Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 no.2 Madrid feb. 2013
https://dx.doi.org/10.4321/S1130-01082013000200003
Primary lymphoma of the colon
Linfoma primario de colon
Marta Pascual1, Blanca Sánchez-González2, Mar García3, Miguel Pera1 and Luis Grande1
1Colorectal Surgery Unit. Department of Surgery. 2Hematology Department. 3Pathology Department. Hospital del Mar. Barcelona, Spain
ABSTRACT
Background: primary colorectal lymphoma is a very rare disease, representing less than 0.5 % of all primary colorectal neoplasms. The gastrointestinal tract is the most frequently involved site of all extranodal lymphomas, the most common type of that is non-Hodgkin's lymphoma. Early diagnosis is often difficult because of unspecific symptoms. Therapeutic approaches have classically included radical resection, chemotherapy and radiotherapy.
Materials and methods: we present our experience in the management of primary colorectal lymphomas over a 17-year period (1994-20011).
Results: in this period 7 cases of primary colorectal lymphoma were diagnosed in our institution. Abdominal pain and change in bowel habit were the most frequent symptoms. Five patients underwent emergency surgery because of bleeding or bowel obstruction. All primary intestinal lymphomas studied were of the B-cell phenotype. Patients were followed up for a median of 59 months (range 1-180). Three of them are alive with no evidence of recurrence.
Conclusion: combination treatment with chemotherapy and surgery can obtain good remission rate. Surgery can resolve complications such bleeding or intestinal perforation that are implicated in lymphoma mortality.
Key words: Lymphoma. Colon. Surgery. Treatment.
RESUMEN
Introducción: el linfoma primario de colon y recto es una patología poco prevalente, representa tan solo el 0,5 % de todas las neoplasias primarias de colon y recto. El tracto gastrointestinal es el lugar donde asientan la gran mayoría de los linfomas extranodales, siendo el más frecuente el tipo linfoma no-Hodking. El diagnóstico precoz es siempre difícil debido a que la sintomatología es muy poco específica. Los algoritmos terapéuticos han incluido clásicamente la resección radical, el tratamiento con quimioterapia y con radioterapia.
Materiales y métodos: presentamos nuestra experiencia en el manejo de los linfomas primarios de colon en un periodo de 17 años (1994-2011).
Resultados: en dicho periodo en nuestro centro fueron diagnosticaron 7 casos de linfoma primario de colon. El dolor abdominal y los cambios en el ritmo deposicional fueron los síntomas más frecuentes. Cinco pacientes requirieron tratamiento quirúrgico urgente debido a hemorragia digestiva u obstrucción intestinal. El estudio anatomopatológico reveló que todos los linfomas tenían el fenotipo de tipo B. Los pacientes tuvieron un seguimiento medio de 59 meses (rango 1-180). Tres de ellos siguen vivos sin evidencia de recidiva.
Conclusión: el tratamiento combinado con quimioterapia y cirugía puede obtener buenos resultados de remisión. La cirugía puede resolver complicaciones como la hemorragia o la perforación intestinal, ambas directamente relacionadas con la mortalidad por linfoma.
Palabras clave: Linfoma. Colon. Cirugía. Tratamiento.
Introduction
Primary lymphoma of the colon and rectum is a rare tumor. It comprises only 0.2-1.2 % of all colonic malignancies (1,2). The gastrointestinal (GI) tract is the most frequently extranodal involved site, accounting for 30-40 % of all cases (1,3). The predominant location of GI lymphomas is the stomach (50-60 %) (4) followed by small bowel (20-30 %), and colon and rectum (10-20 %) (5). To establish the diagnosis it is necessary to have a high index of suspicion because the variability of symptoms.
Treatment often involves a multidisciplinary approach, combining surgery and chemotherapy, with the use of radiotherapy in selected cases. However, there are no randomized trials and treatment decisions are mainly based on expert opinions or consensus.
We present the experience of primary colorectal lymphomas over a 15-year period in a single center.
Patients and methods
We performed a retrospective descriptive study of all consecutive cases of primary colorectal lymphoma diagnosed in our institution from 1994 to 2011. The registry of the Department of Pathology was used for this purpose.
All cases were histologically confirmed. The type of lymphoma was classified according to the WHO classification system (6). Immunohistochemical analysis (IHC) was performed to classify lymphomas as germinal center B-cell (GCB) or non-germinal center B-cell (ABC) subtypes (7). A computed tomography scan (CT) and a bone marrow biopsy was performed to determine what stage of the Ann Arbor Staging System for gastrointestinal lymphoma was used.
