My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 n.8 Madrid Aug. 2012
https://dx.doi.org/10.4321/S1130-01082012000800009
Giant duodenal ulcer perforation: a case of innovative repair with an antrum gastric patch
Perforación de ulcus gigante duodenal: reparación innovadora mediante una plastia del antro gástrico
Javier A.-Cienfuegos, Fernando Rotellar, Víctor Valentí, Jorge Arredondo, Jorge Baixauli, Nicolás Pedano, Manuel Bellver and José Luis Hernández-Lizoain
Department of General and Digestive Surgery. Clínica Universidad de Navarra. Pamplona, Navarra. Spain
ABSTRACT
Backgrounds: the treatment of a perforated giant duodenal ulcer (GUDs) represents a formidable surgical challenge regarding the duodenal wall defect repair in severe peritonitis setting. A high incidence of dehiscence and hospital mortality (15-40%- has been reported with the majority of the techniques).
We report a case of GUDs perforation successfully treated with a subtotal gastrectomy and a gastric patch with the remnant antrum, for repairing the duodenal defect.
Case report: a 63-years-old man with antecedents of peptic ulcer disease presents a large duodenal ulcer perforation with 48 hrs delay and associated with severe peritonitis and a retroperitoneal collection. A subtotal gastrectomy with Billroth II reconstruction and reconstruction of the duodenal defect with a patch of the remnant antrum was carried out. The patient was discharged at 17th postoperative day with good tolerance.
Discussion: the duodenal defect repair with a patch of the remant antrum, represents a valid alternative in similar circumstances. To our knowledge, it appears to be the first clinical description of this technique.
Key words: Giant ulcer. Perforation. Gastric patch. Duodenal repair.
RESUMEN
Antecedentes: el tratamiento de un ulcus duodenal gigante (UDG; > 2 cm) perforado entraña una gran dificultad técnica, por la reparación del gran defecto duodenal; y por la peritonitis sobreañadida. Todas las técnicas descritas se asocian con un índice elevado de dehiscencias y una mortalidad del 15-40%. Describimos por primera vez el caso de un UDG perforado, tratado mediante una gastrectomía subtotal y con una plastia del antro gástrico remanente.
Caso clínico: varón de 63 años que se interviene de un UDG perforado en la 2a porción duodenal asociado con peritonitis severa y disección de la gotiera parieto-cólica derecha retroperitoneo. Se realiza gastrectomía tipo Bilroth II y reparación del defecto duodenal mediante una plastia con la pared del antro gástrico remanente. El paciente fue dado de alta a los 17 días.
Discusión: la reparación del defecto duodenal con una plastia del antro gástrico, puede ser una opción muy valiosa en situaciones similares a la descrita. En nuestro conocimiento, se trata de la primera descripción clínica de esta técnica.
Palabras clave: Ulcus gigante. Perforación. Plastia gástrica. Reparación duodenal.
Introduction
Despite the efficacy of medical treatment of peptic ulcer disease (PU), an already increase incidence of severe PU complications -bleeding, perforation- have been reported, attributed to the indiscriminate use of non-steroidal anti-inflammatory and low-dose aspirin (1-3).
These complications usually occur in patients suffering of concurrent medical illness and are associated with an increased operative mortality (15-40%). Patient age older than 70 years, a delay in the surgical treatment, preoperative shock (Blood pressure < 100 mmHg), hypoalbuminemia, metabolic acidosis and renal dysfunction have identified as poor prognostic factors (2-4).
The giant duodenal ulcer (GUDs) perforation (a full-thickness peptic ulcer 2 cm or larger in diameter and usually involving a large portion of the duodenum) is a rare entity that represents a formidable surgical challenge regarding the duodenal defect repair specially when is associated with life-threatening peritonitis.
We describe the case of perforated GDUs, associated with systemic inflammatory response, successfully treated with a partial gastrectomy and a patch with the remnant antrum for closing the large duodenal defect. To our knowledge, it represents the first clinical report with this technique.
Case report
A 63-years-old man was referred from a local hospital because persisting abdominal pain, with nausea, vomiting and weakness. Five days earlier, the patient consulted in the referring hospital because of sudden abdominal epigastric pain irradiated to right hypocondrium, associated with nausea and vomiting undigested food particles. An upper endoscopy revealed a double pylorus sign, with one of the lumen occluded. The exploration was interrupted because acute bleeding. On the following day, a conventional barium meal study showed a gastric outlet obstruction.
