My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 n.9 Madrid Sep. 2012
https://dx.doi.org/10.4321/S1130-01082012000900002
Ionizing radiation in patients with Crohn's disease. Estimation and associated factors
Radiación ionizante en pacientes con enfermedad de Crohn. Estimación y factores asociados
Ana Ciáurriz-Munuce1, María Fraile-González1, Helena León-Brito1, Miren Vicuña-Arregui1, Santiago Miquélez2, Juan Úriz-Otano1 and Carlos Jiménez-López1
1Department of Gastroenterology. Complejo Hospitalario de Navarra B. Pamplona, Navarra. Spain
2Department of Radio-Physics. Complejo Hospitalario de Navarra. Pamplona, Navarra. Spain
ABSTRACT
Introduction: exposure to ionizing radiation is associated with an increased risk of developing tumors. Patients with Crohn's disease (CD) usually require multiple imaging tests using this type of radiation.
Objectives: the objectives of this study were to estimate the total dose of ionizing radiation received by patients with Crohn's disease during their course and to identify the factors associated with higher radiation doses.
Methods: two hundred thirty-five CD patients diagnosed between 1972 and 2010 were included. The effective dose (ED) received by each patient was calculated retrospectively based on the number of gastrointestinal transit studies and computed tomography scans performed. Considering recent epidemiological studies, an ED greater than or equal to 50 mSv was used as the cut-off point for increased risk of developing cancer.
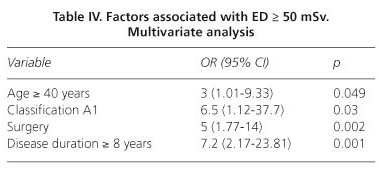
Results: the mean ED received per patient was 33.4 mSv (95% CI 29.3-37.5). A total of 49 (20.8%) patients received an ED ≥ 50 mSv. The following factors were identified as independent predictors associated with an ED ≥ 50 mSv: Age older than 40 years, need for surgery, age under 16 years at diagnosis and disease duration over 8 years.
Conclusions: a substantial proportion of patients with Crohn's disease receive high doses of potentially carcinogenic ionizing radiation. Identification of the most susceptible patients to receive high doses of radiation, monitoring of effective doses received and the use of imaging techniques that do not require ionizing radiation (MR enterography, abdominal ultrasound) could contribute in reducing patients' exposure to potentially carcinogenic ionizing radiation.
Key words: Crohn's disease. Radiation. Gastrointestinal transit. Computed tomography.
RESUMEN
Introducción: la exposición a radiación ionizante se asocia a un mayor riesgo de desarrollar tumores. Los pacientes con enfermedad de Crohn requieren habitualmente múltiples pruebas de imagen que utilizan este tipo de radiación.
Objetivos: los objetivos de este estudio son estimar la dosis total de radiación ionizante recibida por pacientes con enfermedad de Crohn a lo largo de su evolución e identificar los factores asociados a dosis de radiación más altas.
Métodos: se incluyeron 235 pacientes con enfermedad de Crohn diagnosticados entre 1972 y 2010. Se calculó retrospectivamente la dosis efectiva (DE) recibida por cada paciente, teniendo en cuenta los tránsitos gastrointestinales y las tomografías computarizadas que se habían realizado. Basados en estudios epidemiológicos previos, se consideró un valor umbral de DE ≥ 50 mSv de mayor riesgo de desarrollar cáncer.
Resultados: la media de DE recibida por paciente fue 33,4 mSv (IC 95% 29,3-37,5). Un total de 49 (20,8%) pacientes recibió una DE ≥ 50 mSv. Se identificaron como factores predictivos independientes asociados a una DE ≥ 50 mSv: edad mayor de 40 años, necesidad de cirugía, edad al diagnóstico menor 16 años y tiempo de evolución mayor de 8 años.
Conclusiones: un porcentaje considerable de pacientes con enfermedad de Crohn recibe dosis elevadas de radiación ionizante potencialmente carcinogénicas. La identificación de los pacientes mas susceptibles a recibir dosis altas de radiación, la monitorización de la dosis efectiva recibida y la utilización de pruebas de imagen que no utilizan radiación ionizante (enterorresonancia, ecografía abdominal), podrían contribuir a reducir la exposición a la radiaciones ionizantes potencialmente carcinogénicas.