The following clinical information was obtained: Age, sex, presentation, site of tumor, operation performed, histology, length of stay, intraoperative complications, adjuvant therapy, treatment response and duration of follow-up.
Results
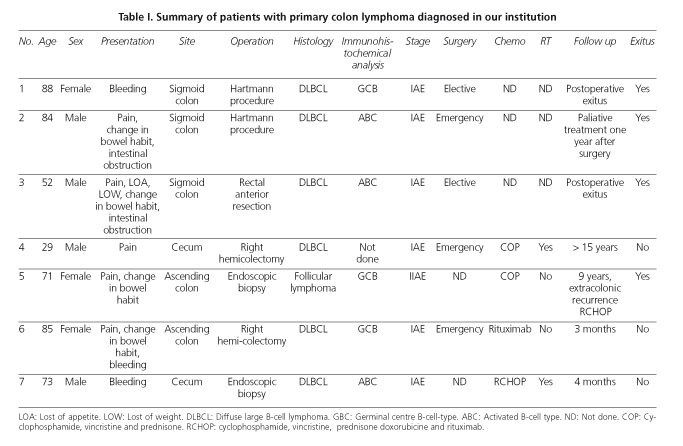
During the 15-year study period, 7 cases of primary colorectal lymphoma were diagnosed. This comprised 0.23 % of all colorectal malignances seen in our department during this period (Table I).
The median age at diagnosis was 67 years (range: 35-87), 4 males. Five patients had good performance status (ECOG/PS 0-1). All of the patients were stage I-II according to Ann Arbor Staging System. The International Prognostic Index (IPI) was low (0-1) in 4 cases. The patients presented with different symptoms, including abdominal pain in 5, change in bowel habit in 4, bleeding in 3, and anorexia or loss of weight in two cases (29 %).
The most common sites of involvement were sigmoid colon in 3, cecum in 2 and ascending colon in 2 other cases. Macroscopically the lesions varied from solitary fungating masses to multiple colonic polyps (Fig. 1). All primary colorectal lymphomas studied were B-cell type (Fig. 2), staining positively for pan B-cell marker CD20. Moreover, 6 out of 7 of the cases corresponded to diffuse large B-cell lymphoma (DLBCL). There was one case of follicular lymphoma. According to immunohistochemical analysis, DLBCL cases could be subclassified as GCB subtype in 2 cases and as ABC subtype in 3. In one case the paraffin block was not available for additional immunohistochemical studies.
The diagnosis of lymphoma was done by surgical resection in 5 patients, and by endoscopic biopsies in 2.
Two patients underwent elective resection and 3 other patients required emergency surgery. Of these, two patients presented with lower gastrointestinal bleeding requiring right hemicolectomy and one patient with intestinal obstruction underwent a Hartmann's procedure. There were two postoperative exitus, a patient with an elective anterior rectal resection who died due to an anastomotic leak and another patient having emergency surgery who died of respiratory and renal failure.
Four patients received chemotherapy or immunotherapy, 2 after surgical excision and 2 after endoscopic diagnosis. The regimens used were cyclophosphamide, vincristine and prednisone (COP), plus doxorubicine (CHOP) or/and rituximab (R). This last is a monoclonal antibody against the protein CD20 that destroys B cells and is part of the so call immunotherapy. This follow-up was performed jointly with the medical oncologists-hematologists. All of them achieved complete remission. The follow-up of the four patients had a median of 52 months (range 1-180). Three patients are alive with no evidence of recurrence and 1 patient died of systemic lymphoma progression. Interestingly, this patient had follicular lymphoma.
Discussion
Primary colorectal lymphoma is a rare disorder comprising 0.1 %-0.5 % of all malignant tumor of the colon and rectum (8,9).
The disease appears later in life, predominantly in the male population (2,10-11). In our study, the mean age was 67 years, which is similar to what was reported in the literature, although we report a case of a 29 years old woman, the youngest patient ever presented in previous series. However, in our study, we have found a similar distribution between males and females.
In our patients, the most common presenting symptom was abdominal pain, according to previous reports (2,5,12,13). Other less common modes of presentation in our series included; change in bowel habit, gastrointestinal bleeding and anorexia or loss of weight, similar to other studies published (5); (1,2,10). Some authors have reported rare cases of emphysematous colitis (14) as the first clinical manifestation, and also masquerading Crohn's disease (15). In conclusion, there are nonspecific symptoms and the diagnosis may be delayed for extended periods.
