Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.105 no.10 Madrid nov./dic. 2013
https://dx.doi.org/10.4321/S1130-01082013001000012
LETTERS TO THE EDITOR
Venous intestinal ischemia due to G20210A mutation of prothrombin gene
Isquemia intestinal de origen venoso consecuencia de la mutación G20210A del gen de la protrombina
Key words: Intestinal ischemia. Prothrombin mutation. Procoagulant conditions.
Palabras clave: Isquemia intestinal. Mutación protrombina. Estados procoagulantes.
Dear Editor,
Venous intestinal ischemia is a relatively rare disease, which has some predisposing factor up to 80 % of cases. These factors may be temporary or permanent. Cancer, immobilization, trauma, intraabdominal infections, or oral contraceptives are temporary factors. Paroxysmal nocturnal hemoglobinuria and hypercoagulability states as factor V Leiden, G20210A mutation in prothrombin gene, C677T methylene-tetrahydrofolate reductase, protein C and S deficiency, antithrombine III deficiency or antiphospholipid syndrome are permanent factors. We report a case diagnosed and treated in our center.
Case report
We report a 77-years-old woman, BMI 28, who developed a bilateral submassive pulmonary thromboembolism after surgery for acute cholecystitis. She was treated with acenocumarol. After the corresponding study, it was found that the patient was heterozygous carrier of G20210A polymorphism of prothrombin gene.
Four months later, the patient was admitted to our emergency room. The patient complained of abdominal pain, bilious vomiting and melena. Anticoagulation was removed 40 days before. On physical examination, the patient was hemodynamically stable, with diffuse abdominal pain but without any signs of peritoneal irritation. No palpable masses or organ enlargement.
Blood count, biochemistry and coagulation show a compensated metabolic acidosis. CT-angiogram was performed for suspected intestinal ischemia. It showed a thrombus partially occluding the ileocolic vein, superior mesenteric vein and all distal branches. It also showed thickening and congestion of the small bowel loops, being preserved distal ileal loops.
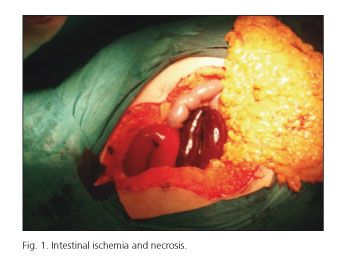
An urgent median laparotomy was performed. We found serohemorrhagic liquid (1,000 cc) and necrosis of jejunum and ileum, 20 to 25 cm from the ligament of Treitz to the ileocecal valve (Fig. 1). Rest of the abdominal cavity apparently normal. Resection of affected bowel and terminal anastomosis was performed.
Postoperatively the patient progressed satisfactorily. She was reviewed by hematology and was discharged on the eight day.
Discussion
G20210 polymorphism in the prothrombin gene is a point mutation at nucleotide at position 20210 (chromosome 11p11-q12). It is a transposition between guanine and adenosine that modify transcription of messenger RNA and raises plasma prothrombin levels.
Overall, the prevalence is estimated between 0.7 and 6.5 % (1). It is much more common in Caucasians of southern Europe (2). More specifically in Spain is the highest prevalence figure. No sex differences have been found.
The mutation alone increases almost three times the risk of deep vein thrombosis and is present in 40 % of cases of thrombosis of the splenoportal axis (3).
Lucio Amitrano (5) found among his patients diagnosed with venous intestinal ischemia that three out of four had a hypercoagulable state. C667T mutation methylene-tetrahydrofolate reductase enzyme was responsible for 50 % of cases. G20210A mutation of prothrombin was responsible of 25 % of cases and factor V Leiden in another 25 %.
Mortality of venous intestinal ischemia is estimated at around 27 % (4). The gold standard for diagnosis is abdominal CT with intravenous contrast, although in some situations a venous Doppler ultrasound may be enough.
Around 50 % of patients with venous intestinal ischemia require urgent intervention and in most cases takes any kind of intestinal resection (5). All patients should receive lifelong anticoagulation except absolute contraindication.
Some authors (6,7) suggest a second look 24 hours later the first surgery, especially in patients with intestinal viability doubt. It may be useful to identify cases where there has been no resection in the first surgery and it is needed in the second one. It is also used to check the viability of the anastomosis performed in the first surgery.
We consider it important to emphasize the great importance of anticoagulation to prevent thrombotic events in this type of patient.
José Andrés García-Marín, Ramón Lirón-Ruiz,
Jose Antonio Torralba Martínez, Juan Gervasio Martín-Lorenzo
y José Luis Aguayo-Albasini
Deparment of General and Digestive Surgery.
Hospital Universitario Morales Meseguer. Murcia, Spain
References
1. Souto JC, Coll I, Llobet D, del Río E, Oliver A, Mateo J, et al. The prothrombin 20210A allele is the most prevalent genetic risk factor for venous thromboembolism in the Spanish population. Thromb Haemost 1998;80:336-9. [ Links ]
2. Muñoz S, Cubo P, González Castillo J, Nuevo JA, García Lamberechts EJ, Sanz A. Superior mesenteric venous thrombosis: A retrospective study of thirteen cases Rev Esp Enferm Dig 2004;96:385-90,390-4. [ Links ]
3. Frutos Bernal MD, Fernández Hernández JA, Carrasco Prats M, Soria Cogollos T, Luján Mompeán JA, Hernández Agüera Q, et al. Trombosis venosa portoesplenomesaraica secundaria a mutación del gen de la protrombina. Gastroenterol Hepatol 2005;28:329-32. [ Links ]
4. Zivelin A, Rosenberg N, Faier S, Kornbrot N, Peretz H, Mannhalter C, et al. A single genetic origin for the common prothrombotic G20210A polymorphism in the prothrombin gene. Blood 1998;92:1119-24. [ Links ]
5. Amitrano L, Brancaccio V, Guadasciona MA, Margaglione M, Iannaccone L, D'Andrea G, et al. High prevalence of thrombophilic genotypes in patients with acute mesenteric vein thrombosis. Am J Gastroenterol 2001;96:146-9. [ Links ]
6. Margaglione M, D'Andrea G, Colaizzo G, Del Popolo A, Brancaccio V, Ciampa A, et al. Coexistence of factor V Leiden and factor II G20210 mutations and recurrent venous thromboembolism. Thromb Haemost 1999;82:1583-7. [ Links ]
7. Lindblad B, Hakansson HO. The rationale for "second-look operation" in mesenteric vessel occlusion with uncertain intestinal viability at primary surgery. Acta Chir Scand 1987;153:531-3. [ Links ]











 texto en
texto en