Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 no.11 Madrid dic. 2012
https://dx.doi.org/10.4321/S1130-01082012001100009
PICTURES IN DIGESTIVE PATHOLOGY
Successful endoscopic mesh removal after laparoscopic Nissen fundoplication
Retirada endoscópica de malla migrada tras funduplicatura laparoscópica tipo Nissen
Iago Rodríguez-Lago1, Miguel Muñoz-Navas1, Juan Carrascosa1, Maite Betés1, Víctor Valentí2 and Fernando Rotellar2
Departments of 1 Gastroenterology and 2 General and Digestive Surgery. Clínica Universidad de Navarra. Pamplona. Navarra, Spain
Case report
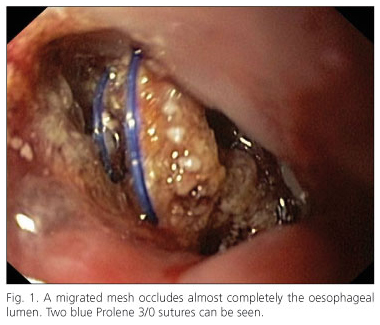
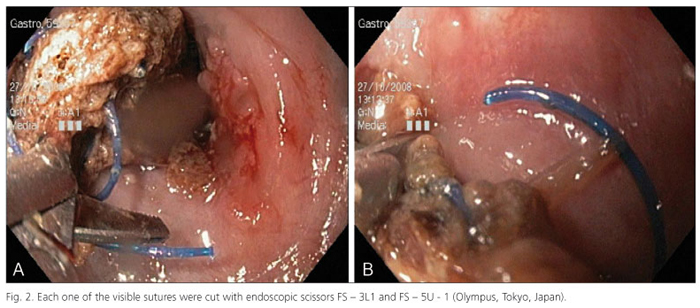
A 72-year-old male was admitted because of dysphagia for solids and liquids. He had undergone a laparoscopic Nissen fundoplication due to erosive esophagitis and hiatal hernia. Three years later, due to symptomatic recurrence of the hernia, surgery with placement of a polypropylene mesh was indicated. After four years he developed epigastric pain and dysphagia for liquids. Gastroduodenoscopy showed a polypropylene mesh occluding almost all the esophageal lumen (Fig. 1). The symptoms worsened, with dysphagia for solids and liquids, with weight loss. First of all, we decided to remove the mesh endoscopically. A first attempt was done by exerting strong traction on the mesh with biopsy forceps without any result. At this point we looked for each one of the blue Prolene 3/0 (Fig. 2A) sutures and cut them with endoscopic scissors FS-3L1 and FS-5U-1 (Fig. 2B) (Olympus, Tokyo, Japan). The mesh was extracted successfully in two fragments (Fig. 3). There were no complications related to the procedure.
Discussion
Laparoscopic Nissen fundoplication is the most common surgical procedure performed for gastroesophageal reflux disease treatment. It has a high rate of success, but failure of the fundoplication is a major problem. Rupture and recurrence with simple suture is a possible complication, so mesh reinforcement has been an option in the last years. The risk of mesh erosion after prosthetic hiatal reinforcement is reported to be up to 2.3 % (1). The most common presenting symptoms are dysphagia, heartburn, chest pain, weight loss, and epigastric pain (2). The median time to onset of symptoms is 23.4 months (2). There are few cases reported of successful endoscopic removal of a migrated mesh. It seems like the best results are obtained by grasping the mesh with a foreign body forceps and cutting all the visible sutures using endoscopic scissors (3,4).
References
1. Targarona EM, Bendahan G, Balague C, Garriga J, Trias M. Mesh in the hiatus: A controversial issue. Arch Surg. 2004;139:1286-96; discussion 1296. [ Links ]
2. Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG, et al. Mesh complications after prosthetic reinforcement of hiatal closure: A 28-case series. Surg Endosc. 2009;23:1219-26. [ Links ]
3. Kattih M, Brady PG, Mamel JJ. Suture-induced dysphagia: The role of endoscopy in diagnosis and therapy. Gastrointest Endosc. 2003;58:636-7. [ Links ]
4. Donatelli G, Dallemagne B, Perretta S, Dhumane P, Marescaux J. Fully endoscopic removal of migrated mesh after laparoscopic fundoplication eroded into the gastroesophageal junction: A case report (with video). Gastrointest Endosc. 2012;75:455-7. [ Links ]











 texto en
texto en