My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 n.8 Madrid Sep. 2013
https://dx.doi.org/10.4321/S1130-01082013000800014
LETTERS TO THE EDITOR
Schwannoma in descending colon: Presentation of a neoplasm in a rare location
Schwannoma en colon descendente: presentación de una neoplasia en rara localización
Key words: Schwannoma. Colon. Diagnosis. Gastrointestinal neoplasms.
Palabras clave: Schwannoma. Colon. Diagnóstico. Neoplasia gastrointestinal.
Dear Editor,
Schwannomas of the gastrointestinal tract are uncommon tumours originating in the cells of Schwann of the peripheral nerves and accounting for 2-6 % of all mesenchymal tumours. They usually appear in the stomach or small intestine and less frequently in the colon.
Case report
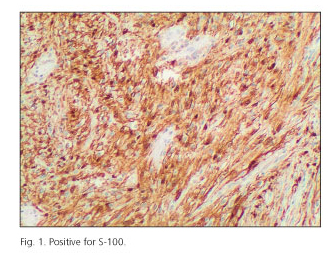
We present a 67-year-old male in whom a screening colonoscopy revealed an ulcerated polypoid lesion 35 cm from the anal margin. The biopsy was unspecific. CT and virtual colonography showed a 4.5 x 3.6 x 3.7 cm polypoid mass in the left colon with regional adenopathies but no distant metastases. The patient was admitted to the emergency department for rectorrhage and abdominal pain. Ultrasonography showed a colico-colic invagination caused by the polypoid mass. The patient underwent a midline laparotomy, which revealed an invagination in the descending colon, but no infiltration or distant dissemination. A segmental colectomy was performed with a mechanical side-to-side anastomosis. The patient evolved favourably. The anatomopathological study informed of a well-circumscribed yellowish-white submucosal tumour made up of spindle cells forming palisades, an intratumoural lymphoid infiltrate with peripheral nodules, and low mitotic activity. Immunohistochemical tests were positive for S-100 and CD68 but there was no reactivity for CD117, CD34, actin and CD10 (Fig. 1). The definitive diagnosis was schwannoma of the colon. No recurrence has been observed in 3 years of follow-up.
Discussion
Schwannomas are common in subjects with von Recklinghausen's disease (1,2). The colon is a rare location, and when they appear they are most often found in the caecum, followed by the sigmoid colon, transverse colon, descending colon (as in our case) and finally the rectum. They are benign neoplasms that rarely degenerate (3). They usually present as a polyp which may ulcerate the mucosa (4,5) and lead to unspecific symptoms such as abdominal pain with rectal bleeding, defecation disorders, colonic obstruction or invagination, as in our patient (6,7). Imaging tests are unspecific. CT shows a well-defined homogeneous mural mass and differentiates them from GISTs (gastrointestinal stromal tumours), which are heterogeneous masses (8). On most occasions diagnosis is not established from the biopsy, but from the surgical specimen (9).
Macroscopically they are well-circumscribed yellowish-white lesions. Microscopically they are arranged in a pattern of intertwined bundles surrounded by an infiltrate of lymphoid cells with germinal centres and small foci of cellular atypia with low mitotic activity (10). An immunohistochemical study is very useful for a differential diagnosis with other lesions such as GISTs, GANTs (a variant of GISTs derived from the autonomic nerves), leiomyomas or leiomyosarcomas, which can show a more aggressive behaviour (11). Schwannomas usually express a positive reaction for S-100, vimentin and GFAP, but no reactivity for the transmembrane receptor tyrosine kinase known as c-KIT or CD117, the precursor cell antigen of the haematopoyetic system CD34, actin or cytokeratins, which do appear more typically in GISTs, GANTs or muscle tumours (12,13). After diagnosis, the options are to perform a polypectomy or segmental colectomy with free margins, due to the low risk of malignancy (14,15). Because of their benignity these patients have a good prognosis. Recurrence or the presence of metastases is very rare.
Article funded in part by the FFIS (Foundation for Health Research and Training in the Region of Murcia, Spain, Group FFIS-008), the University of Murcia (Spain) and IMIB (Murcia Biomedical Research Institute).
