Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 no.2 Madrid feb. 2013
https://dx.doi.org/10.4321/S1130-01082013000200016
LETTERS TO THE EDITOR
Severe colitis due to indomethacin suppository
Colitis grave por supositorios de indometacina
Key words: Indomethacin suppository. Nonsteroidal anti-inflammatory drugs. Colitis.
Dear Editor,
Colitis occurs with exposure to various chemicals, including alcohol, radiocontrast agents, glutaraldehyde, formalin, ergotamine, hydrogen peroxide and drugs (1). Frequency of colitis induced by drugs is often under estimated. Antibiotics, 5-fluorouracil (5-FU), hydroxycarbamide, nonsteroidal anti-inflammatory drugs (NSAIDS) and aspirin are usually incriminated (2-4). We report the case of severe diarrhea and hematochezia after self administration of an indomethacin suppository to a young woman.
Case report
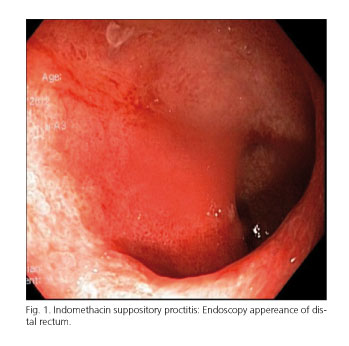
A 30-year-old female presented to the gastroenterology department with rectal pain, diarrhea and rectal bleeding. Her past medical history revealed migraine for 1 year. She had self administered indomethacin suppository 200 mg/day with the hope to improve headache for 3 months. The patient developed severe rectal pain and bloody diarrhea. At admission, physical examination revealed mild abdominal tenderness at lower quadrant and digital rectal examination was painful. Laboratory tests were normal. Amoeba antigen in stool was negative. A sigmoidoscopy demonstrated oedema, erythema, and erosions of mucosa in the distal half of rectum, and biopsies were taken from rectum (Fig. 1). Histopathological examination of rectum revealed mucosal congestion, lymphatic ductus ectasia, hemorrhage and necrosis but did not demonstrate neutrophilic infiltrate along with crypt abscesses and crypt distortion. Meselazine enema 4 gr was administered once a day at night. The patient's symptoms improved rapidly. She was discharged on 7th day and was free of symptoms at the follow up. Three months after meselazine enema therapy, sigmoidoscopic examination became normal. We stopped meselazine enema therapy. He was evaluated at the outpatient clinic and sigmoidoscopic 3 months later. Sigmoidoscopic examination became normal. She was free of symptoms at the follow up and the disease did not recurre.
Discussion
NSAIDS are widely used for treatment of painful conditions. These drugs may cause damage not only to the upper gastrointestinal tract but also to the small and large intestine (4,5). Colitis induced by indomethacin suppository is a rare condition as in our case. Patients with drug induced colitis often present with symptoms that can include abdominal and rectal pain, hematochezia and diarrhea as in our case. Endoscopic and histologic findings are also often nonspecific and may imitate ischemic or inflammatory colitis as in our case (4,5). In the present case, the patient was managed with meselazine enema and showed marked improvement. Previous reports have shown that colitis resolved spontaneously with conservative treatment and antibiotics. In patients with persistent diarrhoea despite drug withdrawal and treatment with cholestyramine and/or antidiarrheals, treatment with budesonide should be considered (5). We used mesalazine enema for the first time in this indication. Mesalazine might have accelated the duration of symptomatic and endoscopic relief in the present case.
In conclusion, indomethacin suppository may cause severe colitis. Fortunately, that adverse event is reversible and improve with mesalazine enema treatment.
Adnan Tas1 and Hacer Celik2
1Departments of Gastroenterology and 2Pulmonary. Osmaniye Public Hospital. Osmaniye, Turkey
References
1. Taş A, Aydn YY, Arhan M, Köklü S. Hydrogen peroxide exposure mimicking ulcerative proctitis. Dig Liver Dis 2011;43:331-2. [ Links ]
2. Slavin RE, Dias MA, Saral R. Cytosine arabinoside-induced gastrointestinal toxic alterations in sequential chemotherapeutic protocols. Cancer 1978;42:1747-59. [ Links ]
3. Gaïes E, Ouanes L, Trabelsi S, Salouage I, Klouz A, Daghfous R, et al. Drug induced colitis: Review article. Therapie 2010;65:249-53. [ Links ]
4. Geramizadeh B, Taghavi A, Banan B. Clinical, endoscopic and pathologic spectrum of non-steroidal anti-inflammatory drug-induced colitis. Indian J Gastroenterol 2009;28:150-3. [ Links ]
5. Casella G, Villanacci V, Fisogni S, Cambareri AR, Di Bella C, Corazzi N, et al. Colonic left-side increase of eosinophils: A clue to drug-related colitis in adults. Aliment Pharmacol Ther 2009;29:535-41. [ Links ]