The most common site for colorectal lymphoma is the cecum, occurring in 57 % of cases, probably because more lymphoid tissue is present in this region. Other sites of the disease are the ascending colon (18 %), the transverse and recto-sigmoid colon (10-20 %) and the descending colon (5 %) (2,12,13,16,17). However, in our study, the most common location for colorectal lymphoma was the sigmoid colon (43 %).
All of our tumours were of B-cell origin, most of them diffuse large B-cell types (85.7 %); this again correlated well with previous reports (2,18). Inflammatory bowel disease (IBD) and immunosuppression have been reported as classical risk factors (19). Even more, human immunodeficiency virus (HIV) positivity has been reported to be associated with a higher incidence of anorectal lymphomas (3). However recent studies (2,5) have not established them as clear risk factors. None of the patients in this series had IBD, HIV or other immune disorders, so we cannot establish a direct causal link.
Treatment of colorectal lymphoma usually involves surgery and chemotherapy. Nowadays, due to the introduction of new active drugs as monoclonal antibodies like rituximab as part of chemotherapy treatment (20), the role of surgery is debatable. Some authors propose that surgery could be beneficial to prevent perforation or bleeding (1) whereas others suggest that early diagnosis and chemotherapy might avoid a surgical procedure. In our opinion, surgery may be beneficial in those patients at risk of complications such as hemorrhage, obstruction and perforation, but it should be associated with postoperative chemotherapy. Moreover, surgery alone with or without radiotherapy must be reserved for selected cases, as localized low-grade lymphomas, because the vast amount of lymphomas, moderate and high-grade B cell lymphoma as DLBCL, almost always extends beyond local fields. In these cases, chemotherapy, with or without surgical excision remains the basis of the treatment.
As known, the CHOP chemotherapeutic regimen (cyclophosphamide, doxorubicine, vincristine and prednisone) remains the first line therapy for primary colorectal lymphomas. Several prospective trials have shown that adding rituximab, monoclonal antibody, to CHOP regimen (RCHOP) resulted in higher response rates and better survival in systemic non-Hodgkin lymphomas but there is few information in primary colorectal lymphoma (21). There are some series that have shown their experience with chemotherapy, many of them before rituximab era, but there results are controversial (22). Of interest, in our study, four patients were treated with chemotherapy or immunotherapy, two of them with previous hemicolectomy and all patients achieved complete response.
Recent advances in gene expression profiling and immunohistochemical analysis (IHC) have led to the identification different subtypes of DLBCL, and confirmed that patients with the ABC disease subtype are less likely to respond well to CHOP-based regimens than those with GCB disease (23). In the future, the identification of these patterns could predict the most effective management strategies for patients. There are no series of patients published with the IHC analysis and survival correlation. In our series, 3 of 6 patients were ABC subtype. We need more patients to analyse the impact of ABC subtype in primary colorectal lymphoma survival.
Survival rate is poor, as we have reported. Unspecific symptoms make this entity difficult to diagnose and, in the majority of cases, the disease is advanced at the time of the first treatment. Histological grade and need of emergency surgery seem to be factors affecting survival (1,24).
Unfortunately, there are no controlled trials providing evidences for the optimal therapeutic approach in patients with primary colorectal lymphoma.
In conclusion, primary lymphoma of the colon and rectum is a rare tumor. Combination of chemotherapy and surgery seems to be the most effective treatment in the majority of patients. Nevertheless, the optimal management of primary lymphoma of the colon and rectum is not established. The new immunochemotherapies may have an impact on primary colorectal lymphoma survival. Moreover, identification of different subtypes of gene expression profiles could lead to improve treatment options.