In his recent medical history, the patient had been operated 12 months before of a duodenal ulcer perforation. A Graham patch (omental patch) with primary closure of the ulcer was performed. There was no relation with Helicobacter pylori and afterwards the patient was treated with proton-pump inhibitors (PPI), 20 mg daily.
In his past medical history, the patient had been diagnosed at the age of 23 years with duodenal peptic ulcer. He currently smokes 20 cigarettes daily and consumes 80-100 mg of alcohol daily.
On examination, the patient appeared ill and complaining of abdominal pain. Pulse, 140 beats per minute; blood pressure, 103/72 mmHg. Oxygen saturation 96% while he was breathing ambient air. There was epigastric tenderness and throughout right hypocondrium guarding. Laboratory testing showed leukocytosis of 11.8 x 103µL neutrophils, 67.1%; monocytes 23.6%; platelets 255 x 103 per mm3, fibrinogen, 877 mg/dL. Rest of laboratory tests were normal. During his admission, the temperature rouse to 38.5 oC, persisted the leukocytosis and C reactive protein (CRP), 29 mg/dL (normal value, 0.8 mg/dl).
A plain radiography and an ultrasonography revealed a large retroperitoneal collection (> 10 cm diameter) with presence of gas bubbles, free air and barium contrast agent extravasation into the Morrison's pouch and right paracolic gutter.
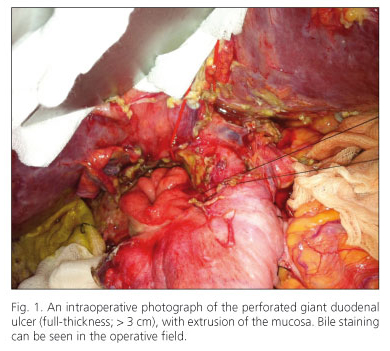
An urgent laparotomy was carried out, disclosing a large purulent collection, which occupied the entire right paracolic space and Morrison's pouch. A wide Kocher maneuver and mobilization of the duodenum revealed a perforated GUD with mucosal extrusion in the posterior wall of the second part of the duodenum (Fig. 1).
A subtotal gastrectomy combined with truncal vagectomy and Billroth II reconstruction was carried out. A gastric patch with the remnant antrum was used to cover the duodenal defect, shaping as "notched lapel" with interrupted 3/0 silk seromuscular sutures (Figs. 2 and 3). The retroperitoneal space was covered with a large vascularized segment of the greater omentum. After copious washing of the abdominal cavity a closed drain (Jakson-Pratt®) was placed on the right parietocolic space.
In the 6th postoperative day, an intraabdominal collection was drained under ultrasonography control, yielding polymicrobial flora. The patient developed an uneventful postoperative course being discharged at 16th postoperative day with a regular diet. The pathology report was negative for Helicobacter pylori.
Discussion
Despite the efficacy of the medical treatment of peptic ulcer disease, in the last decades a steady increase in the PU complications has been reported regarding with NSAIDs consumption (1-4).
The PU perforation still represents 10-20% of the surgical complications, having recently raised the attention of several authors (2,3). In a prospective study of 113 consecutive cases: age older than 70 years, the presence of shock at the time of admission, a delay beyond 24 h in the diagnosis and concurrent medical illness, were related with hospital mortality (4). Besides these risk factors, ASA physical status (American Society of Anesthesiologists), hypoalbuminemia, increased serum creatinine, and metabolic acidosis have been confirmed as well (2-5).
The perforated giant ulcers comprise about 1-2% of the perforated duodenal ulcers, and are associated with a high morbidity (20-70%) and mortality (15-40%). Perforation of GDUs is particularly hazardous and represent a surgical challenge regarding the closure of the severe duodenal wall defect and surrounding inflammation (6-9).
Though the majority of PU perforations (0-2 cm wide) are successfully treated with one-layer closure plus a greater omentum patch (Graham technique); perforations of GDUs demand more complex procedures as subtotal gastrectomy associated with jejunal serosal patch, pedicle graft of jejunum or pyloric exclusion. Nevertheless each of these procedures have shown a high incidence of duodenal dehiscence (> 10%) and a high mortality (10-65%) (3,4,7-10).
In our case a partial gastrectomy with Billroth II reconstruction, a gastric patch with the antrum remnant for covering the duodenal defect was carried out, as consequence of the peritoneal contamination and the patient's previous history of PU disease.
