small intestine (69%), stomach (57%) and duodenum (52%). An immunophenotypic study is essential to characterize the lymphoma: CD20, CD5 and cyclin D1 antigens and the presence of translocation t (11;14). Clinical factors associated with poor prognosis are advanced age, poor general condition, advanced stage, splenomegaly, elevated LDH, low serum albumin, tumour disease and anaemia. Chemotherapy is the treatment of choice, including regimens with CHOP, cyclophosphamide, vincristine and prednisone (COP) and doxorubicin, teniposide, cyclophosphamide and prednisolone (AvmCP).
References recommended
1. Romaguera J, Hagemeister FB. Lymphoma of the colon. Current Opin Gatroenterol 2005;21(1):80-4. [ Links ]
2. Lavergne A, Brouland JP, Launay E, Nemeth J, Ruskone-Fourmestraux A, Galian A. Multiple lymphomatous polyposis of the gastrointestinal tract. Cancer 1994;74(11):3042-50. [ Links ]
3. Remes-Troche JM. A rare case of multiple lymphomatous poliposis. Arch Patol Lab Med 2003;127:1028-30. [ Links ]
4. Hokama A, Tomoyose T, Yamamoto Y, Watanabe T, Hirata T, Kinjo F, et al. Adult T-cell leukemia/lymphoma presenting multiple lymphomatous polyposis. World J Gastroenterol 2008;14(42):6584-8. [ Links ]
5. Vignote ML, Chicano M, Rodríguez FJ, Acosta A, Gómez F, Poyato A, et al. Multiple lymphomatous polyposis of the GI tract: report of a case and review. Gastrointest Endosc 2002;56(4):579-82. [ Links ]











 texto en
texto en