Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.2 Madrid feb. 2014
https://dx.doi.org/10.4321/S1130-01082014000200008
PICTURES IN DIGESTIVE PATHOLOGY
Diffuse colon opacifications due to lanthanum carbonate
Imágenes intraluminales colónicas por carbonato de lantano
Amaya Jimeno-Almazán, Rafael Vilaplana-García and María Contreras-Padilla
Department of Internal Medicine. Hospital Santa Lucía. Cartagena, Murcia. Spain
Introduction
Lanthanum carbonate is a free calcium and aluminum phosphate binder used in chronic renal failure that may produce a characteristic radiopaque image in the colon by intraluminal deposits that must be known. This can help the differential diagnosis in cases of abdominal pain of unknown origin in patients receiving this treatment.
Case report
We report a case of a 68-year-old patient with multiple vascular risk factors (hypertension, diabetes mellitus, dyslipidemia and hyperuricemia and a former smoker) and chronic kidney disease of mixed diabetic-hypertensive origin in hemodialysis program since 2002. As complications associated with his disease presents hyperphosphatemia, hypocalcemia and secondary hyperparathyroidism. His medications included: Cinacalcet, resincalcio and calcium acetate with lanthanum carbonate. The patient also had chronic ischemic heart disease and has had an ischemic cerebral stroke in 2006.
On the day of admission, after the meal, he has a sharp and intense unirradiated pain located in mesogastrium accompanied by vomiting and several liquid stools without blood or mucous. He had no fever or other symptoms. Physical examination was unremarkable. In the emergency department, a blood test was performed including biochemistry and blood count.
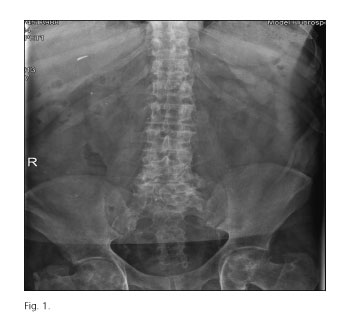
The relevant abnormal laboratory test results were: C-reactive protein 2.4 mg/dL, procalcitonin (PCT) 1.55 ng/mL, glucose 209 mg/dL, urea 73 mg/dL and creatinine 6.0 mg/dL. The following values were within normal limits: Blood count, aspartate aminotransferase, alanine aminotransferase, bilirubin, amylase, and serum electrolytes. In addition, a plain abdominal X ray (Fig. 1) and an abdominal ultrasound revealed no significant findings.
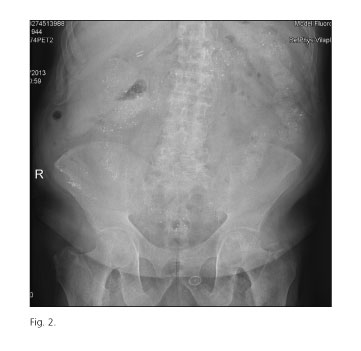
He was admitted to the Internal Medicine ward with a presumptive diagnosis of ischemic colitis. Nothing by mount and symptomatic treatment was established, without antibiotics, with complete resolution of symptoms within 48 hours. Complete normalization of analytical parameters was confirmed, including biochemistry, liver function, PCT (0.74 ng/mL), and complete blood count -WBC 9.70 (standard formula)-, so it does not consider the need for further tests (CT abdomen and/or colonoscopy). A new X-ray was performed prior to discharge (Fig. 2). Multiple radiopaque images throughout the course of the colon similar in appearance to contrast and in relation to lanthanum carbonate are appreciated. Outpatient medications were continued, so they have no direct relation to the current status. A final diagnosis of infectious enterocolitis, possibly viral, was done and the patient was discharged on the fourth day.
Discussion
It is a high-risk patient with multisystem micro and macrovascular involvement in relation to the classical vascular risk factors, so it seems fitting that the initial diagnosis was that of ischemic colitis. However, the initial nonspecific clinical presentation, the absence of clinical signs of severity, spontaneous recovery without any specific intervention in the first 24 hours and analytical normality make this diagnosis unlikely. Another possibility was a bacterial active infection of intestinal origin. PCR and PCT oriented the possibility of infection, but were below the threshold of higher sensitivity and specificity (PCT 2 ng/mL and PCR 5 mg/dL) to consider septic origin. In the absence of antibiotic treatment these two parameters were normalized. Under these circumstances compatible images with lanthanum carbonate are identified in the plain abdominal radiography. The main adverse event of this drug is tolerability from gastrointestinal standpoint. However, in studies of drug safety, it is found that it is unlikely that these force it withdrawal (1,2). In our case, the patient recovered from the symptoms that led to his admission while maintaining lanthanum carbonate treatment; consequently they can not be attributed directly to their consumption and we finally consider that the radiological findings were accidental. Therefore, we believe that all symptoms were likely related to an acute enterocolitis of unknown etiology and so it was self-limiting.
Lanthanum carbonate is a free of calcium and aluminum binder, used in the control of hyperphosphatemia in patients with chronic renal failure undergoing dialysis. It is not metabolized and is excreted almost entirely in the feces. It has the advantage over other chelators that does not increase the calcium and may be involved in reversing the calcium vascular deposits (3). The most frequent adverse reactions are gastrointestinal manifestations, such as abdominal pain, constipation, diarrhea, dyspepsia, flatulence, nausea, and vomiting. These are reduced when ingested with food and generally disappear over time. In the American version of the technical information for the drug, is noted the possibility of the appearance of radiopaque images in abdominal plain radiography (4). This phenomenon is not constant; therefore, it can be found normal radiographs in nearly half of patients depending on the time of the taking, the dosage, and the presence of pre-existing disease (eg, diverticulosis) (4-6). It is not exactly known how lanthanum carbonate behaves and how it deposits in a intestinal reservoir (4).
In conclusion, physicians should be aware of the peculiarity of the images to avoid misinterpretation. Lanthanum carbonate also should be included in the differential diagnosis of abdominal pain of unknown cause in patients who start taking the drug.
References
1. Yamada S, Yoshida H, Taniguchi M, Tanaka S, Eriguchi M, Tsuruya K, et al. Effectiviness of lanthanum carbonate treatment used in combination with other phosphate binders in peritoneal diálisis patients. Inter Med 2012;51:2097-104. [ Links ]
2. Shigematsu T. Lanthanum Carbonate Research Group. One year efficacy and safety of lanthanum carbonate for hiperphosphatemia in Japanese chronix kidney disease patients undergoing hemodialysis. Ther Apher Dial 2010;14:12-9. [ Links ]
3. Pérez Alonso L, Moreno Polanco MA. Carbonato de lantano: una explicación novedosa de una imagen radiológica habitual. Rev Clin Esp 2011;211:60-8. [ Links ]
4. Díez Ojeda B, Medrano Martínez S, Alonso Álvarez MA. Imagen radiológica del carbonato de lantano. Nefrología 2010;30:263-4. [ Links ]
5. Cerny S, Kunzendorf U. Radiographic apperance of lanthanum. N Engl J Med 2006;355:1160. [ Links ]
6. Vrigneaud L, Lefèbvre D, Daem AO, Lemaitre V. Radiographic characteristics of lanthanum carbonate absorption. Nephrol Ther 2008;4:111-13. [ Links ]











 texto en
texto en