The repair of severe duodenal wall defects have been an issue of several experimental and clinical studies, under the circumstances of oncologic procedures, blunt abdominal trauma as well as GDUs or diverticulum perforation (6,9,11-14). In 1978, Papachristou and Fortner described in dogs the "island" gastric patch with the greater curvature of the stomach meanwhile keeping intact its gastric wall vasculature, for closing duodenal defects, although has not been described in humans (15).
The use of an isolated jejunal loop as serosal patch is the preferred technique, concurrently others have adduced duodenal diversion claiming the technical complexity in the severe peritonitis scenario as well (7,8,10).
A high incidence of dehiscence (> 10-50%) and gastric outlet obstruction has been reported in most of the papers. The shown technique could be very useful in the hazardous setting of large GUDs perforation associated with peritoneal contamination.
Acknowlegments
The authors thank Íñigo Chalezquez for the art-work and Beatriz Urbelz for the technical assistance.
References
1. Thorsen K, Glomsaker TB, Von Meer A, Soreide K, Soreide JA. Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg 2011;15:1329-35. [ Links ]
2. Moller MH, Shah K, Bendix J, Jensen A G, Zimmermann-Nielsen E, Adamsen S, et al. Risk factors in patients surgically treated for peptic ulcer perforation. Scand J Gastroenterol 2009;44:145-52. [ Links ]
3. Gupta S, Kaushi KR, Sharma R, Attri A. The management of large perforations of duodenal ulcers. BMC Surgery 2005;5:1-5. [ Links ]
4. Boey J, Wong J. Perforated duodenal ulcers. World J Surg 1987;11: 319-24. [ Links ]
5. Fombellida D, Gil Romea I, Moreno Mirallas MJ, Urieta Carpi A. Factores de riesgo en el tratamiento quirúrgico de la úlcera piloroduodenal perforada. Rev Esp Enferm Dig 1988;90:503-8. [ Links ]
6. Castellano G, Galvao O, Vargas J, Canga F, Moreno D, Sánchez T, et al. The diagnosis of peptic ulcer penetration into the liver by endoscopy biopsy. A report of 2 cases and review of the literature. Rev Esp Enferm Dig 1992;82:235-8. [ Links ]
7. Nussbaum MS, Schusterman MA. Management of giant duodenal ulcer. Am J Surg 1985;149:367-1. [ Links ]
8. Lal P, Vindal A, Hadke NS. Controlled tube duodenostomy in the management of giant duodenal ulcer perforation -a new technique for a surgically challenging condition. Am J Surg 2009;198:319-23. [ Links ]
9. Walley BD, Goco I. Duodenal patch grafting. Am J Surg 1980;140: 706-7. [ Links ]
10. Jani K, Saxena AK, Vaghasia R. Omental plugging for large-sized duodenal peptic perforations: A prospective randomized study of 100 patients. South Med J 2006;99:467-71. [ Links ]
11. Degiannis E, Boffard K. Duodenal injuries. Br J Surg 2000;87:1473-9. [ Links ]
12. Bhattachacharjee HK, Misra MC, Kumar S, Bansal VK. Duodenal perforation following blunt abdominal trauma. J Emerg Trauma Shock 2011;4:514-7. [ Links ]
13. Ishiguro S, Moriura S, Kobayashi I, Tabata T, Yoshioka Y, Matsumoto T. Pedicled ileal flap to repair large duodenal defect after rigth hemicolectomy for right colon cancer invading the duodenum. Surg Todat 2004;34:386-8. [ Links ]
14. Hosseini SV., Abbasi HR, Rezvani H, Vasei M, Ashraf MJ. Comparison between gallbladder serosal and mucosal patch in duodenal injuries repair in dogs. J Invest Surg 2009;22:148-53. [ Links ]
15. Papachristou DN, Fortner JG. Reconstruction of duodenal wall defects with the use of a gastric "island" flap. Arch Surg 1977;112:199-200. [ Links ]
![]() Correspondence:
Correspondence:
Javier A.-Cienfuegos.
Department of General and Digestive Surgery.
Clínica Universidad de Navarra.
Avda. Pío XII, 36.
31008 Pamplona, Navarra. Spain
email: fjacien@unav.es
Received: 10-02-2012
Accepted: 02-03-2012











 text in
text in