Palabras clave: Enfermedad de Crohn. Radiación. Tránsito gastrointestinal. Tomografía computarizada.
Abbreviations
CD: Crohn's disease.
GIT: gastrointestinal transit.
CT: computed tomography.
ED: effective dose.
mSv: miliSievert.
Introduction
Crohn's disease (CD) is a condition characterized by inflammation and ulceration of the gastrointestinal tract and may be accompanied by multiple extraintestinal manifestations. It has a chronic course with alternation of symptomatic periods and clinical remission. It is usually diagnosed in the second or third decade of life but in 20% of patients it is identified in childhood (1).
For initial diagnosis, assessment of disease extent and activity, assessment of treatment response and follow-up, as well as for endoscopic procedures, CD patients undergo repeated imaging tests, some of which use ionizing radiation -gastrointestinal transit (GIT) and computed tomography (CT)-. Exposure to ionizing radiation, even at diagnostic levels, is associated with an increased incidence of cancer (2).
The aim of our study was to estimate the total dose of ionizing radiation received by patients with Crohn's disease followed in a tertiary hospital and to identify the factors associated with the exposure to higher radiation doses.
Materials and methods
Study design and patients
A retrospective study involving patients followed up in our department, diagnosed with CD between 1972 and 2010. Exclusion criteria included patients with a doubtful diagnosis of CD, mainly indeterminate colitis, and patients with CD diagnosed at another site (incomplete medical history).
Data were obtained from the clinical records of each patient. Different demographic and clinical variables were collected: sex, age, Montreal classification, history of major surgery as a consequence of CD, disease duration in years and number of GIT studies and CT scans performed in each patient since (their disease) diagnosis (studies performed for reasons unrelated to control of CD were excluded ) (Table I).
Calculation of radiation doses
The effective dose (ED) of radiation was calculated retrospectively for each patient. CT scans were performed in a SIEMENS SOMATON EMOTION single slice scanner until the year 2008 and a SIEMENS SENSATION 64 multislice scanner from 2008 onwards. GIT examinations were performed on a remote-controlled GENERAL ELECTRICAL MPS-64 table.
Considering the characteristics of the radiographic studies and equipment used in our center, an ED mean value of 10 mSv was calculated for each GIT, and 9 mSv for each CT. These doses were calculated assuming a voltage of 80 kV, an imaging time of 180 s, a current of 5 mA and 3 shots per examination for GITs, and a voltage of 130 kV and a dose-length product of 600 mGy*cm for CT scans.
Considering recent epidemiological studies (2-4), an ED greater than or equal to 50 mSv was used as the cut-off point for increased risk of developing cancer.
Data analysis
Student's t, Chi-square and Fisher's exact tests were used for the comparison of quantitative and categorical variables. For the identification of predictive factors associated with high radiation doses, a univariate analysis was performed and a multivariate analysis with the binary logistic regression test was also carried out. In the multivariate analysis, only variables with predictive value identified in the previous univariate analysis were included. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 17.0.
Results
Out of the 248 patients initially evaluated, 13 (5.2%) were excluded due to prior diagnosis of indeterminate colitis or incomplete medical history (6 and 7 patients, respectively).
Two hundred thirty five patients diagnosed with CD between 1972 and 2010 were included, of which 123 (52.3%) were male, with a median age of 39 (16-82) years and with a median disease duration of 8 (0-38) years.
Forty percent of the patients required major surgery in the course of their disease, which was more common in patients with a stricturing or penetrating pattern than in patients with an inflammatory pattern (93%, 57% vs. 11%, respectively, p < 0.001).
Four (2%) patients developed a total of 5 tumors throughout the follow-up period: breast cancer and vulvar cancer 20 and 24 years after CD diagnosis (1 patient, ED: 20 mSv), breast cancer 14 years after CD diagnosis (ED: 87 mSv), testicular seminoma 9 years from diagnosis (ED: 0 mSv) and cutaneous lymphoma 29 years from CD diagnosis (ED: 129 mSv).