References
1. Bairey O, Ruchlemer R, Shpilberg O. Non-Hodgkin's lymphomas of the colon. Isr Med Assoc J 2006;8:832-5. [ Links ]
2. Wong MT, Eu KW. Primary colorectal lymphomas. Colorectal Dis 2006;8:586-91. [ Links ]
3. Doolabh N, Anthony T, Simmang C, Bieligk S, Lee E, Huber P, et al. Primary colonic lymphoma. J Surg Oncol 2000;74:257-62. [ Links ]
4. Zinzani PL, Magagnoli M, Pagliani G, Bendandi M, Gherlinzoni F, Merla E, et al. Primary intestinal lymphoma: Clinical and therapeutic features of 32 patients. Haematologica 1997;82:305-8. [ Links ]
5. Gonzalez QH, Heslin MJ, Davila-Cervantes A, Álvarez-Tostado J, de los Monteros AE, Shore G, et al. Primary colonic lymphoma. Am Surg 2008;74:214-6. [ Links ]
6. Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, et al. The World Health Organization classification of hematological malignancies report of the Clinical Advisory Committee Meeting, Airlie House, Virginia, November 1997. Mod Pathol 2000;13:193-207. [ Links ]
7. Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004;103:275-82. [ Links ]
8. Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961;49:80-9. [ Links ]
9. Stanojevic GZ, Nestorovic MD, Brankovic BR, Stojanovic MP, Jovanovic MM, Radojkovic MD. Primary colorectal lymphoma: An overview. World J Gastrointest Oncol 2011;3:14-8. [ Links ]
10. Tauro LF, Furtado HW, Aithala PS, D'Souza CS, George C, Vishnumoorthy SH. Primary lymphoma of the colon. Saudi J Gastroenterol 2009;15:279-82. [ Links ]
11. Musallam KM, Hatoum HA, Barada K, Taher AT, Salem ME, Malek EM, et al. Primary colorectal lymphoma. Med Oncol 2010;27:249-54. [ Links ]
12. Henry CA, Berry RE. Primary lymphoma of the large intestine. Am Surg 1988;54:262-6. [ Links ]
13. Wychulis AR, Beahrs OH, Woolner LB. Malignant lymphoma of the colon. A study of 69 cases. Arch Surg 1966;93:215-25. [ Links ]
14. Chou YH, Hsu HL, Lee JC, Lin BR, Liu KL. Emphysematous colitis of ascending colon with portal venous air caused by diffuse large B-cell lymphoma. J Clin Oncol 2010;28:e496-7. [ Links ]
15. Kashi MR, Belayev L, Parker A. Primary extranodal Hodgkin lymphoma of the colon masquerading as new diagnosis of Crohn's disease. Clin Gastroenterol Hepatol 2010;8:A20. [ Links ]
16. Dionigi G, Annoni M, Rovera F, Boni L, Villa F, Castano P, et al. Primary colorectal lymphomas: Review of the literature. Surg Oncol 2007;16(Supl 1): S169-71. [ Links ]
17. Contreary K, Nance FC, Becker WF. Primary lymphoma of the gastrointestinal tract. Ann Surg 1980;191:593-8. [ Links ]
18. Zighelboim J, Larson MV. Primary colonic lymphoma. Clinical presentation, histopathologic features, and outcome with combination chemotherapy. J Clin Gastroenterol 1994;18:291-7. [ Links ]
19. Azab MB, Henry-Amar M, Rougier P, Bognel C, Theodore C, Carde P, et al. Prognostic factors in primary gastrointestinal non-Hodgkin's lymphoma. A multivariate analysis, report of 106 cases, and review of the literature. Cancer 1989;64:1208-17. [ Links ]
20. Salar A, Domingo-Domenech E, Estany C, Canales MA, Gallardo F, Servitje O, et al. Combination therapy with rituximab and intravenous or oral fludarabine in the first-line, systemic treatment of patients with extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue type. Cancer 2009;115:5210-7. [ Links ]
21. Pfreundschuh M, Trumper L, Osterborg A, Pettengell R, Trneny M, Imrie K, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: A randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol 2006; 7:379-91. [ Links ]
22. Pricolo R, Parziale A, Filosa M, Voltolini F, Zangrandi A. Primary lymphoma of the rectum: a case report and review of the literature. Chir Ital 2002;54:549-54. [ Links ]
23. Wilson WH H-IF, Dunleavy K, Little RF, O'Connor OA. Novel disease targets and management approaches for diffuse large B-cell lymphoma. Leuk Lymphoma 2010;51(Supl. 1):1-10. [ Links ]
24. Fan CW, Changchien CR, Wang JY, Chen JS, Hsu KC, Tang R, et al. Primary colorectal lymphoma. Dis Colon Rectum 2000;43:1277-82. [ Links ]
![]() Correspondence:
Correspondence:
Marta Pascual
Colorrectal Surgery Unit
Department of Surgery
Hospital del Mar
Passeig Marítim, 25-29
08003 Barcelona, Spain
e-mail:
Mpascual@parcsalutmar.cat
Received: 08-02-2012
Accepted: 20-02-2013











 texto en
texto en