María Ángeles Verdú-Fernández, María Pilar Guillén-Paredes, María Luisa García-García
José Andrés García-Marín, Enrique Pellicer-Franco and José Luis Aguayo-Albasini
Department of General and Digestive Surgery
Hospital General Universitario Morales Meseguer
Campus de Excelencia Internacional "Mare Nostrum"
Universidad de Murcia. Murcia, Spain
References
1. Daimaru Y, Kido H, Hashimoto H, Enjoji M. Benign schwannoma of the gastrointestinal tract: A clinicopathologic and immunohistochemical study. Hum Pathol 1988;19:257-64. [ Links ]
2. Miettinen M, Shekitka KM, Sobin LH. Schwannomas in the colon and rectum: A clinicopathologic and immunohistochemical study of 20 cases. Am J Surg Pathol 2001;25:846-55. [ Links ]
3. Nonose R, Lahan AY, Santos Valenciano J, Martínez CA. Schwannoma of the Colon. Case Rep Gastroenterol 2009;3:293-9. [ Links ]
4. Kwon MS, Lee SS, Ahn GH. Schwannomas of the gastrointestinal tract: Clinicopathological features of 12 cases including a case of esophageal tumor compared with those of gastrointestinal stromal tumors and leiomyomas of the gastrointestinal tract. Pathol Res Pract 2002;198:605-13. [ Links ]
5. Tanaka T, Ishihara Y, Takabayashi N, Kobayashi R, Hiramatsu T, Kuriki K. Gastrointestinal: Asymptomatic colonic schwannoma in an elderly woman; a rare case. J Gastroenterol Hepatol 2011;26:1339. [ Links ]
6. Martínez JJ, Vicente JJ, García B, Pérez M, González R. Manifestación atípica de una lesión infrecuente: Vídeo y ecoendoscopia de un schwanoma gástrico. Rev Esp Enferm Dig 2005;97:844-5. [ Links ]
7. Kim HJ, Kim CH, Lim SW, Huh JW, Kim YJ, Kim HR. Schwannoma of ascending colon treated by laparoscopic right hemicolectomy. World J Surg Oncol 2012;10:81. [ Links ]
8. Levy AD, Quiles AM, Miettinen M, Sobin LH. Gastrointestinal schwannomas: CT features with clinicopathologic correlation. AJR Am J Roentgenol 2005;184:797-802. [ Links ]
9. Yoon W, Paulson K, Mazzara P, Nagori S, Barawi M, Berri R. Gastric schwannoma: A rare but important differential diagnosis of a gastric submucosal mass. Case Rep Surg 2012;2012:280982. [ Links ]
10. Hsu KF, Lin CT, Wu CC, Hsiao CW, Lee TY, Mai CM, et al. Schwannoma of the rectum: report of a case and review of the literature. Rev Esp Enferm Dig 2010;102:289-91. [ Links ]
11. Tanoue Y, Tanaka N, Nagai M, Suzuki Y. Benign pigmented schwannoma of the great omentum: Report of a rare case and review of the literature. Case Rep Gastroenterol 2009; 3:222-9. [ Links ]
12. Torres FJ, Fernández P, Del Álamo C, Martínez A, Moreno S. Schwannoma quístico de colon. Presentación de un caso. Rev Esp Patol 2009;42:143-6. [ Links ]
13. Hou YY, Tan YS, Xu JF, Wang XN, Lu SH, Ji Y, Wang J, Zhu XZ. Schwannoma of the gastrointestinal tract: A clinicopathological, immunohistochemical and ultrastructural study of 33 cases. Histopathology 2006;48:536-45. [ Links ]
14. Park KJ, Kim KH, Roh YH, Kim SH, Lee JH, Rha SH, et al. Isolated primary schwannoma arising on the colon: Report of two cases and review of the literature. J Korean Surg Soc 2011;80:367-72. [ Links ]
15. Watanabe A, Ojima H, Suzuki S, Mochida Y, Hirayama I, Hosouchi Y, et al. An individual with gastric schwannoma with pathologically malignant potential surviving two years after laparoscopy-assisted partial gastrectomy. Case Rep Gastroenterol 2011;5:502-7. [ Links ]











 text in
text in