Effective dose received
A total of 817 radiographic studies (493 GITs and 324 CTs) were performed in 207 (88%) patients. GITs were done in 182 patients (77.4%) (median: 2, range: 1-15) and CTs were performed in 139 patients (59.1%) (median: 2, range: 1-10). Both tests were done in 114 (48.5%) patients.
The mean ED received per patient was 33.4 mSv (95% CI 29.3-37.5). Patients over 40 years of age, with disease duration of longer than 8 years, diagnosis of CD at age under 16 years, stricturing or penetrating pattern, ileal and ileocolic location, involvement of the upper gastrointestinal tract, and patients who had been submitted to surgical treatment received a higher dose of radiation (p < 0.05) (Table II).
Effective dose ≥ 50 mSv
Forty nine (20.8%) patients received an ED ≥ 50 mSv. The factors associated with an ED ≥ 50 mSv were disease duration greater than or equal to 8 years, diagnosis of CD at age younger than 16 years, a stricturing or penetrating pattern, ileocecal or ileocolic location, involvement of the upper gastrointestinal tract, and history of major surgery due to CD (Table III). However, in the multivariate analysis, the variables identified as independent predictive factors related to a greater potential risk for tumor development (ED ≥ 50 mSv) were patient's age over 40 years, the need for surgery, diagnosis age under 16 years and disease duration over 8 years (Table IV).
Discussion
Standard management of patients with Crohn's disease includes performing repeated imaging tests such as gastrointestinal transit (GIT) and computed tomography (CT) that may use ionizing radiation which has a cumulative effect in the patient. Any dose of ionizing radiation is able to induce malignancy in the long term. Studies which investigate the association between cancer risk and ionizing radiation have been conducted on two large cohorts (atomic bomb survivors and nuclear industry workers). These publications demonstrate that there is statistically significant increase in the risk of tumour development with an ED exposure above 35-40 mSv (2-4). Furthermore, recently published epidemiological studies suggest that this risk increases progressively with an ED from 50 mSv onwards (5,6). For this reason, an ED greater than or equal to 50 mSv was used as the cut-off point for increased risk of developing cancer. It is estimated that up to 1 in 10 patients with inflammatory bowel disease is exposed to potentially harmful radiation doses (7,8).
In our study, one out of every 5 patients with CD was exposed to doses of ionizing radiation which are considered to be potentially carcinogenic (ED ≥ 50 mSv). The effective radiation dose was calculated taking in account only GIT studies and abdominal CT scans indicated for this condition, without considering other sources of ionizing radiation such as plain X-rays of the abdomen or additional tests requested for other conditions. Thus, it is likely that the actual total doses received per patient were underestimated.
A GIT study is a radiological test used for the assessment of the small bowel, which has progressively fallen into disuse since the mid 1980s, and has been replaced by CT (9). Because our sample included patients diagnosed from 1972 onwards, we found many studies of this type in it. The ED from a GIT study depends on the number of images taken and on the time needed for the imaging. The common method for calculating ED is to consult standardized tables. For a more precise estimate of the radiation dose received, radio-physics specialists of our center have estimated the ED attributed to each GIT study by using mean values. For CTs, universally accepted DLP (dose-length product) to effective dose conversion factors are employed. To calculate the DLP, the mean values obtained in a sample of patients undergoing abdominal CT within the annual program of patients' dose estimation have been taken.
Children, women, and subjects under 40 years of age are more radiosensitive (2,8). In our sample, the ED received was similar in both sexes. Elderly patients (≥ 40 years) received higher doses of radiation, which is probably related to a longer time since disease onset (Table II). Our patients diagnosed with CD at an age under 16 years, possibly due to the chronic course and more aggressive nature of the disease, were exposed to higher doses of radiation than patients diagnosed later on in life (Table II).
The multivariate analysis shows that the need for surgery is one of the independent predictive factors related to more carcinogenic EDs (ED ≥ 50 mSv). This finding is probably influenced by the fact that many of these patients have had a more aggressive disease course, and therefore a greater need for radiological examinations for complication diagnosis and monitoring. In our series, 93% of patients with a penetrating pattern and 51% with a stricturing pattern were operated on in contrast to 11% of patients with an inflammatory pattern (p < 0.001).
Disease duration is one of the most important factors associated with higher doses of radiation (10). In our study, patients aged 40 years or older, with an early diagnosis of the disease (before 16 years), and with a disease duration over 8 years received potentially harmful radiation doses (ED ≥ 50 mSv) (p < 0.05).
Involvement of the upper gastrointestinal tract could be another feature related to high EDs (11). These patients require a greater number of imaging tests for the evaluation of gastrointestinal tract portions which are poorly accessible by endoscopy. Additionally, surgical procedures are more frequently performed on them. In our case, the limited number of patients included in our sample meeting these characteristics may have underestimated the true effect that the involvement of the upper gastrointestinal tract has on the dose of radiation received (p > 0.05).
Chronic inflammation of the gastrointestinal tract in patients with CD entails a greater risk of developing colorectal cancer, small bowel cancer and lymphoma (11). In addition, the use of immunosuppressive drugs such as azathioprine and mercaptopurine, and monoclonal antibodies such as infliximab, could increase the risk of malignancy (8,11,12). On the other hand, thiopurines cause an increase in this risk by enhancing radiosensitivity (13). Thus, patients with a more severe disease which received higher doses of radiation (10,11) and required a more frequent use of immunosuppressive and/or biological drugs, would have an increased risk for tumor development (8).
In our study, four patients developed some type of cancer, and there was one patient with two tumors. Two subjects were exposed to potentially carcinogenic radiation doses (87 mSv and 129 mSv respectively). The patient with the highest ED (129 mSv) developed a cutaneous lymphoma. These results should be interpreted with caution because this is a descriptive study. Furthermore, the main aim of our paper is to estimate the total dose of ionizing radiation received by patients with Crohn's disease, and to identify the factors associated with an exposure to higher radiation doses. We do not to intend to assess patients' cancer risk based on the radiation doses received.
In the recent decades, technological advances have made CT a commonly used procedure in CD patients due to its wide availability, high resolution, and promptness and convenience for the patient (2,9). It also permits the assessment of associated extraluminal disease. All these factors have contributed to an extended use of CT as part of the routine clinical practice in patients with CD, resulting in a greater exposure to ionizing radiation and possibly an increased risk of developing tumors (2,7). Therefore, ionizing radiation should be a factor to be taken into account so as to limit the use of CT in patients with CD, particularly in those groups with the greatest radiosensitivity (infants, women) or higher requirements of imaging tests (14).
The implementation of a record of the cumulative dose of radiation in the medical history of patients with CD would be convenient. The use of alternative imaging tests that do not require ionizing radiation (MR enterography, abdominal ultrasound), should also be considered so that the harmful effect of radiation in these patients is reduced.
MR enterography is a valid alternative with a comparable diagnostic accuracy to CT (15,16), as it is able to identify intestinal inflammatory activity and even differentiate it from fibrosis. It also assesses the degree of extraintestinal involvement, with an even higher resolution than CT for the study of fistulas and perianal disease (17,18). MR enterography indications include the diagnosis and assessment of CD extent, planning of medical-surgical treatments and the detection of complications (18). However, the availability of this technique is lower and its cost is greater (19).
Abdominal ultrasound is a dynamic and low-cost imaging procedure with a good diagnostic performance in the evaluation of the small bowel in CD. In spite of the operator dependence it entails, its sensitivity and specificity have improved due to the development of new techniques such as ultrasound using oral contrast and echo-Doppler. Therefore, it might be a very useful technique for the diagnosis and monitoring of patients with CD, as well as for cases in which surgery is proposed (15,17,20).
In conclusion, in our study, a significant number of CD patients receive high doses of ionizing radiation, which is potentially associated with an increased risk of tumor development. In these patients, it would be advisable to monitor the effective dose of radiation, to limit the use of examinations which require ionizing radiation, and to evaluate the use of alternative imaging tests with a high diagnostic accuracy such as ultrasonography and MR enterography, particularly in those subjects which may be more predisposed to receive higher doses of radiation.
References
1. Loftus EV Jr. Clinical Epidemiology of Inflammatory Bowel Disease: incidence, prevalence, and environmental influences. Gastroenterology 2004;126:1504-17. [ Links ]
2. Brenner DJ, Hall EJ. Computed tomography -An increasing source of radiation exposure. N Engl J Med 2007;357:2277-84. [ Links ]
3. Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. BRJ 2008;81:362-78. [ Links ]
4. Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res 2000;154:178-86. [ Links ]
5. Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci 2003;100:13761-6. [ Links ]
6. Pauwels EK, Bourguignon M. Cancer induction caused by radiation due to computed tomography: a critical note. Acta Radiol 2011;52:767-73. [ Links ]
7. Newnham E, Hawkes E, Surender A, James SL, Gearry R, Gibson PR. Quantifying exposure to diagnostic medical radiation in patients with inflammatory bowel disease: are we contributing to malignancy? Aliment Pharmacol Ther 2007;26:1019-24. [ Links ]
8. Kroeker KI, Lam S, Birchall I, Fedorak RN. Patients with ibd are exposed to high levels of ionizing radiation through CT scan diagnostic imaging: a five-year study. J Clin Gastroenterol 2011;45(1):34-9. [ Links ]
9. Jaffe TA, Gaca AM, Delaney S, Yoshizumi TT, Toncheva G, Nguyen G, et al. Radiation doses from small-bowel follow-through and abdominopelvic MDCT in Crohn's disease. Am J Roentgenol 2007; 189:1015-22. [ Links ]
10. Levi Z, Fraser A, Krongrad R, Hazazi R, Benjaminov O, Meyerovitcha J, et al. Factors associated with radiation exposure in patients with inflammatory bowel disease. Aliment Pharmacol Ther 2009;30:1128-36. [ Links ]
11. Desmond AN, O'regan K, Curran C, McWilliams S, Fitzgerald T, Maher MM, et al. Crohn's disease: factors associated with exposure to high levels of diagnostic radiation. Gut 2008;57:1524-9. [ Links ]
12. Aithal GP, Mansfield JC. Review article: the risk of lymphoma associated with inflammatory bowel disease and inmunosuppressive treatment. Aliment Pharmacol Ther 2001;15:1101-8. [ Links ]
13. Smith MA, Irving PM, Marinaki AM, Sanderson JD. Review article: malignancy on thiopurine treatment with special reference to inflammatory bowel disease. Aliment Pharmacol Ther 2010;32:119-30. [ Links ]
14. Peloquin JM, Pardi DS, Sandborn WJ, Fletcher JG, McCollough CH, Schueler BA. Diagnostic ionizing radiation exposure in a population-based cohort of patients with inflammatory bowel disease. Am J Gastroenterol 2008;103:2015-22. [ Links ]
15. Mackalski BA, Bernstein CN. New diagnostic imaging tools for inflammatory bowel disease. Gut 2006;55:733-41. [ Links ]
16. Ripollés T, Martínez MJ. Técnicas seccionales de imagen en la enfermedad de Crohn: ecografía, tomografía computarizada y resonancia magnética. Radiología 2007;49:97-108. [ Links ]
17. Bruining DH, Loftus EV Jr. Technology insight: new techniques for imaging the gut in patients with IBD. Nat Clin Pract Gastroenterol Hepatol 2008;5(3):154-61. [ Links ]
18. Tolan DJM, Greenhalgh R, Zealley IA, Halligan S, Taylor SA. MR Enterographic manifestations of small bowel Crohn Disease. Radiographics 2010;30:367-84. [ Links ]
19. Lee SS, Kim AY, Yang SK, Chung JW, Kim SY, Park SH. Crohn disease of the small bowel: comparison of ct enterography, mr enterography and small-bowel follow through as diagnostic techniques. Radiology 2009;251:751-61. [ Links ]
20. Pallota N, Tomei E, Viscido A, Calabrese E, Marcheggiano A, Caprilli R, et al. Small intestine contrast ultrasonography: an alternative to radiology in the assessment of small bowel disease. Inflamm Bowel Dis 2005;11:146-53. [ Links ]
![]() Correspondence:
Correspondence:
Ana Ciáurriz Munuce
Department of Gastroenterology
Complejo Hospitalario de Navarra B
C/ Irunlarrea, 3
31008 Pamplona, Navarra. Spain
e-mail: anaciaurriz@hotmail.com
Received: 16-05-2012
Accepted: 07-08-2012











 text in
text in